a. Portal hypertension (elevated pressure in the portal vein) is a result of the increased resistance in blood flow through the portal venous circulation.
This disorder is almost always the result of cirrhosis.
b. All blood returning to the heart from the spleen, stomach, pancreas, and intestines is detoured through the liver by the portal vein. Branches of the portal vein carry the blood into the functional units (lobules) of the liver. Here, poisons are extracted by the hepatic cells to be stored or detoxified. Nutrients just absorbed from the intestines are extracted and stored or utilized in anabolism.
c. As portal pressure increases, blood backs up into the spleen and bypasses the liver, returning to the right atrium via collateral circulation. The result is splenomegaly, ascites, and varicosities of the collateral veins (esophageal and gastric varices).
d. Esophageal and gastric varices are dilated, tortuous veins in the submucosa of the esophagus and stomach. Prone to rupture, esophageal varices may require immediate emergency treatment to control hemorrhage and prevent shock and death from hypovolemia.
e. Nursing Implications. A patient with bleeding esophageal varices is to be considered in critical condition. Nursing management is aimed at assisting the physician in controlling bleeding and preventing shock and death.
(1) Monitor V.S. closely and assess level of consciousness frequently.
(2) Observe for signs of hypovolemic shock.
(3) Measure and record I&O.
(4) Administer IVF’s and blood, as ordered.
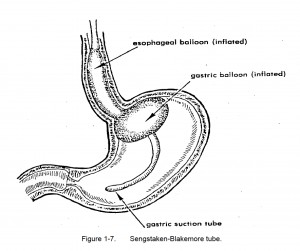
(5) Initiate balloon tamponade, as ordered. (Refer to figure 1-7 and para 1-26f, Sengstaken-Blakemore Tube.)
(6) Administer iced saline lavage, as ordered. (Refer to para 1-38, Lavage.)
(7) Offer reassurance and moral support to the patient and his family.
(a) Assess the patient’s mental status and coping mechanisms.
(b) Reinforce teaching and explanations.
(c) Report to the professional nurse any observations about the needs of the patient and his family.
