Abdominal and Pelvic Pain
Any patient complaining of pelvic pain should have a pregnancy test. I am surprised at how often it is positive despite the patient saying "that's impossible."
Most patients complaining of intermittent, chronic pelvic pain will benefit from oral contraceptive pills. BCPs reduce or eliminate most dysmenorrhea and have a favorable influence on other gynecologic problems such as endometriosis, ovarian cysts, and adenomyosis, a benign condition in which the uterine lining grows into the underlying muscle wall, causing pain and heavy periods.

When using BCPs to treat chronic pelvic pain, multiphasic BCPs such as Ortho Novum 7/7/7, Triphasil or Tri-Norinyl have not been as effective as the stronger, monophasic BCPs such as LoOvral, Ortho Novum 1+35 or Demulen 1/35 (in my experience). I believe the reason is that the multiphasic pills, by virtue of their lower dose and changing dosage, do not suppress ovulation as consistently as the higher-dose pills.
If the BCPs do not help or if the patient continues to have pain during her menstrual flow, change the BCP schedule so the patient takes a monophasic (LoOvral, 1+35, etc.) BCP every day. She will:
- not stop at the end of a pack.
- not wait one week before restarting.
- not have a menstrual flow.
If she doesn't have a menstrual flow, she can't get dysmenorrhea. Taken continuously, BCPs are effective and safe. The only important drawback is that she will not have a monthly menstrual flow to reassure her that she is not pregnant.
Because the birth control pills are so very effective in treating dysmenorrhea, the emergence of cyclic pelvic pain while taking BCPs is a worrisome symptom. Endometriosis can cause these symptoms. Happily, birth control pills, particularly if taken continuously, are a very effective treatment for endometriosis. Upon return to a garrison setting, women with pain while taking should be evaluated by an experienced gynecologic clinician.
After a number of months, women on continuous BCPs will usually experience spotting or breakthrough bleeding. It is not dangerous. If this becomes a nuisance, stop the BCPs for one week (she'll have a withdrawal bleed), and then restart the BCPs continuously.
Read more about Birth Control Pills
Any pregnant patient who experiences bleeding should lie still (bedrest) until the bleeding stops for a few days. Then she may be moved to a definitive care setting (hospital). If she is destined to miscarry, having her lie still will not prevent the miscarriage, but it will probably postpone the miscarriage until she can be moved to a safe place where D&C capability is present.
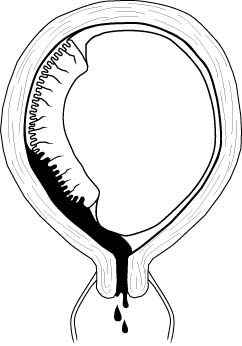
Patients who are more than 20 weeks pregnant who have constant pain in the uterus are probably experiencing a placental abruption (premature separation of the placenta), particularly if the uterus is tender. They may or may not have vaginal bleeding.
When hospital care is available, these women are best evaluated by an obstetrician with the technologic resources of electronic fetal monitoring, ultrasound and a sophisticated laboratory testing. In isolated settings, bedrest with the patient lying on her left side and IV hydration are really the only options you have. If the pain improves with bedrest, keep the patient at rest. Consider transport later, after the pain resolves. If the pain shows no evidence of improving with rest, then you will need to transport her sooner since severe placental abruption may be fatal to the patient and/or her baby. Definitive treatment consists of cesarean section and treatment of the coagulopathy (bleeding disorder) that usually accompanies this problem.
If neither definitive therapy (cesarean section) nor medical evacuation are available, the following generalizations can be made:
- With very mild cases, the contractions will usually go away with bedrest and the pregnancy will continue for a while (days to weeks) although early delivery is usually the rule. The ultimate outcome for mother and baby is generally good if the mild abruption is the only significant problem.
- For moderate degrees of placental abruption, the woman usually goes into premature labor and delivers. She generally does well, but the baby may be stillborn or severely incapacitated.
- For severe degrees of placental abruption, if the woman does not deliver very promptly, the abruption will likely prove fatal to her because of the marked coagulopathy that develops. If the baby is not delivered within 10 to 20 or 30 minutes of the severe abruption, it will likely be stillborn.
Under these circumstances, supportive treatment (bedrest, IV fluids, blood transfusions) may be lifesaving.
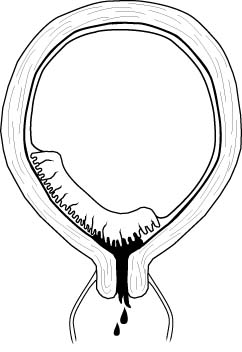
Any pregnant patient beyond the 20th week of pregnancy who is bleeding should lie still and YOU SHOULD NOT DO A PELVIC EXAMINATION UNLESS INSTRUCTED TO DO SO BY A CONSULTING OBSTETRICIAN. In most cases, the bleeding comes from a small placental abruption and will temporarily resolve with bedrest. Occasionally, the bleeding will be from a "placenta previa," a condition in which the placenta is located immediately behind the cervix. If you perform a pelvic exam on a patient with placenta previa, you may cause massive bleeding which you won't be able to stop without a cesarean section.
Most bleeding in pregnant patients will stop temporarily with bedrest. If a definitive treatment center is close (a brief, smooth ambulance ride), then immediate transport of the patient is best. If a definitive treatment center is distant, it is probably better to stop the bleeding first with bedrest. Move her after a few days when the long and perhaps bumpy transport is less likely to re-start the bleeding. If the bleeding shows no sign of slowing despite bedrest, you may need to begin transport anyway.
Should transport not be an available option:
- Continue the bedrest as long as there is any bleeding. Marginal placenta previas may resolve with time and successful vaginal delivery, while dangerous, can be successful. In this case, pressure from the fetal head on the placenta tends to compress or tamponade the loss of blood from the placenta long enough to achieve a successful delivery.
- In cases of a complete placenta previa, where the placenta totally covers the internal cervical os, maternal death during labor, due to intractable hemorrhage is the rule.
Gradual onset of mild bilateral pelvic pain with purulent vaginal discharge is the typical complaint. Fever <100.4 and deep dyspareunia are common.
Moderate pain on motion of the cervix and uterus with purulent or mucopurulent cervical discharge is found on examination. Gram-negative diplococci or positive chlamydia culture may or may not be present. WBC may be minimally elevated or normal.
Treatment consists of Doxycycline 100 mg PO BID x 10-14 days, plus one of these:
- Cefoxitin 2.0 gm IM with probenecid 1.0 gm PO, OR
- Ceftriaxone 250 mg IM, OR
- Ceftizoxime 1 gm IM, OR
- Cefotaxime 0.5 gm IM
Alternative treatment includes:
- Ofloxacin 400 mg orally twice a day for 14 days, PLUS
- Metronidazole 500 mg orally twice a day for 14 days
For further information, read the CDC Treatment Guidelines for PID
With moderate to severe PID, there is a gradual onset of moderate to severe bilateral pelvic pain with purulent vaginal discharge, fever >100.4 (38.0), lassitude, and headache. Symptoms more often occur shortly after the onset or completion of menses.
Excruciating pain on movement of the cervix and uterus is characteristic of this condition. Hypoactive bowel sounds, purulent cervical discharge, and abdominal dissension are often present. Pelvic and abdominal tenderness is always bilateral except in the presence of an IUD.
Gram-negative diplococci in cervical discharge or positive chlamydia culture may or may not be present. WBC and ESR are elevated.
Treatment consists of bedrest, IV fluids, IV antibiotics, and NG suction if ileus is present. Since surgery may be required, transfer to a definitive surgical facility should be considered.
ANTIBIOTIC REGIMEN: (Center for Disease Control, 1998)
Doxycycline 100 mg PO or IV every 12 hours, PLUS either:
- Cefoxitin, 2.0 gm IV every 6 hours, OR
- Cefotetan, 2.0 gm IV every 12 hours
This is continued for at least 48 hours after clinical improvement. The Doxycycline is continued orally for 10-14 days.
ALTERNATIVE ANTIBIOTIC REGIMEN: (Center for Disease Control, 1998)
- Clindamycin 900 mg IV every 8 hours, PLUS
- Gentamicin, 2.0 mg/kg IV or IM, followed by 1.5 mg/kg IV or IM, every 8 hours
This is continued for at least 48 hours after clinical improvement. After IV therapy is completed, Doxycycline 100 mg PO BID is given orally for 10-14 days.Clindamycin 450 mg PO daily may also be used for this purpose.
ANOTHER ALTERNATIVE ANTIBIOTIC REGIMEN: (Center for Disease Control, 1998)
- Ofloxacin 400 mg IV every 12 hours, PLUS
- Metronidazole 500 mg IV every 8 hours,
ANOTHER ALTERNATIVE ANTIBIOTIC REGIMEN: (Center for Disease Control, 1998)
- Ampicillin/Sulbactam 3 g IV every 6 hours, PLUS
- Doxycycline 100 mg IV or orally every 12 hours.
ANOTHER ALTERNATIVE ANTIBIOTIC REGIMEN: (Center for Disease Control, 1998)
- Ciprofloxacin 200 mg IV every 12 hours, PLUS
- Doxycycline 100 mg IV or orally every 12 hours, PLUS
- Metronidazole 500 mg IV every 8 hours.
For further information, read the CDC Treatment Guidelines for PID
Bureau of Medicine and
Surgery |
Operational Obstetrics
& Gynecology - 2nd Edition |