LESSON ASSIGNMENT Paragraphs 3-1 through 3-8.
TASK TAUGHT 081-833-0007, Establish and Maintain a Sterile Field.
LESSON OBJECTIVES After completing this lesson, you should be able to:
3-1. Identify the basic principles for using sterile materials.
3-2. Identify the basic steps in sterile technique.
3-3. Identify the basic procedures for setting up a sterile field.
SUGGESTION After completing the assignment, complete the exercises at the end of this lesson. These exercises will help you achieve the lesson objectives.
3-1. PRINCIPLES OF STERILE TECHNIQUE
Sterile technique refers to the way sterile materials are handled in order to keep them free of living microorganisms (germs). Sterile technique prevents contamination. Sterile technique is needed in any procedure involving contact with an open wound, breaking skin or mucous membrane, or entrance into a normally sterile body cavity. In the controlled setting of the operating room, sterile technique can be practiced exactly. The following three rules are the basis of the sterile technique.
a. An article is either sterile or contaminated.
b. A sterile article that has been touched by a contaminated article is no longer sterile.
c. Any sterile article that has become unintentionally wet or damp is no longer sterile.
3-2. BASIC STEPS IN STERILE TECHNIQUE
a. Set up for, assist with, and perform sterile procedures in a clean environment.
b. Wash hands thoroughly before beginning any sterile procedure.
c. Use only sterile supplies.
d. Keep unused sterile equipment sterile during preparation for and while performing the procedure. An object or surface is sterile when it has been made free from all living microorganisms by one of the processes of sterilization.
3-3. CREATING A STERILE FIELD
A sterile field is a work surface area prepared to hold sterile equipment during a sterile technique procedure. The sterile field provides an area in which sterility is continually maintained. The procedures for establishing a sterile field are given below.
a. Obtain the necessary equipment and supplies. All articles required for the procedure, which will be within the sterile field must be sterile.
b. Perform patient care handwash.
c. Locate a suitable surface. Set up the field on a surface that is clean, flat, dry, and free from drafts.
d. Create a sterile field using one of the two methods given below.
(1) Preferred method. The preferred method is to use a double-wrapped sterile package. Do not let your hands pass over the sterile field or the wrapped sterile object while you are establishing the field.
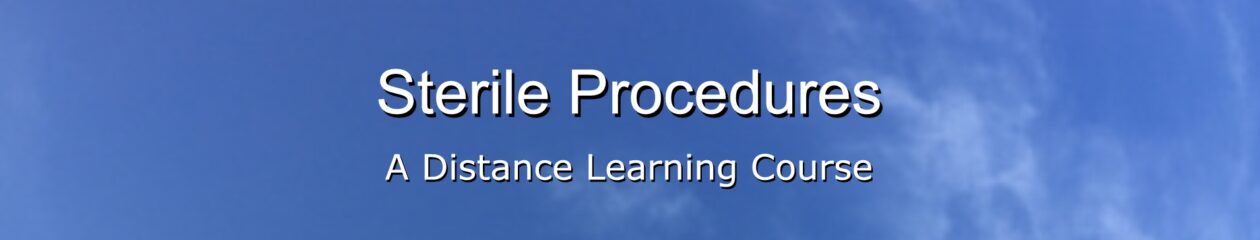
(a) Lay the package so that the flaps are on top (figure 3-1).
(b) Open the outer layer, usually a paper or plastic cover. This layer forms a barrier between the work surface and the inner wrapper.
(c) Open the inner wrapper.
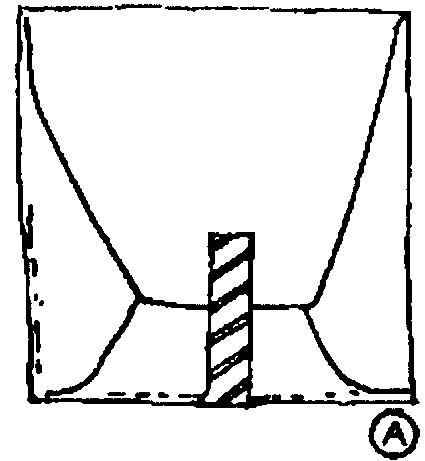
1 Using one hand lift the distal flap up and away from the package (figure 3-2). Let this flap drop gently.
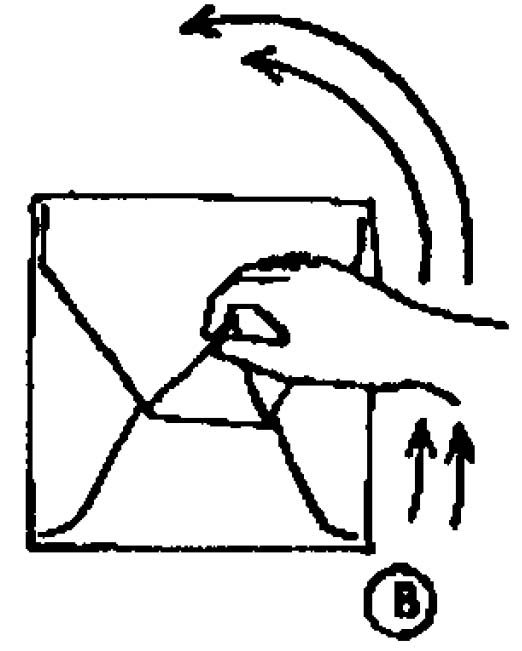
2 Open the left flap (figure 3-3).
3 Open the right flap (figure 3-4).
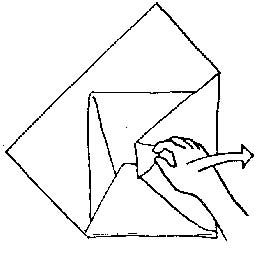
4 Then, open the near flap (figure 3-5).
5 Open the wrapper so your hand and arm do not pass over any part of the inside of the wrapper that has been exposed.
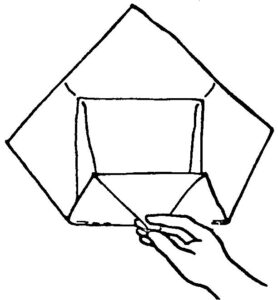
(d) Use the inside of inner wrapper as the sterile field. The object that was wrapped is now located inside a sterile field and is removed from the sterile field using sterile technique.
(2) Alternate method. Obtain package of sterile drapes or towels. Create a sterile field by opening the sterile drapes or towels in the same manner as a double-wrapped sterile package. The inside of the sterile drapes or towels form the sterile field.
CAUTION: Do not contaminate sterile field by reaching over or across it. Talk only if necessary around a sterile field to prevent the spread of bacteria. Consider an article contaminated if you have doubts about its sterility.
3-5. GIVING STERILE ITEMS TO ANOTHER WORKER
Open sterile packages without contaminating the contents. Hold the items so that a sterile worker can grasp item without contaminating himself or the item. Use the same procedures as given in paragraphs 3-4a through e.
3-6. OPENING AND POURING STERILE LIQUIDS
Sterile liquids are necessary for many procedures requiring sterile technique. Use the following procedures to open bottles containing a sterile liquid and to pour the liquids into a sterile container.
a. Lift or unscrew the cap. Do not touch bottle rim and inside cap, as these items are considered sterile. As you remove the cap, listen for a vacuum release sound. If there is no vacuum release sound, assume that the liquid is not sterile and get another bottle of the liquid to use instead.
b. Hold the cap in your hand or rest the cap upside down on table (not on sterile field since the outside of the cap is contaminated) so that the inside of the cap does not become contaminated. If the cap becomes contaminated, it cannot be used to reseal the bottle of sterile liquid and the left over portion of the sterile liquid must be discarded.
c. Glove your nondominant hand.
(1) Make sure glove package has not been contaminated (torn, and so forth) and that gloves are the proper size.
(2) Perform a patient care handwash, if you have not already done so.
(3) Place the package on a clean, dry surface.
(4) Peel back the outer wrapper.
(5) Remove the inner package and place it so that the end marked “cuff” is toward you.
(6) Grasp lower corner and open the package to a flat position.
(7) Grasp lower corners of the package and pull to the side in order to expose the cuffs.
(8) Grasp the cuff of the glove on the same side as your nondominate hand with your dominate hand. (figure 3-8).
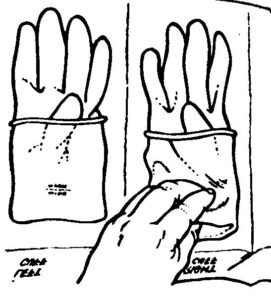
(9) Remove the glove from the wrapper, step back, and insert your nondominate hand into the glove (figure 3-9).

d. Hold bottle in your ungloved hand with label against your palm. This protects the label from dripping solution. Also a clean label can be read easily.
e. If the bottle was opened previously, pour a small amount of liquid into a waste container, usually an emesis basin. Prepouring will cleanse the lid of the bottle. The container should not be inside the sterile field.
f. Pick up the container into which the liquid is to be poured with your gloved hand and step back from the sterile field. This is done to keep any liquid from dropping onto the sterile field. If a sterile field becomes wet, consider it to be contaminated.
g. Hold the bottle about 6 inches above the container into which the liquid is being poured and pour the liquid slowly in a steady stream into the sterile container. Pouring slowly in a steady stream avoids splashing.
(1) Do not touch the bottle lip against the container. If the lip of the bottle touches the container, the container will not be sterile.
(2) Do not allow the bottle to pass over the sterile field. If the bottle passes over any part of the sterile field, then that part of the field is considered contaminated, because a microscopic organism could have fallen from the bottle or your hand onto the field.
h. Replace the container onto the sterile field.
i. Replace the cap securely on the bottle. If the cap or rim of the bottle becomes contaminated, discard the bottle.
j. Remove the sterile glove by grasping the portion of the glove over the heel of the hand and pulling the glove off. Discard the glove in an appropriate container.
k. Write the date and time and your initials on the bottle label.
l. Return the bottle to the storage area. (NOTE: Local SOP may require that you discard the bottle rather than reusing it.) Vacuum-packed sterile liquids can normally be used for 24 hours if the bottle is resealed. If your ungloved hand or other contaminated object touches the neck of the bottle, inside the bottle cap, the bottle rim, or the lip of the cap, the rim or cap is considered contaminated and you must discard the bottle.
3-7. ASSISTING WITH THE WITHDRAWAL OF STERILE SOLUTION FROM A VIAL
Some sterile liquids that are used as medications for injection come in small bottles with rubber tops. These tops can be pierced with a sterile needle in order to withdraw the sterile contents. When performing this procedure, you will be assisting a physician or other medical personnel who is wearing sterile gloves and cannot touch the outside of the vial because the vial is contaminated. You, however, will not be gloved. Follow the procedures given below.
a. Obtain a correct vial of solution. Check the bottle against the physician’s orders to verify that the solution is correct (correct name, dosage, and route).
b. Clean the vial stopper with an alcohol swab.
c. Hold the vial firmly with the label up so that the person with the sterile gloved hands can verify that the solution is the proper one. The gloved person then:
(1) Pulls the plunger of the syringe to the amount of solution required.
(2) Inserts the needle through center of rubber stopper.
(3) Pushes the plunger into the syringe to increase air pressure inside vial (figure 3-10).

(4) Pulls plunger out to somewhat more than the prescribed level.
(5) Withdraws the needle with a quick straight pull. (If the needle touches the outside of the vial, then the needle is contaminated and the entire procedure must be done again.)
d. Discard or store vial in accordance with local SOP.
NOTE: Withdrawing fluid from an ampule is accomplished in basically the same manner.
3-8. NOTIFYING PERSONNEL THAT STERILE FIELD IS CONTAMINATED
Any individual who observes the contamination of the sterile field, regardless of rank or position, must immediately notify all individuals performing the procedure that the sterile field is contaminated and how the contamination occurred.