Introduction to the Operating Room
LESSON 1: ORIENTATION
1-23
1-23. PRINCIPLES
The principles of sterile technique are applied in various ways. The principles and their application of sterile technique will be discussed in the following paragraphs.
a. All materials used as a part of the sterile field for an operation must be sterile. Certain basic items such as the linen, the instrument set, and the basins may be obtained from the supply kept in the sterile supply room. Others, such as specialized surgical instruments, may be sterilized the night before or immediately preceding the operation and taken directly from the sterilizer to the sterile operative field.
(1) Linen used in the OR is usually dyed green. This helps to reduce the glare from lights, thus reducing fatigue and eyestrain. Also, green linen helps to eliminate potential contamination from the wards, since linen in the wards is colored differently and should not be used in the OR.
(2) Moreover, linen selected for use in the OR should be checked to ensure that it is not torn, frayed, or stained, and that no holes are present in the cloth. Likewise, linen should be handled gently to prevent lint and dust from being spread about the room.
(3) Only materials known to be sterile should be used and their sterility should be maintained throughout the operative procedure.
b. Only persons who are "sterile" should touch sterile articles. "Unsterile" persons should only touch unsterile items. All supplies for the "sterile" team members (scrub, surgeon, and assistants) are provided by the circulator. The "unsterile" team member protects the sterility of items through the use of the wrappers on sterile packages (see figure 1-27).
Figure 1-27. Scrub reaching for sterile supplies.
NOTE: Observe the way in which the circulator handles the sterile wrapper.
c. Items should be considered unsterile if there is doubt about their sterility.
(1) If a sterile-appearing package is found in an area not designated for sterile storage, it is considered unsterile and must be reprocessed and resterilized or discarded.
(2) If there is doubt about the timing of a sterilizer, its contents are considered unsterile.
(3) If an "unsterile" person brushes against a sterile table, the table is considered contaminated. If a "sterile" person brushes against an unsterile table, the person's sterile gown is considered contaminated.
(4) If a sterile table or sterile items are left uncovered and unguarded, the table and items are considered unsterile.
d. "Unsterile" persons should avoid reaching over a sterile field. "Sterile" persons should avoid reaching over an unsterile area.
(1) The scrub sets basins or glasses to be filled at the edge of the sterile table opposite where he stands. The circulator stands near the edge of the table to fill them.
(2) The circulator stands at a distance from the sterile field when adjusting the light over it.
(3) A "sterile" team member turns away from the sterile field to have perspiration mopped from his brow.
(4) The scrub drapes the part of an unsterile table nearest him first.
e. Only the top surface of a draped table is considered sterile.
(1) Linen or sutures falling over the edge of the table should be discarded. The scrub should not touch the part hanging below the table level.
(2) When the circulator uncovers a sterile table, he should be careful that the edge of the sheet nearest the floor is not brought up to table level where it might contaminate the sterile contents.
(3) When the scrub drapes a table with sterile linen, he should see that the part of the linen, which drops below the table's surface is not brought up to table level again.
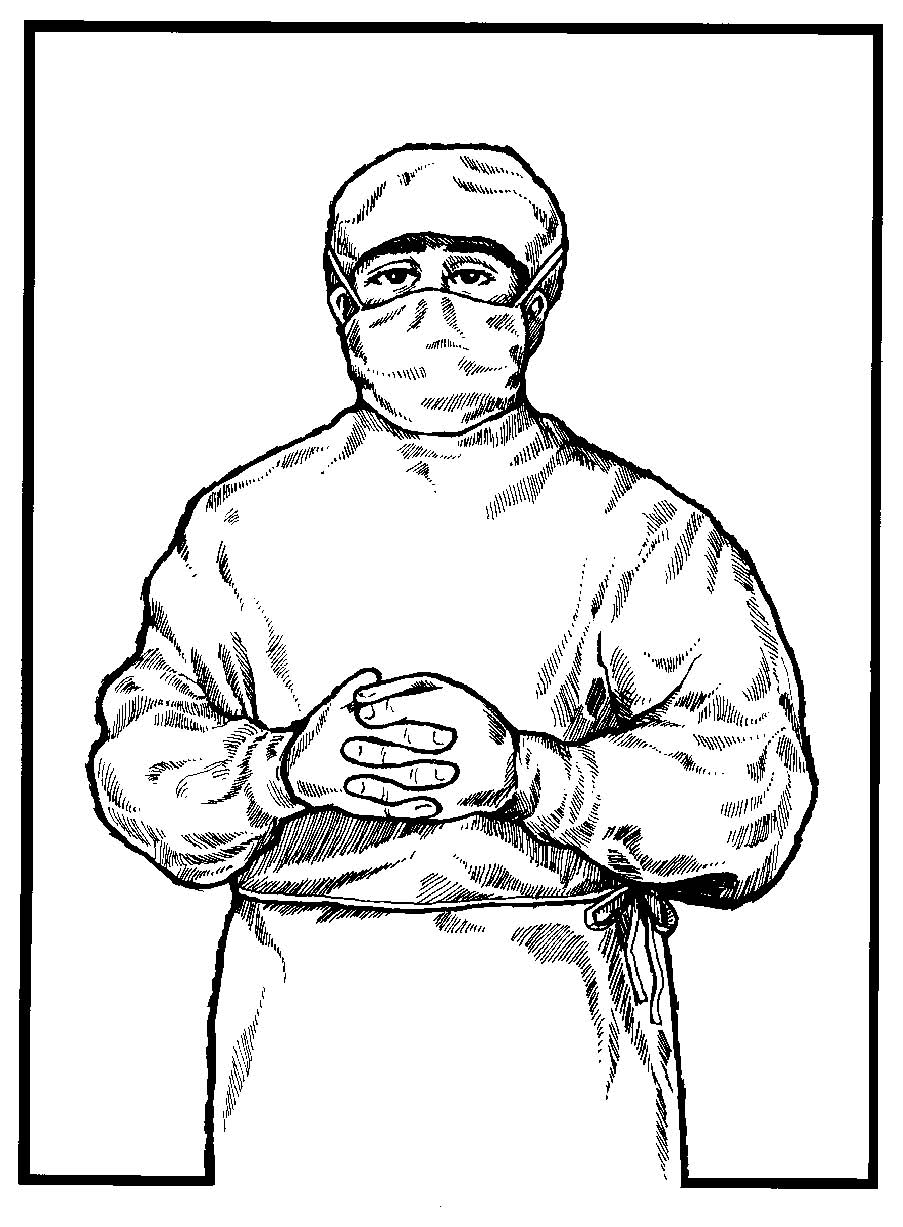
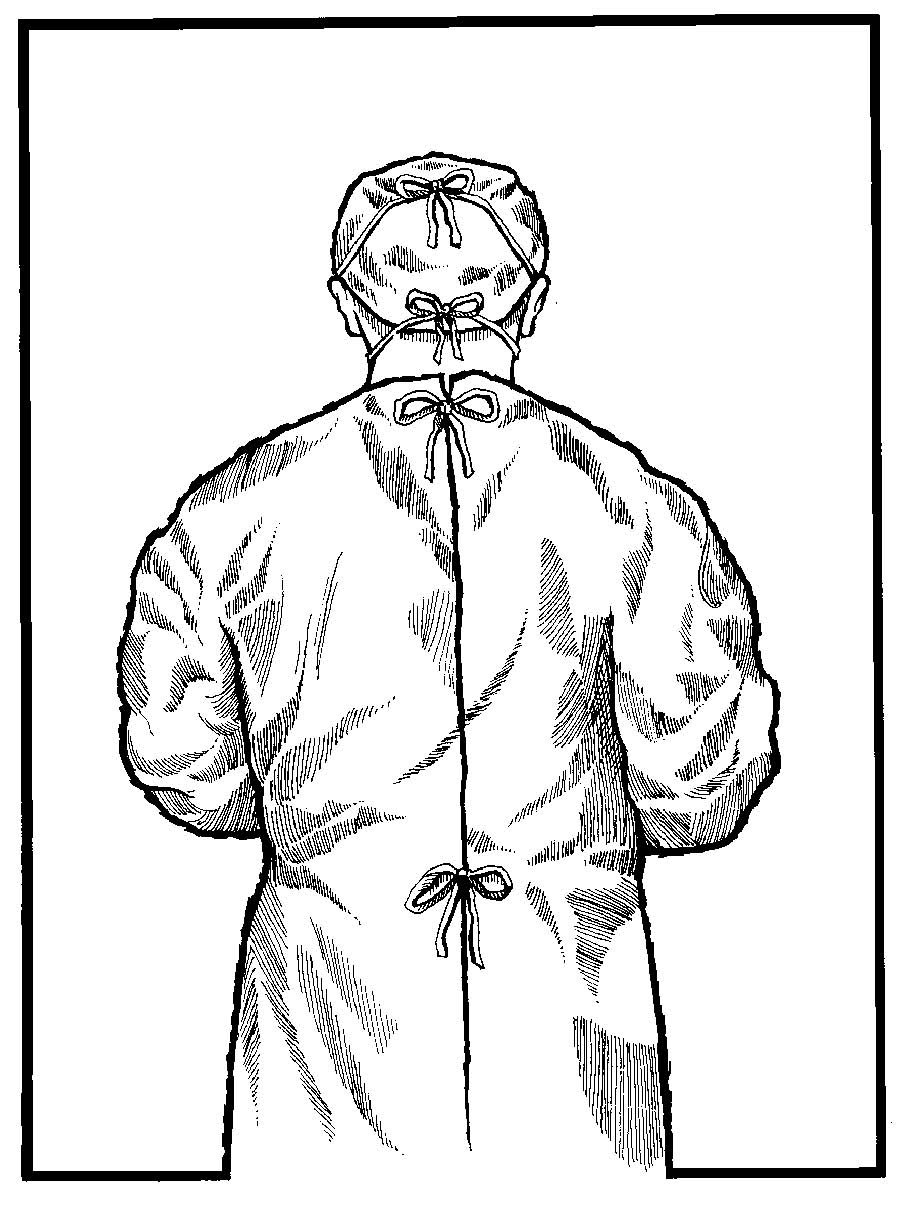
f. The parts of a surgical gown (see figures. 1-28 and 1-29) considered sterile are the sleeves (except for the axillary area) and the front from waist level to a few inches below the neck opening.
Figure 1-28. Sterile team member's attire (front view).
Figure 1-29. Sterile team member's attire (back view).
(1) A "sterile" person should keep his hands in sight and at waist level or above (see figures. 1-28 and 1-29).
(2) A "sterile" person should keep his hands away from his face and his elbows close to his sides (see figure 1-28). He should never fold his arms, since his gown may be moist with perspiration in the axillary region; thus, his gloves would be contaminated. When a "sterile" person stands on a footstool, the lower part of his gown should not brush the sterile table.
(NOTE: Common sense determines sterile parts of a gown worn by tall and short
members in relation to their waists and the tops of sterile tables.
g. The edge of a cover that encloses sterile contents is not considered sterile. Such covers include the edges of wrappers on sterile packages, the caps on solution flasks, and test-tube covers. No definite line separates the sterile from the unsterile area at the edge of the cover; therefore, the edge is considered unsterile.
(1) The scrub should lift contents from packages by reaching for them with the arm straight out and lifting the items straight up--with the elbow held high throughout the procedure (see figure. 1-27).
(2) The circulator lifts the cap from a solution flask or test tube so that the edge of the cap never touches the lip.
(NOTE: Caps are not replaced)
The entire contents are dispensed and any excess solution is discarded.
(3) When a circulator opens a package, his hands are placed under the cuff to provide a protected wide margin of safety between the inside of the sterile pack and the unsterile hands. When a sterile article that is wrapped sequentially in two wrappers with the corners folded toward the center of the article is opened, the circulator opens the corner farthest from his body first and the corner nearest his body last.
h. "Sterile" team members keep well within the sterile area. The scrub should allow a wide margin of safety when passing unsterile areas. The scrub as well as all other "sterile" team members should observe the following practices:
(1) "Sterile" team members should stand back at a safe distance from the operating table while draping the patient.
(2) "Sterile" team members should pass each other back-to-back.
(3) A "sterile" team member should turn his back to an "unsterile" person or area when passing.
(4) A "sterile" team member should face a sterile area when passing.
(5) "Sterile" team members should stay near the sterile tables when waiting for a case to begin. They should not wander about the room nor go out into the corridor.
i. "Unsterile" team members should keep away from sterile areas. "Unsterile" persons should allow a wide margin of safety when passing sterile areas and should follow the rule for passing--"unsterile" persons should face a sterile area when passing it to be sure they have not touched the area. In addition, "unsterile" persons should not go within the sterile "circle" or between two sterile fields. An unsterile team member should never crowd past a "sterile" team member.
j. "Sterile" team members should keep their contact with sterile areas to a minimum.
(1) "Sterile" team members should not lean on the sterile tables nor on the draped patient.
(2) The scrub should keep the large instrument table (back table) and the Mayo stand far enough away so that the gowns of "sterile" team members do not brush the area.
k. Sterile areas should be protected from moisture because a moist item may become contaminated. When moisture soaks through a sterile area to an unsterile one, or vice versa, a means of transporting infectious organisms to the sterile area is provided. Therefore, the OR specialist should observe the following rules of practice:
(1) Sterile packages should be laid on dry sterile areas.
(2) If any portion of a sterile package becomes damp or wet, the entire package should be either resterilized or discarded.
(3) If a sterile package falls on the floor, it is considered unsterile.
(4) Ampules wet with a bactericidal solution should be handled in such a way as to avoid wetting the sterile drape.
(5) A towel should be placed in the bottom of an instrument tray before placing the instruments in it for autoclaving. The towel will absorb the moisture and permit the tray to be set upon a sterile table after being autoclaved.
(6) Linen packages from the sterilizer should be permitted to cool before being stored on shelves. This procedure prevents packages from becoming damp from steam condensation when placed upon a cool shelf.
(7) Sterile drapes should be placed on a dry surface. Thus, time should be allowed for the prep solution used to paint the patient's skin to dry before draping is begun.
(8) During surgery, if a solution soaks through a sterile area from an unsterile one--or through an unsterile area from a sterile one, the wet area should be covered with another sterile drape.
l. Whenever microorganisms cannot be eliminated from a field, they should be kept to an irreducible minimum. Although absolute asepsis in an operative field cannot be reached, every effort is made to control sources of possible contamination (refer to (1)-(4) below).
(1) Skin. Skin cannot be sterilized. Skin normally harbors staphylococcus and other organisms; however, any agent capable of sterilizing skin will also destroy the skin. The skin of the patient as well as that of members of the "sterile" team is therefore a potential source of contamination in every operation. However, this does not remove the need for strict aseptic technique. Defenses within the patient's body will usually overcome the relatively few organisms left on the skin when the following protective measures are carried out:
(a) The patient's skin is given a shave and scrub before surgery, and is again thoroughly cleansed in the OR just prior to the incision.
(b) The skin of OR personnel is another source of contamination. They follow rigid steps in scrubbing their hands and arms, using brushes and detergents and adhering to strict technique. This is done to remove the maximum number of organisms. When drying their hands, hand towels should not touch their scrub clothes.
(c) "Sterile" team members gown and glove without touching the outside of gowns or gloves with their bare hands.
(d) All of the patient's skin area except the site of incision is covered with sterile drapes.
(e) When no longer needed, the knife used for the skin incision is placed in a basin and kept within the sterile area by the scrub.
(f) Sterile towels/materials may be used to cover the skin after the incision is made. The reason for this additional precaution is to protect the surgical wound from the waste products continually excreted by the skin, because this waste contains microorganisms. In addition, airborne organisms continuously pose a threat of contaminating the incision.
(g) If a "sterile" team member's glove is punctured during an operation, the glove is to be changed at once. If the glove is pricked by a needle or an instrument, the glove is to be changed immediately and the needle or instrument is discarded from the sterile field. Notify the circulator of the needle's whereabouts.
(h) The cap, worn on the head of team members, should completely cover the hair to prevent particles of dandruff or hair from falling on the sterile field or in the room. Refer to figures 1-28 and 1-29.
(2) Mucous membrane. Some areas cannot be scrubbed. Mucous membrane is not scrubbed since scrubbing would damage the tissue. When the site of operation is the mucous membrane of the nose, mouth, throat, or anus, the number of microorganisms present is great. However, the various parts of the body do not usually become infected by organisms that normally inhabit those parts. Even so, an effort is made to reduce the number of organisms present in an operative area and to prevent scattering the remaining ones.
(a) As much of the operative area is cleansed, as is feasible and the surrounding skin is scrubbed.
(b) When the specialist is scrubbing the patient's skin, the surgeon makes an effort to use a sponge only once for mopping an area. Once he removes the sponge from contact with the skin, he discards the sponge into a kick bucket.
(3) Infected areas. Infected areas are grossly contaminated. The "sterile" team members should avoid scattering the contamination. In addition, cases involving infected areas require a special cleanup procedure following the operation.
(4) Air. The air is contaminated by dust and droplets.
(a) Team members are required to wear a mask covering the nose and mouth (refer to figure 1-28). A mask is worn not only during an operative procedure, but also any time personnel enter the OR. The mask must cover the mouth and nose entirely and be tied securely to prevent venting. The strings should not be crossed when tied because the sides of the masks will gap. A pliable metal strip is inserted in the top hem of most masks to provide a firm contour fit over the bridge of the nose. This strip also helps prevent fogging of eyeglasses. Air should pass only through the filtering system of the mask. Masks should be either on or either off. They should not be saved from one operation to the next by allowing them to hang around the neck or by tucking them into a pocket. Bacteria that have been filtered by the mask will become dry and airborne if the mask is worn necklace fashion. By touching only the strings when removing the mask, contamination of the hands will be reduced. Masks should be changed between procedures and sometimes during a procedure, depending on the length of the operation and the amount of talking done by the surgical team.
(b) When possible, the respiratory tract of the patient should be isolated from the incision. In some cases, isolation is achieved by using the ether screen. This serves as a barrier between the incision and the respiratory tract.
(c) Team members should not talk except when essential. Silence assists masking to reduce the number of organisms spread from nose and throat.
(d) Team members should avoid sneezing and coughing if possible.
(e) Persons who have colds or any active infection should be excluded from the OR.
(f) The scrub should cover the sterile tables with sterile drapes if an operation is delayed.
(g) Main corridors are considered contaminated areas; therefore, doors from corridors into the ORs should be kept closed. Sterile items without wrappers should not be carried through corridors. (Note the scrub room and the sterilizing area open directly into an OR in figure 1-3.) If "sterile" team members must go out into the corridor, they should change their gowns and gloves upon returning to the room.
(h) Walking through and around the OR should be kept to the necessary minimum.
(i) Visitors should sit in an observation balcony. If the entrance to this balcony is inside the surgical suite, visitors will be required to change into scrub clothes.
(j) All dusting should be damp dusting with a germicide solution. Floors should be wet-vacuumed between cases as well as at the end of the day. Dry dusting and dry mopping should be avoided in the OR, as the dust created by use of such methods would continue to settle or float in the room for hours.
(k) Powder is no longer used in the glowing process because it is likely to drift in the air, and it may cause adhesions in the surgical wound as it heals. Disposable gloves are slightly powdered, and even this is always rinsed off with sterile normal saline solution.
(l) Scrub clothes will not be worn outside the surgical suite.
(m) The bedclothes over the patient should be handled gently when he is being transferred to the operating table to avoid throwing lint off into the air. Local policy may require bedclothes to be removed in an interchange area prior to the entry in the OR; nevertheless, the patient should be covered with a cover sheet.
(n) Dressings removed from a wound should be placed at once in a bag, and the bag should be closed and discarded. Drainage that is left exposed to the air may become dried, thus enabling the infectious organisms in it to become airborne and carried to other parts of the surgical suite and the hospital to infect others.
(o) The circulator (and other team members performing nonsterile duties) should wash their hands before and after the care of each patient.