|
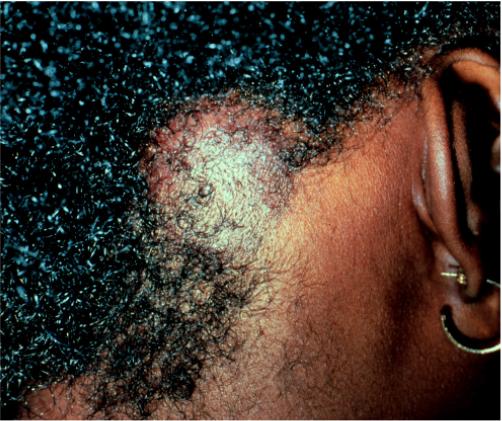
Tinea capitis is classically
thought to be a pediatric condition. However, it does occur in the
active duty age group, especially black males. The most common cause
of tinea capitis in the 1990s is Trichophyton tonsurans.
Trichophyton tonsurans
infection of the scalp can produce a variable clinical picture.
Asymptomatic scaly patches containing tiny black dots with minimal
hair loss frequently confused with Alopecia Areata is the most
frequent presentation (figure 11) although large, boggy inflamed
plaques sometimes occur (figure 12). A Wood's light is of no use to
diagnose Trichophyton tonsurans because this organism does not
fluoresce.
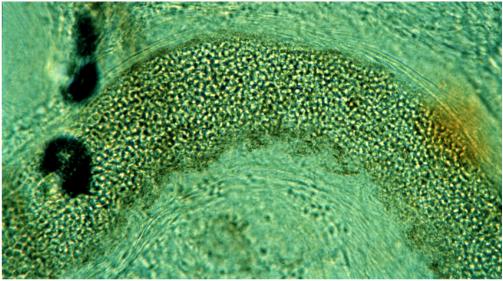
Potassium hydroxide scrapings
from the scalp should not be taken from the scale. Instead, they
should include the broken fragments of hair or the tiny black dots.
Use the tip of an 18-g needle. A curette will function. Be sure to
let the preparation digest for several minutes (after gently heating)
before viewing.
Instead of looking for
branching hyphae, look for tiny athrospores (sometimes in chains)
within and outside of the hair shaft fragments (figure 13).
Therapy of tinea capitis
involves systemic antifungals (see below). Topical therapy alone is
inadequate, it will not adequately penetrate the hair follicles. The
use of an antifungal shampoo such as Selsun, Nizoral, or Head and
Shoulders is good adjunctive therapy and will make your patient much
less infectious to his/her shipmates. Griseofulvin is still the drug
of choice. Oral treatment for at least 10 weeks is necessary.
(c) Oral Antifungal
Therapy
The use of oral
antifungal therapy is frequently misunderstood by the primary care
provider. For now, griseofulvin is the drug of choice although this
may change in the next year or two. The newer generation of oral
antifungals is quite costly and is frequently unavailable to deployed
units.
Griseofulvin
Griseofulvin is a
reasonably safe and effective drug in healthy patients if properly
used. Not all griseofulvin preparations are the same. The
bioavailability and doses of micro-size and ultra micro- size forms of
griseofulvin are quite different. Follow the PDR recommendations for
dosing. One exception however, is the need to use the "upper end" of
the dosing scales for tinea capitis.
Gastrointestinal side
effects and headache are the most frequent problems with griseofulvin.
These problems can usually be avoided if the drug is given with a
meal, especially with some lipid. A piece of toast with margarine or
oil and vinegar on a salad will provide sufficient fat. Bacon and
eggs are not necessary. Phototoxicity is unusual but reported.
Unlike antibacterial
agents, griseofulvin works quite slowly. The deposition of the drug
in newly keratinizing epithelium allows it to work. This takes time
so be patient. Pretreatment liver function tests repeated every month
or two combined with a good follow up monthly will prevent significant
hepatotoxicity. Be aware of the interactions with coumadin and do not
prescribe for patients with porphyria.
Ketoconazole
This oral form of this
medication is of limited use for treating tinea. This is best
reserved for selected patients with candida or tinea versicolor.
Itraconazole (Sporanox)
This drug is very
expensive. The use of "pulse" therapy for the treatment of the nails
(tinea unguium) is equally effective as daily therapy in most
patients. Use 200 mg twice a day (with food) for 7 consecutive days
per month repeated for 3 or 4 months. Liver function tests are usually
not needed for healthy patients using this "pulse" regimen. The list
of drug-drug interactions is very long for this medication. Check the
PDR for details.
Tebenafine (Lamasil)
This medication is also very
expensive. However, it does not have the long list of drug
interactions as itraconazole. The dose is 250 mg daily for 3-4
months. Follow the PDR concerning patient monitoring. |