|
Not
all that is red, itchy, and scaly on the feet or groin is fungal. Be
sure to consider other causes such as contact dermatitis, eczema, and
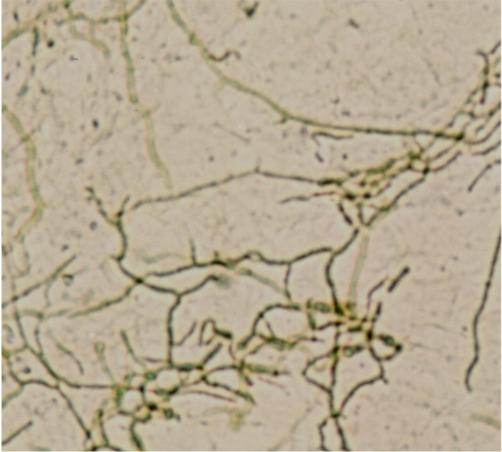
bacteria. Take a KOH preparation from the scaly advancing border of a
groin rash or from scaling on the feet adjacent to (but not within) an
area of maceration, or the roof of a vesicle on the foot to confirm
the diagnosis. Branching hyphae should be visible (figure 9).
Fungus lives where it is wet,
warm, and dark. The groin and foot are ideal locations for growing
fungus. Control of the milieu is important to controlling tinea.
Potent medications are not a substitute for simple preventative
measures to make the fungus less welcome.
Web
spaces and groins should be thoroughly dried after gently showering,
followed by applying simple antifungal powders containing tolnaftate
or miconazole. Shoes should fit well and socks should be frequently
changed. If possible, two sets of routine footwear should be
maintained; one for odd days, one for even days. In this fashion, the
shoes will dry out on the "off day". Sweating of the feet can be
treated with antiperspirants such as aluminum chloride solution (e.g.
DrySol, Xerac AC, or Certain Dri) applied at bedtime. Boxer shorts
are preferable to briefs... especially if wearing BDUs.
If
tinea develops, remember to use the preventive steps outlined
previously in addition to the treatment plan. These actions will make
the treatment much more effective, provide more rapid relief, and
allow for better results over the long run.
Wet, very macerated tinea of
the web spaces is best treated with antifungal lotions such as
miconazole or clotrimazole after astringent compresses with Burow's
solution (see Impetigo above) or dilute vinegar. These areas are
frequently overgrown with a potpourri of gram negative bacteria
(figure 10). The concurrent use of a drug such as oral ciprofloxacin
accelerates recovery.
Typical web space tinea is
treated with a cream or solution vehicle antifungal drug. Miconazole
or clotrimazole are effective. Nizoral, Spectazole, Naftin, or
Lamasil cream is also effective but quite a bit more expensive. At
least 3 weeks of treatment are required.
Chronic, hyperkeratotic, cracked and
peeling "moccasin foot" tinea is treated with keratolytics such as
Whitfield's ointment, 10% salicylic acid in petrolatum or 12% ammonium
lactate lotion (Lachydrin). Antifungal creams are also effective but
are quite a bit more expensive. Localized vesicular plantar tinea can
be treated with cream. Extensive vesicular tinea of the feet requires
the addition of astringent soaks (see above) and strong consideration
of oral antifungal therapy (see below).
Not all itchy perineums and groins are
caused by tinea. Strongly consider the diagnosis of Candida if
"satellite pustules" and extensive maceration are present, especially
in females. The differential diagnosis frequently includes contact
dermatitis (occupational and non-occupational), seborrheic dermatitis,
and psoriasis. Take a history and look for diagnostic hints.
Remember, in temperate climates Tinea and Candida rarely involve the
scrotum.
Contact dermatitis as an overlay to
another diagnosis on the genital and crural skin occurs more often
than is appreciated. Patients with itchy groins are desperate to stop
the itch and will try anything topical; topical benzocaine,
deodorants, rubbing alcohol, strong antibacterial soaps, and Ben Gay
to name a few. Insist that all applications be ceased except the ones
that you prescribe. Wet and weepy groins need astringent solution
compresses and ventilation to facilitate drying.
If the diagnosis is tinea cruris, begin
with twice a day antifungal cream once if the area is not weeping.
Treat for at least 3 weeks. Remember that nystatin powder, cream or
lotion, while effective for Candida, will not work against the
dermatophyte fungi which cause tinea. If the tinea is very macerated,
strongly consider using oral antifungal therapy (see below) as well as
astringent solution compresses.
The diagnosis of Tinea of the nails (tinea unguium)
needs to be confirmed before you even consider treatment. Not all distorted
nails are due to fungal infection. If you are not sure of the diagnosis,
refer to dermatology.
Tinea unguium is not worth treating and will only
rarely be permanently cured. While a period of remission can usually be
achieved, the fungus usually returns within 1-2 years. It is frequently
associated with tinea pedis in middle aged or older males who have some
immunologic anergy to the organism (Trichophyton rubrum).
Topical treatment alone will not work. The use of
oral therapy (e.g. griseofulvin, itraconazole, terbenifine) therapy is
frequently ineffective, expensive, and risks some side effects and drug
interactions (especially itraconazole). Because this condition is prone to
recurrence carefully advise the patient about the various treatment regimens
and the realistic potential for an unsatisfactory result.
Written and revised by CAPT Dennis
A. Vidmar, MC, USN, Department of Military and Emergency
Medicine, and Department of Dermatology, Uniformed Services University
of the Health Sciences, Bethesda, MD (1999).
Additional images provided by CAPT Vidmar in
June, 2000, subsequent to the initial publication of this manual.
|