1-3. INTRODUCTION
a. Personal cleanliness is of extreme importance for operating room personnel. A daily shower, frequent shampoos, and attention to hands and fingernails are most important. Because of the close contact with other members of the “sterile” team, personnel should also use a body deodorant. They should note and report to the operating room supervisor any infection, rash, or open lesion about the hands, nails, and arms. They should also report any signs of a cold or other systemic infection.
b. The specialist must make specific preparation before he begins to scrub. Such preparation, which is necessary to further eliminate factors of contamination, is discussed in paragraphs 1-4 through 1-9.
c. For the specialist to perform the scrub most effectively, certain features and equipment should be available in the scrub rooms within the surgical suite (see paragraph 1-10).
1-4. FINGERNAILS
The specialist should keep his fingernails short enough so that they are not visible over the tips of the fingers. Short nails are easy to clean and, if kept smooth, will not puncture gloves. Nails should be free of polish.
1-5. JEWELRY
The specialist is to remove all jewelry from his hands and arms. He may pin these items in a pocket of his scrub suit. Bacteria and dead skin cells accumulate beneath watches, bracelets, and rings.
1-6. SCRUB SUIT
a. The specialist is to don a clean, short-sleeved cotton scrub suit each day before entering the semi-restricted/restricted areas of the surgical suite. Street clothes or hospital uniforms are never worn in these areas. The scrub suit should cover all other clothing such as undergarments. The scrub shirt must be tucked into the trousers to avoid contamination by the shirt tail flapping on a sterile field. The trouser legs should not touch the floor as this may transport bacteria from one place to another.
b. The specialist assigned to scrub should adjust the sleeves of his scrub suit to at least four inches above his elbows.
Editor’s Note
According to this AMEDD text, the scrub shirt should always be tucked into the trousers to prevent “flapping” and accidental contamination of a sterile field. However, in most surgical suites in and out of the military, it is an individual choice whether to tuck the shirt in or leave it out. As an untucked shirt improves air circulation and body cooling, many people prefer that it remain untucked. Sometimes, for specific types of surgical cases, it is necessary to either leave the tail out or in, but that would be specified by local surgical policy.
1-7. SHOES
a. Ideally, the specialist should keep a pair of shoes for wear in the surgical suite only and he should keep these shoes clean. Shoe soles are a source of gross contamination and of cross infection from one area of the hospital to another.
b. Street shoes (military low-quarters and/or nursing white shoes) are never worn in the restricted areas of the surgical suite unless shoe covers are placed over them. Shoe covers should be worn on a single-use basis. They must be removed on leaving the restricted area and a fresh pair put on before reentrance to that area.
c. Local policy governs the wearing of the scrub suit shoes and shoe covers.
1-8. SURGICAL CAP
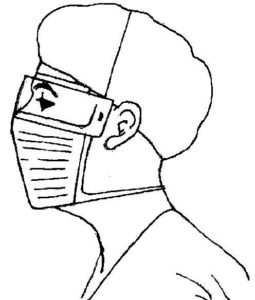
The specialist is to wear a clean head cover each day; most hospitals use disposable hoods and caps. He should wear it in a manner to cover the hair completely (see Figure 1-1). The wearing of the cap prevents the possible contamination of the sterile field by falling hair or dandruff.
1-9. SURGICAL MASK
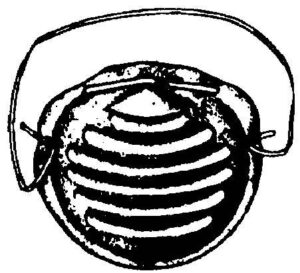
a. The surgical mask is worn primarily to protect the patient from bacteria exhaled from the oro- and nasopharynx of operating room personnel. Two types of disposable masks that are standard items are, one with paired head and neck ties (see Figure 1-1) and a cup type with an elastic headband (see Figure 1-2). Both are made of a nonwoven fabric with adjustable metal nosepieces along the top of the mask. The metal stay is used to hold the mask snugly to the face, thus preventing fogging of the specialist’s glasses if worn. The mask must fit snugly around the nose and mouth to filter air through it rather than permit the passage of air around the sides. The specialist is to don a fresh mask immediately before beginning the scrub procedure. The mask is not considered sterile.
b. After the mask has become damp, droplets from the nose and mouth can easily pass through it–the mask no longer serves as a barrier to germs. Therefore, the mask should be changed after each procedure and more often if it has become damp.
c. The specialist should never allow the mask to dangle around his neck. He should never place the mask in his pocket or on a clean surface and he should not handle it except by the ties and/or elastic headband after it is removed. Careful handling of a soiled mask prevents the spread of microorganisms throughout the surgical suite.
d. When removing the mask, the specialist should handle it by the ties and/or elastic headband and should immediately place it in the designated receptacle. As soon as he removes a soiled mask, the specialist should wash his hands.
1-10. SCRUB ROOMS
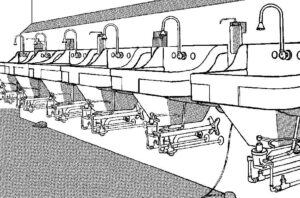
a. A scrub area should be situated between each two operating rooms and should open directly into an operating room. The sinks should be deep enough, at least one foot, so that water will not be splashed onto the scrub clothes, the floor, or the hands and arms during the procedure (see Figure 1-3). The sinks should be provided with hot and cold water faucets which should be controlled by knee levers or by foot levers. If arm or hand levers must be used, these controls must be adjusted for water temperature flow before starting to scrub. If the specialist’s hands or arms accidentally touch the faucets or the sink during any phase after the scrub has begun, he has become contaminated and must begin the scrubbing cycle again. Running water is preferred because it completely and easily rinses away suds containing bacteria.
b. Containers for surgical detergents are placed between each two sinks. Foot-operated pedals attached to the containers provide a convenient method of dispensing detergents without contaminating the hands. Scrub brushes (depending on the type used) may be placed in dispensers, one between each two sinks. A clock should be provided for timing the scrub procedure when required.
