1-5. PREVENTION OF WOUND INFECTION
Steps to prevent wound infection must be taken by each person who renders aid, care, or treatment to the casualty. Although all combat wounds are contaminated by their nature, the following precautions can be taken to avoid converting contaminated wounds to infected wounds and to minimize the occurrence of wound infections.
a. Sterile Dressing. The application of a sterile dressing over the wound will lessen the chance of contamination becoming infection.
b. Clean Hands. Persons giving direct care and treatment to patients should wash their hands in soap and water or rinse hands in antiseptic. Hands contaminated with blood, vomitus, mucus, urine, or feces should be thoroughly scrubbed before providing care and treatment.
c. Clean Wound.
(1) Minor cuts and bruises may be scrubbed vigorously with soap and water and dried with sterile cotton before dressings are applied.
(2) If an antiseptic is immediately available, it may be applied around a superficial wound when hemorrhage is not severe and when surgery is expected to be delayed for more than six hours after the injury occurred.
(a) When applying antiseptic around a wound, use a sterile cotton swab. Start at the wound edge and apply the antiseptic away from the wound. Do not retrace.
(b) Do not put antiseptic into the wound nor permit it to drain into the wound.
(c) Do not remove or loosen a dressing to apply antiseptic around the area of the wound.
(d) Do not touch the antiseptic supply with a used swab or anything else not sterile.
(e) Do not breathe, cough, or sneeze on wounds or sterile items.
d. Precautions. Avoid causing further injury and prevent chilling, exposure, fatigue, and other factors which lessen the body’s resistance.
e. Medication. Antibiotics and tetanus toxoid, if needed, are usually administered at the aid station.
1-6. BODY DEFENSES
The body incorporates certain defenses against the invasion of pathogens causing infection.
a. Skin. The skin is the first line of defense since most pathogens cannot enter unbroken skin.
b. Phagocyte. Another line of defense is phagocyte cells such as white blood cells. These cells engulf pathogens and absorb them. Phagocytes increase in numbers at the site of infection.
c. Immune Substances. Still another line of defense is the development by the body of antibodies and antitoxins. Because pathogens are foreign substances, the body reacts and destroys them by producing immune bodies. All patients vulnerable to gross infection or infectious diseases, particularly tetanus, should receive indicated prophylactic doses of antibiotics and immunizing agents.
d. Lymphatic System. The lymphatic system also defends the body against invading pathogens. The lymph acts like a washing machine for the body. It cleanses the body tissues. Lymph flows into the tubules and glands that act as filters and strains the invaders.
e. Factors Which Lesson Body Defenses. Several factors that may be present in combat casualties tend to lessen body defenses. They include wound injuries, chilling, exposure, fatigue, and malnutrition.
1-7. SIGNS AND SYMPTOMS OF INFECTION
Inflammation is a purposeful reaction of tissue to injury. If it develops in the absence of pathogens, it is called a sterile inflammation. When produced by pathogens, it is called septic.
a. Changes in Tissue Caused by Inflammation. The changes induced in infected tissues by inflammation consist of heat, redness, swelling, sensitivity, tenderness, and pain. In addition, red streaks radiating from the affected area may be present as well as pus formation, usually in the center of the infection. Malaise, headache, and fever may also be present.
b. Sepsis. If the infectious process cannot be localized in the wound area by the body’s defenses, it eventually spreads so that a generalized septic condition or septicemia develops. This may result in shock that can lead to death.
1-8. CYCLE OF INFECTION
Prevention and control of infection is of vital importance to the patient as well as to health care personnel. In order to provide proper care for patients with communicable diseases or infectious organisms, you should understand the components of infection and the methods to control the cycle of infection. The cycle of infection (see figure 1-1) is like a chain consisting of six links. To produce disease, each link of the infectious process must be present in a logical sequence. Removing one link in the chain will control the cycle of infection. The six links are discussed in the following paragraphs.
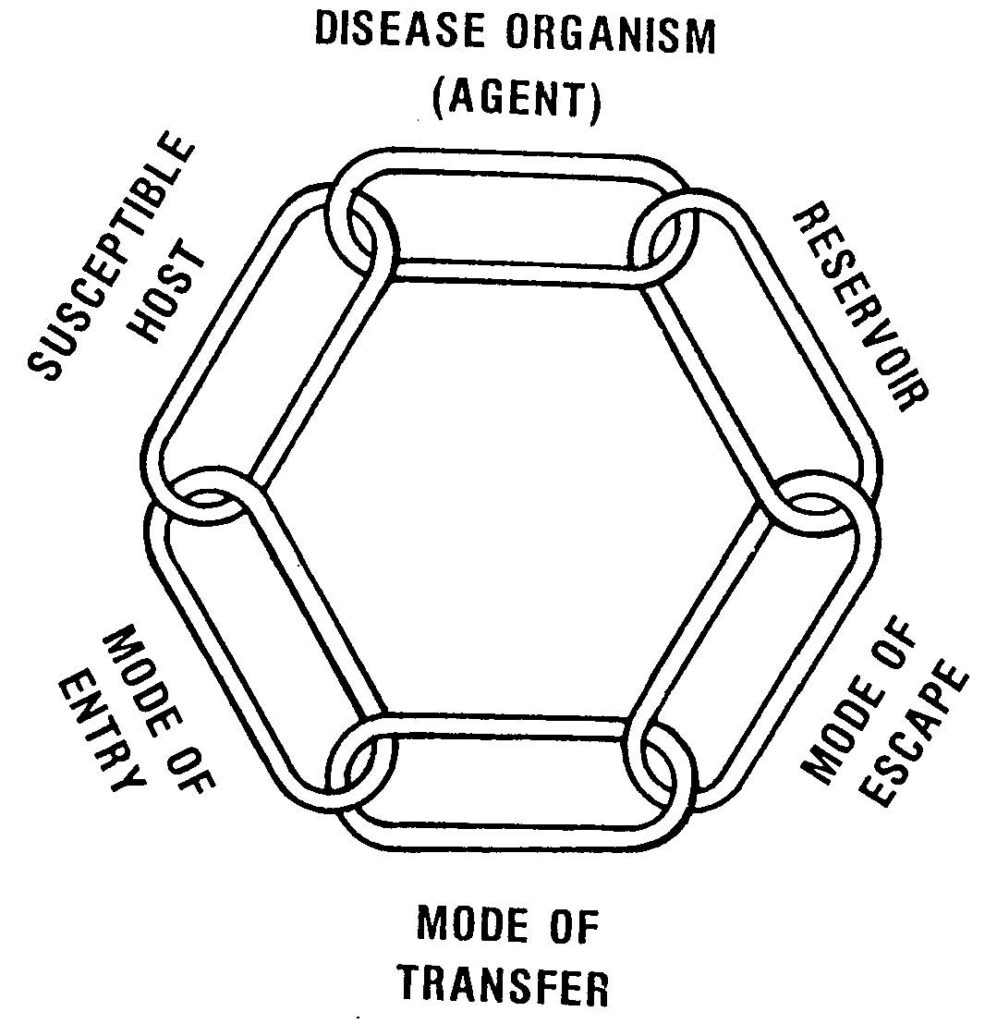
a. Infectious Microorganisms (Agent). These are the pathogens that cause communicable diseases.
b. Reservoir. The reservoir (source) is the person or animal that has the disease. Sometimes a person may have a disease but is not ill. This type of person is called a carrier. The carrier known as Typhoid Mary is a classic example. She was a food worker in a restaurant who spread the disease typhoid by contaminating the foods she handled. Other examples of reservoirs are a person with a common cold, a person with malaria, a person with syphilis, a rat with plague, and a bat with rabies.
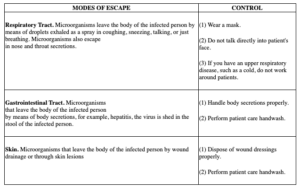
c. Mode of Escape. This refers to the route by which the infectious microorganisms escape the reservoir. For example, pathogens that cause respiratory diseases usually escape through the respiratory tract (coughing, sneezing, and so forth) Modes of escape and methods of controlling the mode (preventing the escape) are shown in figure 1-2.
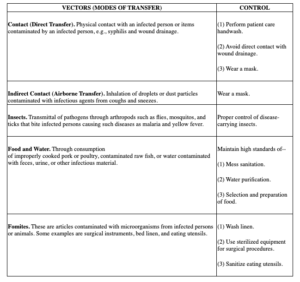
d. Vector. The vector is the connection between the source of the disease (reservoir) and the person who is going to catch the disease (host). The vector is sometimes referred to as the “vehicle of disease transmission.” Vectors and their control are discussed in figure 1-3.
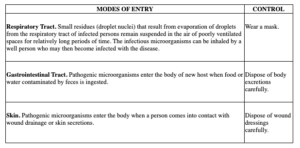
e. Mode of Entry. The mode of entry refers to the method by which the pathogens enter the person (host). For example, some pathogens are inhaled (respiratory tract). Ways of controlling modes of entry are shown in figure 1-4.
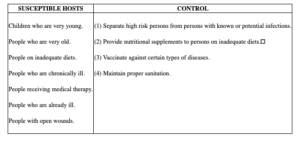
f. Susceptible Host. The host is the person who gets the disease. Once the host has the disease, he becomes a reservoir for future transmission of the disease. A listing of the most susceptible persons to disease and some control measures are shown in figure 1-5.