Low Back Pain
Initial evaluation requires:
Chronic pain or pain that is refractory to
conservative treatment requires a more thorough evaluation noting any
changes in the history as to character, pattern and associated symptoms.
Differential Diagnosis of low back pain
-
“Mechanical” low back pain
-
Sciatica
-
Herniated nucleus pulposus with/without nerve
impingement
-
Spondylolysis with or without Spondylolysthesis
-
Scoliosis
-
Sacroiliac joint (SI joint) dysfunction
-
Rare causes:
-
Infection
-
Connective tissue disease (e.g. Ankylosing spondylitis)
-
Tumor
-
Referred pain – e.g. kidney stone,
abdominal aortic aneurysm (AAA)
-
Spinal stenosis
History
Ask usual questions about the pain such as:
-
Duration
-
Character
-
Radiation
-
What makes it worse and better
-
Associated symptoms
-
Neurologic symptoms of numbness, tingling or
weakness
-
Any loss of bowel or bladder control
-
Trauma
-
Previous treatment
Physical Exam
-
Check for range of motion of the back in
-
Inspect the back for obvious signs of
deformity.
-
While forward flexing, look for one shoulder
higher than the other- this would suggest scoliosis.
-
Palpate the spinous processes and surrounding
tissues for tenderness.
-
Note any paraspinal muscle spasm.
-
Perform a neurological exam as detailed below
for a suspected herniated disk:
|
MMT
(0 to 5) |
Sensory |
Deep Tendon Reflexes |
L4 |
Anterior Tibialis (Dorsiflexors) |
Medial Malleolus |
Patella |
L5 |
Ext. Hallicus (Great Toe Extension) |
1st Web Space |
N/A |
S1 |
Peroneal (evertors) |
Lateral Malleolus |
Schilles |
-
Rectal tone if loss of bowel or bladder control
(S2, 3,4)
-
Straight leg raise – note the degree of
flexion that reproduces the radiating symptoms
-
Biomechanics should
be evaluated as they may contribute to low back pain and may be
corrected.
Additional tests:
-
Stork – back extended while lifting one leg
(pain in spine => R/O pars interarticularis defect; seen on
oblique X-rays)
-
Fabere– for hip and SI joint involvement. Pt supine with involved side foot on opposite knee (flexed
abducted, externally rotated hip) causes pain in hip; then to stress
the SI joint, press down on flexed knee and the opposite anterior
superior iliac spine
-
Gaenslen’s sign (SI joint pain) – with both
legs drawn onto chest, shift pt to side of table (one buttock over
edge); the unsupported leg drops over the edge while the opposite
leg remains flexed
-
SI compression/distraction – compress or
distract pelvis
Radiologic tests
-
Plain radiographs are not recommended for
routine evaluation of acute LBP within the first month unless a
finding from the history and physical exam raises concern such as
signs and symptoms of spondylolysis, scoliosis, cauda equina
syndrome, tumor or infection. Indications for further studies are reserved for patients
whose symptoms continue despite conservative treatment.
-
X-rays (deformity of spine). Check obliques if suspect spondylolysis
-
MRI (tumors, infection, HNP, spinal stenosis)
-
Bone scan if spondylolysis and can’t tell if
new or old
Lab Tests
Waddell’s test is used to
look for nonorganic back pain. 3 or more positive responses suggest psychosocial issues
as cause of pain:
-
Tenderness (superficial nonanatomic, tenderness
to light touch)
-
Simulation tests (axial loading – vertical
loading on the skull; rotation – passive rotation of shoulders and
pelvis in same plane causes pain)
-
Distraction (discrepancy between sitting and
supine straight leg raising tests)
-
Regional disturbances (nonanatomic weakness or
paresthesia)
-
Overreaction (disproportionate facial
expression, verbalization or tremor)
What should one look for to determine if there
is a need for emergent referral/ Medevac:
-
Cauda equina syndrome – pressure on the cauda equina/nerves in
the spine from a herniated disk or other tissue that causes
bladder/bowel incontinence, urinary retention, saddle anesthesia, loss
of anal sphincter tone, neurological compromise or progressive major
motor weakness of lower extremity. If the pressure is not relieved in a timely fashion there may be
permanent neurologic damage.
-
Fracture – history of
trauma, step off on exam, neurologic signs/symptoms
-
Infection – fever, toxic appearing patient
-
Tumor/malignancy -
unexplained weight loss, night sweats, night pain, x-ray lesions
-
AAA - Inability to find
position of comfort, referred pain, pulsatile mass in belly – usually
in elderly
Management of low back pain
-
If there are no worrisome signs or symptoms, low
back pain is usually managed conservatively very successfully – 80-90
percent will be recovered in 4-6 weeks.
-
Radicular symptoms that are not progressing can be
managed conservatively.
-
Reduce activity – relative rest. Not bed rest – bed rest for longer than a day actually
deconditions the body and may produce a prolonged time to recovery
-
Pain management -NSAIDs, tylenol
-
Modalities such as ice,
heat, ultrasound may help
-
Gentle flexibility
exercises for back, hamstrings
-
Strengthening of abdominal
muscles/trunk support
-
If signs and symptoms worsen or do not improve over
4 weeks, consider radiographic studies.
Sciatica
Sciatica refers to a form of low back pain where the sciatic nerve is
irritated. The sciatic
nerve is the coalition of S2, 3, and 4. There is often pain in the area of the sciatic notch and this may
be where the nerve is irritated. Treatment
is the same as mechanical low back pain.

Vertebral Anatomy

Scoliosis with S-curve of the spine

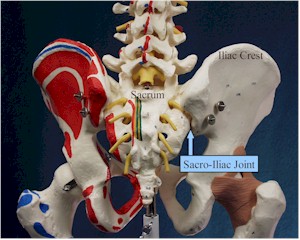
Sacro-Iliac Joint from the Front
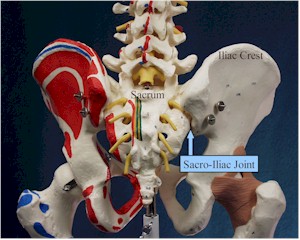
SI Joint from the Rear
Chris
Polkoski, MS, PA-C and CDR Scott D. Flinn, MC, USN
Home
· Military Medicine
· Sick Call · Basic Exams
· Medical Procedures
· Lab and X-ray · The Pharmacy
· The Library · Equipment
· Patient Transport
· Medical Force
Protection · Operational Safety · Operational
Settings · Special
Operations · Humanitarian
Missions · Instructions/Orders · Other Agencies · Video Gallery
· Forms · Web Links · Acknowledgements
· Help · Feedback
Approved for public release;
Distribution is unlimited.
Bureau of Medicine and Surgery
Department of the Navy
2300 E Street NW
Washington, D.C
20372-5300 |
Operational Medicine
Health Care in Military Settings
CAPT Michael John Hughey, MC, USNR
NAVMED P-5139
January 1, 2001 |
United States Special Operations
Command
7701 Tampa Point Blvd.
MacDill AFB, Florida
33621-5323 |
*This web version is provided by The Brookside Associates, LLC. It contains
original contents from the official US Navy NAVMED P-5139, but has been
reformatted for web access and includes advertising and links that were not
present in the original version. The medical information presented was reviewed and felt to be accurate in 2001. Medical knowledge and practice methods may have changed since that time. Some links may no longer be active. This web version has not been approved by the
Department of the Navy or the Department of Defense. The presence of any
advertising on these pages does not constitute an endorsement of that product or
service by either the US Department of Defense or the Brookside Associates. The
Brookside Associates is a private organization, not affiliated with the United
States Department of Defense.
© 2015, Brookside Associates, LLC. All rights reserved
Other Brookside Products
|
|