|
Medical Education Division |
Operational Medicine 2001
Standard First Aid Course
NAVEDTRA 13119



Basic Life SupportAtmospheric air that is essential for life contains approximately 21% oxygen. When you breathe in (inhale) only a quarter of the air is taken by the blood in the lungs. The air you breath out (exhale) contains approximately 16% oxygen. Enough to support life! Seconds after being deprived of oxygen, the heart is at risk of developing irregular beats or stopping. Within four to six minutes, the brain is subject to irreversible damage. Basic life support is maintenance of the ABCs (airway, breathing, and circulation) without auxiliary equipment. The primary importance is placed on establishing and maintaining an adequate open airway. Airway obstruction alone may be the emergency: a shipmate begins choking on a piece of food. Restore breathing to reverse respiratory arrest (stopped breathing) commonly caused by electric shock, drowning, head injuries, and allergic reactions. Restore circulation to keep blood circulating and carrying oxygen to the heart, lungs, brain, and body. This course is not a substitute for formal training in basic life support. Airway Obstruction Airway obstruction, also known as choking, occurs when the airway (route for passage of air into and out of the lungs) becomes blocked. The restoration of breathing takes precedence over all other measures.. The reason for this is simple: If a casualty cannot breathe, he or she cannot live. Individuals who are choking may stop breathing and become unconscious. The universally recognized distress signal (Fig. 2-1) for choking is the casualty clutching at his or her throat with one or both hands. The most common causes of airway obstruction are swallowing large pieces of improperly chewed food, drinking alcohol before or during meals, and laughing while eating. The tongue is the most common cause of obstruction in the casualty who is unconscious. A foreign body can cause a partial or complete airway obstruction. Partial Airway Obstruction If the casualty can cough forcefully, and is able to speak, there is good air exchange. Encourage him or her to continue coughing in an attempt to dislodge the object. Do not interfere with the casualty's efforts to remove the obstruction. First aid for a partial airway obstruction is limited to encouragement and observation. When good air exchange progresses to poor air exchange, demonstrated by a weak or ineffective cough, a high-pitched noise when inhaling, and a bluish discoloration (cyanosis) of the skin (around the finger nails and lips), treat as a complete airway obstruction. Complete Airway Obstruction A complete airway obstruction presents with a completely blocked airway, and an inability to speak, cough, or breathe. If the casualty is conscious, he or she may display the universal distress signal. Ask "Are YOU choking?" If the casualty is choking, do the following: 1. Shout "Help"-Ask the casualty if you can help. 2. Request medical assistance - Say "Airway is obstructed" (blocked), call (Local emergency number or medical personnel).
Figure 2-1 Universal Distress Signal
Figure 2-2 Abdominal Thrust 3. Abdominal thrusts (Heimlich Maneuver)
If the casualty becomes unconscious, do the following:
Figure 2-3 Abdominal Thrust
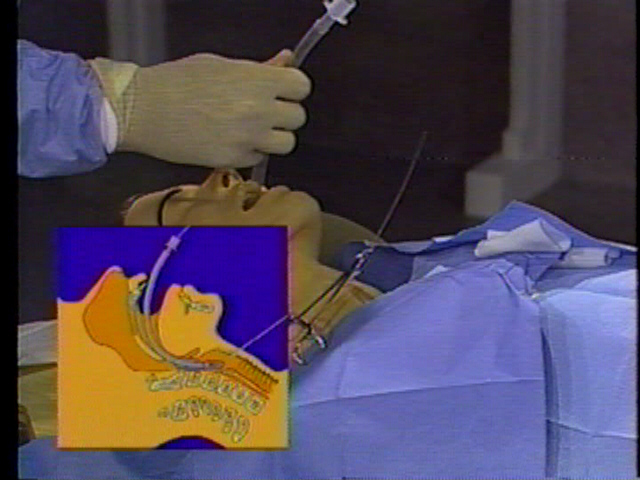
Figure 2-4 Head Tilt-Chin Lift 4. Finger sweep - Place the casualty on his or her back, open casualty's mouth and grasp the tongue and lower jaw between your thumb and fingers, lift jaw with your index finger into the mouth along inside of cheek to base of tongue. Use "hooking" motion to dislodge object for removal. 5. Open airway (Head-tilt/Chin-lift) -Place your hand on the casualty's forehead. Place the fingers of your other hand under the (Fig. 2-4) bony part of the chin. Avoid putting pressure under the chin, it may cause an obstruction of the airway. Tilt the head and lift the jaw, avoid closing the casualty's mouth. Place your ear over the casualty's mouth and nose. Look at the chest, listen and feel for breathing, 3 to 5 seconds. If not breathing, say, "Not Breathing." (jaw-thrust maneuver) - If you suspect the casualty may have an injury to the head, neck, or back, you must minimize movement of the casualty when opening the airway. Kneeling at the top of the casualty's head, place your elbows on the surface. Place your fingers behind the angle of the jaw or hook your fingers under the jaw, bring (Fig. 2-5) jaw forward. Separate the lips with your thumbs to allow breathing through the mouth. Note that the head is not tilted and the neck is not extended.
Figure 2-5 Jaw Thrust 6. Give breaths - Pinch nose, open your mouth, take a deep breath, and make an air-tight seal around the casualty's mouth. Give 2 full breaths, each lasting 1 to 1 1/2 seconds. Pause between each breath. If unsuccessful, perform abdominal thrusts. 7. Perform abdominal thrusts
8. Continue steps 4 to 7 -Until successful, you are exhausted, you are relieved by another trained individual, or by medical personnel. If the casualty is found unconscious, do the following: 1. Check unresponsiveness - Tap or gently shake the casualty, shout, "Are you OK?" 2. Shout, "Help" - If there is no response from casualty. 3. Position casualty - Kneel midway between his or her hips and shoulders facing casualty. Straighten legs, and move arm closest to you above casualty's head. Place your hand on the casualty's shoulder and one on the hip. Roll casualty toward you as a unit, move your hand from the shoulder to support the back of the head and neck. Place the casualty's arm nearest you alongside his or her body.
Figure 2-6 Abdominal Thrust Reclining 4. Open airway (Head-tilt/Chin-lift or Jaw-thrust) - Place your hand on the casualty's forehead. Place the fingers of your other hand under the bony part of the chin. Avoid putting pressure under the chin, it may cause an obstruction of the airway. Tilt the head and lift the jaw, avoid closing casualty's mouth. Place your ear over the casualty's mouth and nose. Look at the chest, listen, and feel for breathing, 3 to 5 seconds. If not breathing, say, "Not Breathing." 5. Give breaths - Pinch nose, open your mouth, take a deep breath, and make an air-tight seal around the casualty's mouth. Give 2 full breaths, each lasting 1 to 1 1/2 seconds. Pause between each breath. If unsuccessful, reposition head, and give 2 full breaths. 6. Request medical assistance - Say "Airway is obstructed" (blocked), call local emergency number or medical personnel. 7. Perform abdominal thrusts
8. Finger sweep - Place the casualty on his or her back, open the casualty's mouth and grasp the tongue and lower jaw between your thumb and fingers, lift jaw, insert your index finger into the mouth along the inside of cheek to base of tongue. Use "hooking" motion to dislodge object for removal. 9. Give breaths - Pinch nose, open your mouth, take a deep breath, and make an air-tight seal around the casualty's mouth. Give 2 full breaths, each lasting 1 to 1 1/2 seconds. Pause between each breath. 10. Continue steps 7 to 9 - Until successful, you are exhausted, you are relieved by another trained individual, or by medical personnel. Chest Thrusts The chest thrust is the preferred method, in place of the abdominal thrust, for individuals who are overweight or pregnant. Manual pressure to the abdominal area in these individuals can be ineffective or cause serious damage. If the casualty is overweight or pregnant, do the following: 1. Conscious - Standing or Sitting.
2. Unconscious - Lying.
Repeat the last three steps until the obstruction is clear, you are exhausted, you are relieved by another trained individual, or by medical personnel. Self Abdominal Thrusts If you are alone and choking, try not to panic, you can perform an abdominal thrust (Fig. 2-7) on yourself by doing the following: 1. With the fist of your hand, place the thumb side against the middle of your abdomen, above the navel and below the tip of the breastbone. Grasp your fist with your other hand and give a quick upward thrust. 2. You also can lean forward and press your abdomen over the back of a chair (with rounded edge), a railing, or a sink.
Figure 2-7 Self-Help for Airway Obstruction If the casualty is not breathing, do the following: Rescue Breathing Rescue breathing is the process of breathing air into the lungs of a casualty who has stopped breathing (respiratory arrest), also known as artificial respiration. The common causes are air-way obstruction, drowning, electric shock, drug overdose, and chest or lung (trauma) injury. Never give rescue breathing to a person who is breathing normally. 1. Check unresponsiveness - Tap or gently shake the casualty, shout, "Are you OK?" 2. Shout, "Help" - If there is no response from casualty. 3. Position casualty - Kneel midway between his or her hips and shoulders facing the casualty. Straighten legs and move arm closest to you above casualty's head. Place your hand on the casualty's shoulder and one on the hip. Roll casualty toward you as a unit, move your hand from the shoulder to support the back of the head and neck. Place the casualty's arm nearest you alongside his/her body. 4. Open airway (Head-tilt/Chin lift or Jaw thrust) - Place your hand on the casualty's forehead. Place the fingers of your other hand under the bony part of the chin. Avoid putting pressure under the chin, it may cause an obstruction of the airway. Tilt the head and lift the jaw, avoid closing the casualty's mouth. Place your ear over the casualty's mouth and nose. Look at the chest, listen, and feel for breathing, 3 to 5 seconds. If not breathing, say, "Not breathing." 5. Give breaths - Pinch nose, open your mouth, take a deep breath, and make an air-tight seal around the casualty's mouth (Fig. 2-8). Give 2 full breaths, each lasting 1 to 1 1/2 seconds. Pause between each breath. Look for the chest to rise, listen, and feel for breathing. 6. Check pulse - While maintaining an open airway, locate the Adam's apple with your middle and index fingers. Slide your fingers down into the groove (Fig. 2-9), on the side closest to you. Feel for a carotid pulse for 5 to 10 seconds. If you feel a pulse, say, "No breathing, but there is a pulse." Quickly examine the casualty for signs of bleeding.
Figure 2-8 Mouth-to-Mouth Ventilation
Figure 2-9 Check Carotid Pulse 7. Request medical assistance - Say "No breathing, has a pulse," call (Local emergency number or medical personnel). 8. Rescue breathing (mouth-to-mouth) Maintain an open airway with head-tilt/chin-lift or jaw-thrust maneuver, pinch nose. Open your mouth, take a deep breath, and make an air-tight seal around the casualty's mouth. Give 1 breath every 5 seconds, each lasting 1 to 1 1/2 seconds. Count aloud "one one-thousand, two one-thousand, three one-thousand, four one-thousand," take a breath, and then give a breath. Look at the chest, listen, and feel for breathing. Continue for 1 minute/12 breaths. 9. Recheck pulse - While maintaining an open airway, locate and feel the carotid pulse for 5 seconds. If you feel a pulse, say, "Has pulse." Look at the chest, listen, and feel for breathing 3 to 5 seconds. If the casualty is not breathing, say, "No breathing." 10. Continue sequence - Maintain an open airway, give 1 breath every 5 seconds, recheck pulse every minute. If pulse is absent, begin CPR. If pulse is present but breathing is absent, continue rescue breathing. If the casualty begins to breathe, maintain an open airway, until medical assistance arrives. Special Situations 1. Air in the stomach (Gastric Distention) - During rescue breathing and CPR, air may enter the stomach in addition to the lungs. To avoid this, keep the casualty's head tilted back, breathe only enough to make the chest rise, and do not give breaths too fast. Do not attempt to expel stomach contents by pressing on the abdomen. 2. Mouth-to-nose breathing - Used when the casualty has mouth or jaw injuries, is bleeding from the mouth, or your mouth is too small to make an air-tight seal. Maintain head tilt with your hand on the forehead, use your other hand to seal the casualty's mouth and lift the chin. Take a deep breath and seal your mouth around the casualty's nose and slowly breathe into the casualty's nose using the procedures for mouth-to-mouth breathing. 3. Mouth-to-stoma breathing - Used when the casualty has had surgery to remove part of the windpipe. They breathe through an opening in the front of the neck, called a stoma. Cover the casualty's mouth with your hand, take a deep breath, and seal your mouth over the stoma and slowly breathe using the procedures for mouth-to-mouth breathing. Do not tilt the head back. (In some situations a person may breathe through the stoma as well as his or her nose and mouth. If the casualty's chest does not rise, you should cover his or her mouth and nose and continue breathing through the stoma). 4. Mouth-to-mask breathing - Used when rescue breathing is required in a contaminated environment, such as after a chemical or biological attack. A resuscitation tube is used to deliver uncontaminated air to the casualty. This resuscitation tube has an adapter at one end that attaches to your mask and a molded rubber mouthpiece at the other end for the mouth of the casualty. 5. Dentures - Leave dentures in place, they provide support to the mouth and cheeks during rescue breathing. If they become loose and block the airway or make it difficult to give breaths, remove them. Circulation Circulation is the movement of blood through the heart and blood vessels. The circulatory system consists of the heart, which pumps the blood, and the blood vessels, which carry the blood throughout the body. Cardiac arrest is the failure of the heart to produce a useful blood flow or the heart has completely stopped beating. The signs of cardiac arrest include unconsciousness, the absence of a pulse, and the absence of breathing. If the casualty is to survive, immediate action must be taken to restore breathing and circulation. Cardiopulmonary Resuscitation (CPR) is an emergency procedure for the casualty who is not breathing and whose heart has stopped beating (cardiac arrest). The procedure involves a combination of chest compressions and rescue breathing. The casualty must be lying face up on a firm surface. Do not assume that a cardiac arrest has occurred simply because the casualty appears to be unconscious. This course is not a substitute for formal training in cardiopulmonary resuscitation (CPR).
Figure 2-11 Xiphoid Process Chest Compressions
Continue CPR - If the casualty has no pulse, give 2 full breaths and continue CPR. Check for a pulse every few minutes. If the pulse is present but breathing is absent, continue rescue breathing. If the casualty begins to breathe, maintain an open airway until medical assistance arrives. Continue CPR until successful, you are exhausted, you are relieved by another trained in CPR, by medical personnel, or the casualty is pronounced dead. Do not interrupt CPR for more than 7 seconds except for special circumstances. CPR with Entry of Second Person When a second person who is trained in administering CPR arrives at the scene, do the following: 1. The second person shall identify himself or herself as being trained in CPR and that they are willing to help. ("I know CPR. Can I help?") 2. The second person should call the local emergency number or medical personnel for assistance if it has not already been done. 3. The person doing CPR will indicate when he or she is tired; and should stop CPR after the next 2 full breaths. 4. The second person should kneel next to the casualty opposite the first person, tilt the casualty's head back, and check for a carotid pulse for 5 seconds. 5. If there is no pulse, the second rescuer should give 2 full breaths and continue CPR. 6. The first person will monitor the effectiveness of CPR by looking for the chest to rise during rescue breathing and feeling for a carotid pulse (artificial pulse) during chest compressions. CPR for Children and Infants If the casualty is an infant (0-1 year old) or child (1-8 years old), do the following: 1. Check unresponsiveness - Infant: Tap or shake shoulder only. Child: Tap or gently shake the shoulder, shout, "Are you OK?" 2. Shout, "Help" - If there is no response from infant or child. 3. Position casualty - Turn casualty on back as a unit, supporting, the head and neck. Place casualty on a firm surface. 4. Open airway (Head-tilt/Chin-lift or jaw thrust) - Place your hand on the casualty's forehead. Place the fingers of your other hand under the bony part of the chin. Avoid putting pressure under the chin, it may cause an obstruction of the airway. Tilt the head and lift the jaw, avoid closing the casualty's mouth. Infant: Do not overextend the head and neck. Place your ear over the casualty's mouth and nose. Look at the chest, listen, and feel for breathing, 3 to 5 seconds. 5. Give breaths - Open your mouth, take a breath, and make an air-tight seal around the casualty's mouth and nose. Give 2 breaths (puffs for infants), each lasting 1 to 1 1/2 seconds. Pause between each breath. Look for the chest to rise, listen, and feel for breathing. 6. Check pulse - While maintaining an open airway, locate the carotid pulse (Infants: Locate the brachial pulse (Fig. 2-13) on the inside of the upper arm, between the elbow and shoulder). Feel for a pulse for 5 to 10 seconds. Quickly examine the casualty for signs of bleeding. 7. Request medical assistance - If someone responded to your call for help, send them to call the local emergency number or medical personnel. 8. Chest compressions (infant) -
9. Chest compressions (children) -
10. Continue CPR - If the infant or child has no pulse, give 1 breath and continue CPR. Check for a pulse every few minutes. If the pulse is present but breathing is absent, continue rescue breathing (Infant: 20 breaths/min; Child: 15 breaths/min.) If the infant or child begins to breathe, maintain an open airway, until medical assistance arrives. Continue CPR until successful, you are exhausted, you are relieved by another trained in CPR or medical personnel, or the infant or child is pronounced dead. This course is not a substitute for formal training in cardiopulmonary resuscitation (CPR). References 1. Instructors Manual for Basic Life Support, American Heart Association, ISBN
0-87493-601-2
Department of the Navy Approved for public release; Distribution is unlimited. The listing of any non-Federal product in this CD is not an endorsement of the product itself, but simply an acknowledgement of the source. Operational Medicine 2001 Home · Military Medicine · Sick Call · Basic Exams · Medical Procedures · Lab and X-ray · The Pharmacy · The Library · Equipment · Patient Transport · Medical Force Protection · Operational Safety · Operational Settings · Special Operations · Humanitarian Missions · Instructions/Orders · Other Agencies · Video Gallery · Phone Consultation · Forms · Web Links · Acknowledgements · Help · Feedback
*This web version is provided by The Brookside Associates Medical Education Division. It contains original contents from the official US Navy NAVMED P-5139, but has been reformatted for web access and includes advertising and links that were not present in the original version. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the US Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense. |