|
|
|||||
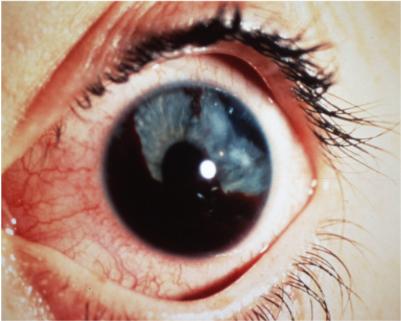
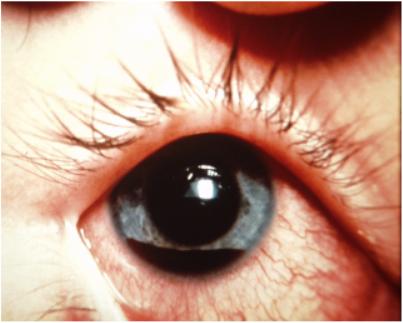
HyphemaDefinition: Blood in the anterior chamber (front part) of the eye. This can be a macrohyphma (grossly detectable) or microhyphema
(microscopic-magnification needed to observe)
Signs/Symptoms:
Causes: Generally occur with trauma associated with fighting, and
sports. Occasionally
spontaneous and can sometimes be seen with diseases like diabetes.
Differential Diagnosis:
Evaluation:
Treatment:
Prognosis:
This section provided by CAPT Robert B. North, Jr., MC, USN
Home · Military Medicine · Sick Call · Basic Exams · Medical Procedures · Lab and X-ray · The Pharmacy · The Library · Equipment · Patient Transport · Medical Force Protection · Operational Safety · Operational Settings · Special Operations · Humanitarian Missions · Instructions/Orders · Other Agencies · Video Gallery · Forms · Web Links · Acknowledgements · Help · Feedback Approved for public release; Distribution is unlimited.
*This web version is provided by The Brookside Associates, LLC. It contains original contents from the official US Navy NAVMED P-5139, but has been reformatted for web access and includes advertising and links that were not present in the original version. The medical information presented was reviewed and felt to be accurate in 2001. Medical knowledge and practice methods may have changed since that time. Some links may no longer be active. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the US Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense.
© 2015, Brookside Associates, LLC. All rights reserved |
|
||||