a. Preparatory Phase.
(1) Review the patient’s clinical record to verify physician’s order and to become familiar with reaso(s) for performing continuous bladder irrigation. Irrigation of the bladder is done for the following reasons:
(a) To help prevent urinary tract obstruction by flushing out small blood clots that form after prostate or bladder surgery.
(b) To create mild tamponade that may help prevent venous hemorrhaging.
(c) To treat an irritated, inflamed, or infected bladder lining.
(2) Check the patient’s medication history for hypersensitivity to antibiotics, and report significant findings to professional nurse.
(3) Wash your hands.
(4) Collect the equipment needed.
(a) Two containers of irrigating solution (usually 1,000 ml containers of normal saline or prescribed amount of antibiotic solution).
(b) Y-type IV tubing.
(c) Sterile alcohol or povidone-iodine sponge.
(d) Catheter kit with a triple lumen catheter.
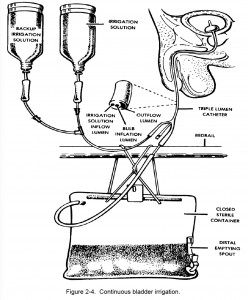
NOTE: A three-way or triple lumen catheter has three separate openings. One lumen inflates the balloon holding the catheter in place. The second lumen allows for the outflow of urine and the outflow of drainage solution. The third lumen allows for the inflow of irrigating solution (antibacterial rinse) into the bladder (figure 2-4).
(e) Closed drainage system.
(5) Approach and identify the patient and explain the procedure.
b. Performance Phase.
(1) Attach catheter to the drainage apparatus before inserting the catheter into the urethra. Catheterize the patient according to the steps previously mentioned.
(2) To prevent the introduction of organisms where the catheter enters the urethral meatus, apply an antimicrobial ointment.
(3) Begin irrigation.
(a) Provide for privacy and drape as necessary.
(b) Insert one spike of the Y-type tubing into each container of irrigating solution.
(c) Squeeze the drip chamber on each spike of the tubing.
(d) Open the flow clamps to remove air from the tubing. Close them when the fluid reaches the end of the tubing.
(e) Hang the two containers of irrigating solution on an IV pole.
(f) Clean the opening to the inflow lumen of the catheter with the sterile alcohol or povidone-iodine sponge.
(g) Insert the distal end of the I.V. tubing securely into the inflow lumen of the catheter. (The outflow lumen should already be attached to tubing leading to the drainage collection bag.)
(h) Open the flow clamp on one of the containers of irrigating solution and set the drip rate as ordered.
(4) Switch to the reserve container when the first container of irrigating solution is nearly empty.
(a) To prevent air from entering the system, do not allow the primary container to empty completely. Simultaneously close the flow clamp on the nearly empty container and open the flow clamp on the second container.
(b) Adjust the drip rate, as ordered.
(c) Disconnect the tubing from the nearly empty container with a twisting motion, being careful not to contaminate the tubing.
(d) Hang a new reserve container on the IV pole and insert the tubing, maintaining asepsis.
(e) Discard the empty container appropriately.
(f) As the irrigating solution containers become nearly empty, repeat the exchange procedure in order to maintain a constant flow of irrigation solution.
c. Follow-Up Phase. Observe special considerations while performing continuous irrigations:
(1) Always have a second container of irrigating solution available to replace the one that’s nearly empty.
(2) Check the inflow and outflow lines periodically for kinks, to make sure the solution is running freely.
(3) Measure the outflow volume correctly.
(a) Outflow volume should equal or, allowing for urine production, slightly surpass inflow volume.
(b) If inflow volume exceeds the outflow volume, suspect bladder rupture or renal damage, and notify the professional nurse immediately.
(4) Assess outflow for blood clots and/or changes in appearance.
(5) Empty drainage collection bags frequently.
(6) Document in the patient’s clinical record. Record procedure, significant nursing observations, and amount of fluid instilled and drained. Report same to professional nurse.
