|
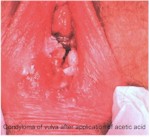
Clinical Warts Condyloma
acuminata, (venereal warts) are caused by a virus known as "Human
Papilloma Virus" (HPV).
There are two categories of warts, clinical and subclinical.
Clinical warts appear as tiny, cauliflower-like, raised lesions around
the opening of the vagina or inside the vagina. These lesions appear
flesh-colored or white, are not tender and have a firm to hard
consistency. If they are on the outside of the vagina or vulva, they
are generally symptomatic, causing itching, burning, and an
uncomfortable sensation during intercourse. If they are inside the
vagina, they generally cause no symptoms.
|

Subclinical Warts
The second category, subclinical warts, are invisible to the naked
eye, are flat and colorless. They usually do not cause symptoms,
although they may cause similar symptoms to the raised warts. These
subclinical warts can be visualized if the skin is first soaked for
2-3 minutes with vinegar (3-4% acetic acid) and then viewed under
magnification (4-10X) using a green or blue (red-free) light source.
Venereal warts are not dangerous and have virtually no malignant
potential. Clinical warts may be a nuisance and so are usually
treated. Subclinical warts are usually not treated since they are not
a nuisance (most people with subclinical warts are unaware of their
presence).
Treatment
Treatment consists of removal of the wart. This can be accomplished
in any number of ways, some more painful than others:
Apply a small amount of bichloracetic acid (80-90%) directly to the
wart, taking care to avoid spreading the acid onto the normal
surrounding skin. For larger lesions, use a cotton-tipped applicator
dipped in the acid. For smaller lesions, use the "stick" end of the
cotton-tipped applicator. Apply enough acid (very tiny amounts) to
cause the lesion to turn white, but not so much that it runs down onto
the normal surrounding skin. No anesthetic is necessary. The patient
may feel nothing, some slight tingling, or a minor stinging. After a
minute or two, rinse the skin with warm water to dilute any remaining
acid and prevent it from coming into contact with the surrounding
skin.
Try to use less acid than you think will be effective since the
patient would rather return for a second, third or fourth treatment
than recover from a serious acid burn of the vulva. Don't use acid
inside the vagina or on the cervix.
Cryosurgery can effectively remove warts. Freezing the
wart with any convenient tool (liquid nitrogen, cryosurgical probe,
etc.) can be done without anesthetic and results in sloughing of the
wart in a week or two. Be careful not to freeze normal skin. Two
freeze-thaw cycles usually work better than a single freeze-thaw
cycle.
Cryosurgery should not be done inside the vagina or on
the cervix unless you have been specially trained to do this as damage
to other structures can occur.
Podophyllum resin can be applied directly to the wart, followed by
washing off the residual podophyllin in 3-6 hours. This effective
approach runs the risk of podophyllin toxicity. This is a minor issue
if the wart is very small and you use tiny quantities of podophyllin.
If you use large amounts, or apply it inside the vagina, toxicity is a
real issue.
Don't apply large amounts of podophyllin and don't
apply any inside the vagina or on the cervix.
Under anesthetic, warts can be surgically removed,
burned, or electrocuted, but such methods are usually unnecessary for
the typical small wart(s).
If untreated, many warts will gradually resolve and
disappear spontaneously, but this may require many months or years.
Remember that in treating the warts, you are actually
destroying the patient's skin which has responded in a strange and
annoying way to the presence of the HPV. You are not getting rid of
the HPV itself.
Continue
to the PowerPoint Lecture...
From:
Operational Obstetrics & Gynecology
2nd Edition
NAVMEDPUB 6300-2C
Bureau of Medicine and Surgery
Department of the Navy |