Knee Pain
Knee Pain
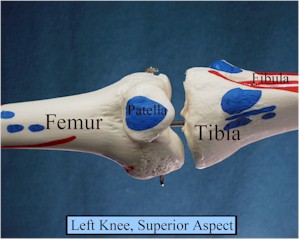
Knee
pain is a common sick call complaint with a broad differential
diagnosis. It is important
to differentiate in the history how the knee became painful. Based on the mechanism of injury, one can narrow the possible
diagnoses into a working differential diagnosis, further refined using
the history and physical.
Differential
diagnosis of knee pain
Trauma
/acute
-
Fracture
-
Internal Derangement
-
Meniscal
injury (most common)
-
Ligamentous
injury – Anterior Cruciate (ACL), Posterior Cruciate (PCL),
-
Medial
Collateral (MCL), and Lateral Collateral (LCL)
-
Knee
dislocation (multiple ligamentous tears and unstable knee)
-
Pre patellar Bursitis
-
Patellar Dislocation (not to be confused with knee
dislocation)
Overuse/chronic
-
Patellofemoral
Syndrome (PFS)
-
Iliotibial
Band Syndrome (ITBS)
-
Degenerative
joint disease (DJD) (Osteoarthritis)
-
Stress
fractures
-
Meniscal
tears (if missed acutely)
-
Patellar
tendonitis
-
Osteochondritis Dessicans (OCD) and loose bodies
Infection/
acute arthritis
History
This will
narrow the focus. Key
historical points include:
-
Mechanism
of injury
-
Location
of pain, noise or other sensations
-
Ability
to bear weight
-
Location
and rapidity of swelling
-
Giving
way – mechanical instability vs. guarding from pain
-
Locking-
unable to move leg unless physically manipulate it to unlock it.
Trauma
Overuse
Injuries can often be distinguished by their location and
character of pain
Septic
Joint
-
A
surgical emergency and should be treated as such.
-
The
patient will have a very painful active and passive Range of Motion
(ROM).
-
They
may also have erythema and a fever.
Physical
exam:
-
Observe
for edema (swelling outside/around the joint), erythema
-
Palpate
the knee.
-
Feel
for an effusion. An
effusion will be due to one of three things and represents
intraarticular pathology. Tapping the knee is indicated for ruling out infection and to
relieve pain. If you do
not suspect infection and the patient’s knee is not painful due to
a tense effusion, you do not need to tap.
-
Reactive
– clear fluid due to DJD, etc
-
Inflammatory
– infection, crystal disease – has WBCs
-
Bloody
– tear in structures such as ligaments, meniscus, bone (look
for fat)
-
Perform
specific maneuvers
-
Lachman
– for ACL tear
-
McMurray’s,
joint line tenderness, flick and duck walk – meniscus
-
Diffuse
medial or lateral tenderness, check for stability at 0 and 30
degrees
-
Check
for patellar signs: Quad inhibition and patellar compression for
PFS, Patellar apprehension for dislocation/subluxation
-
Palpate
patellar tendon for signs of tendonitis
-
Check
distal pulses and sensation – may have vascular injury e.g.
with dislocated knee
When
are x-rays needed?
Trauma- Ottawa Rules
-
Age
55 or older
-
Isolated
tenderness of the patella
-
Tenderness
at the head of the fibula
-
Inability
to flex the knee to 90 degrees
-
Unable
to bear weight (2 steps with affected leg) both immediately and upon
evaluation
-
Suspected
OCD
-
Obtain
tunnel view, A/P and lateral
-
If
positive, obtain the contralateral side. (Can be bilateral)
-
Suspected
ACL tear
-
R/O
intra-articular fractures – tibial spine
-
R/O
Segond fracture (very small avulsion fracture of the lateral tibial
plateau)
-
Patellar
dislocation- R/O fracture after relocation
-
Multiple
visits without improvement
-
Atypical
presentation
-
R/O
arthritis
When
is MRI needed?
-
To evaluate soft tissue injuries – meniscus, ACL,
PCL
-
Staging of OCD
-
Note: MRI
is not necessary to confirm diagnosis. For example, a patient with suspected meniscal tear by
history and physical can be treated as such.
When is arthrocentesis beneficial?
-
To aid in diagnosis
-
Mandatory when suspecting infection
-
Cell count
-
Glucose
-
Protein
-
Gram Stain
-
Culture
-
R/O gout or pseudo gout
-
Crystal analysis
-
To provide symptomatic relief
-
Trauma
-
To improve examination – relieves tension and can
inject lidocaine
What
if exam is not accurate secondary to patient pain and guarding?
-
If significant ligamentous disruption is suspected
and rapid diagnosis is necessary can do arthrocentesis and inject
joint with local anesthetic and repeat exam.
OR
-
Treat patient conservatively and repeat exam in two
weeks after acute pain subsides.
When
should I refer emergently?
-
Suspected
or confirmed septic joint
-
Infected
prepatellar bursitis not responding to oral antibiotics
-
Knee
dislocation (disruption of multiple ligaments) – vascular status
may be compromised
-
Locked
knee that can not be unlocked
-
Suspected
or confirmed intra-articular fractures
-
Inability
to extend leg (patellar tendon rupture, fractures)
Management
-
Recognize emergencies
-
Septic joint
-
Immediate orthopedic referral for surgical drainage
and antibiotics
-
If unable to Medevac, antibiotics – ceftriaxone and
medevac at earliest possible time
-
Patella dislocation
-
Lateral pressure against patella while extending knee
-
3 weeks of immobilization at 30 degrees of flexion,
quad strengthening
-
Locked joint (meniscus, OCD, loose body)
-
R/O pseudolocking (hamstring spasm, swelling)
-
If unable to unlock joint, consider injecting local
anesthetic and performing ROM. Make sure you are not making an intra-articular fracture
worse.
-
Knee dislocation – relocate and check distal pulses
– can tear popliteal vessels – surgical emergency
-
Acute
trauma. If no x-ray or
other diagnostic capabilities available, follow acute trauma
guidelines until able to perform. Often, as with internal derangement, definitive diagnosis may
be delayed until acute effusion and pain have resolved.
Acute management - PRICEMM
-
Protection - Range of motion bracing
-
Rest - May require crutches if significant pain or
instability with weight bearing.
-
Ice – 20 minutes t.i.d.
-
Compression – Ace wrap may help control excess edema
-
Elevate – above heart if possible
-
Meds - NSAIDS for pain and inflammation
-
Modalities – electrical stimulation may help reduce
pain and inflammation
After acute pain resolves, obtain definitive
diagnosis and continue appropriate rehabilitation
-
Range
of motion
-
Strengthening
-
Endurance
Overuse
Injuries
Sharon
Burnham, DO, and Scott D. Flinn, MD
For further information, read:
Sports
Related Injury Management, in the General Medical Officer Manual
Home
· Military Medicine
· Sick Call · Basic Exams
· Medical Procedures
· Lab and X-ray · The Pharmacy
· The Library · Equipment
· Patient Transport
· Medical Force
Protection · Operational Safety · Operational
Settings · Special
Operations · Humanitarian
Missions · Instructions/Orders · Other Agencies · Video Gallery
· Forms · Web Links · Acknowledgements
· Help · Feedback
Approved for public release;
Distribution is unlimited.
Bureau of Medicine and Surgery
Department of the Navy
2300 E Street NW
Washington, D.C
20372-5300 |
Operational Medicine
Health Care in Military Settings
CAPT Michael John Hughey, MC, USNR
NAVMED P-5139
January 1, 2001 |
United States Special Operations
Command
7701 Tampa Point Blvd.
MacDill AFB, Florida
33621-5323 |
*This web version is provided by The Brookside Associates, LLC. It contains
original contents from the official US Navy NAVMED P-5139, but has been
reformatted for web access and includes advertising and links that were not
present in the original version. The medical information presented was reviewed and felt to be accurate in 2001. Medical knowledge and practice methods may have changed since that time. Some links may no longer be active. This web version has not been approved by the
Department of the Navy or the Department of Defense. The presence of any
advertising on these pages does not constitute an endorsement of that product or
service by either the US Department of Defense or the Brookside Associates. The
Brookside Associates is a private organization, not affiliated with the United
States Department of Defense.
© 2015, Brookside Associates, LLC. All rights reserved
Other Brookside Products
|
|