|
|
||||
Shoulder PainThe shoulder is a complex, unstable, and intricate joint that can be injured both through trauma and overuse. Shoulder pain is usually due to injury to one of three main groups of shoulder structures:
Determine the mechanism of injury and the extent of disability. A good history and physical will usually determine the cause of the pain and direct the care. Differential diagnosis of shoulder pain: Acute injuries
Chronic injuries
Referred pain
History and physical Always verify the distal pulses, capillary refill, and sensation. The key to understanding shoulder pain is understanding the anatomy:
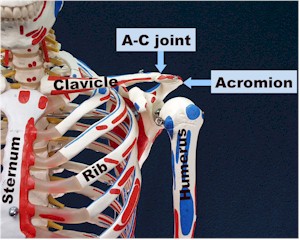
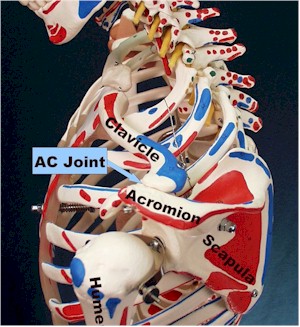
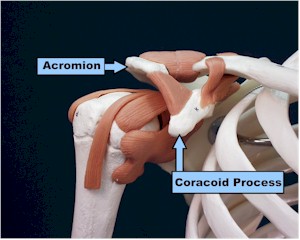
The bony structures and AC joint are usually injured through trauma:
The glenohumeral joint is made of the glenoid fossa of the scapula, the humeral head, the joint capsule, and the labral cartilage, essentially the meniscus of the shoulder which helps hold the humeral head in place. These structures are usually injured through trauma, especially with an anterior dislocation or subluxation.
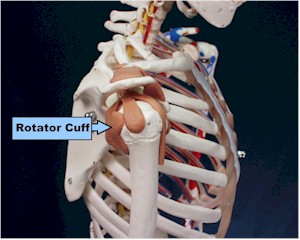
The rotator cuff muscles all originate off the scapula and wrap around the humerus, helping to hold the humerus in the glenoid fossa. The subscapularis comes from the underside of the scapula and wraps around to attach anteriorly on the humerus; it internally rotates the arm. The supraspinatous originates above the spine of the scapula, runs under the acromium and over the humerus to attach on the lateral humerus, abducting the arm. It is the muscle that commonly gets impinged between the acromium and humerus and is usually the one torn in rotator cuff tears. The infraspinatous and teres minor come from the lower scapula attaching to the posterior humerus. Therefore, when they contract they externally rotate the humerus. The rotator cuff is rarely torn in young people without a dramatic injury such as when a baseball pitcher blows out his arm. Older folks get degenerative tears. Testing of the rotator cuff
muscles is done by testing internal rotation (subscap.), external rotation (teres minor and infrasp.) and abduction with
the thumbs down and arms parallel to the ground (supraspin.). The impingement test is done by having the arm 90 degrees forward
flexed parallel to the ground and then gently internally rotating. Pain indicates a positive test.
When should x-rays be obtained?
What other studies should be considered?
Treatment plan. Treatment depends on the severity of the injury.
In general , follow the guidelines for treatment of acute injuries: PRICEMM
Rehabilitation begins with ranges of motion
exercises. Pendulum
exercises where the patient leans over and gentle rotates the arm in a
circular motion are usually the first activities started. Gradually increase motion, then work on strength. Rotator cuff strengthening exercises are useful in many
conditions and are essential for treatment of impingement syndrome. Endurance is worked on next, followed by specific activity
training.
Treatment of specific conditions:
Anterior shoulder dislocations can be reduced easier if reduction is performed soon after the injury. Although controversial, x-rays probably do not need to be performed prior to relocation unless there is an obvious fracture. Delaying reduction allows the shoulder muscles to spasm and makes reduction much more difficult, especially if pain medicine and x-ray are not readily available. There are many techniques to reduce dislocations. One way that does not require any assistance or special equipment involves having the patient lay supine.
Rotator cuff tendonitis and tears. If a large tear is suspected in a young person, consider obtaining an MRI, arthrogram, and urgent referral. Smaller tears and tendonitis are usually treated by rehabilitation using the standard protocol of improving range of motion, then strengthening the rotator cuff muscles. Consider MRI and/or referral if symptoms don’t improve. Scott D. Flinn, MD
Home · Military Medicine · Sick Call · Basic Exams · Medical Procedures · Lab and X-ray · The Pharmacy · The Library · Equipment · Patient Transport · Medical Force Protection · Operational Safety · Operational Settings · Special Operations · Humanitarian Missions · Instructions/Orders · Other Agencies · Video Gallery · Forms · Web Links · Acknowledgements · Help · Feedback Approved for public release; Distribution is unlimited.
*This web version is provided by The Brookside Associates, LLC. It contains original contents from the official US Navy NAVMED P-5139, but has been reformatted for web access and includes advertising and links that were not present in the original version. The medical information presented was reviewed and felt to be accurate in 2001. Medical knowledge and practice methods may have changed since that time. Some links may no longer be active. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the US Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense.
© 2015, Brookside Associates, LLC. All rights reserved |
|
|||