|
Emergency War Surgery NATO Handbook: Part IV: Regional Wounds and Injuries: Chapter
XXII: Craniocerebral Injury
Operative Management of Open and Penetrating Wounds
United States Department of Defense
Treatment is carried out in the following order:
-
The head is shaved and the wound inspected. X-rays are examined to determine the
distribution of bone and metallic fragments.
-
Endotracheal intubation and general anesthesia are preferable in most cases. Adequate
blood is made available for wounds near major dural venous sinuses.
-
The scalp is scrubbed with an antiseptic solution, preferably an iodophor. The wound is
copiously irrigated with 1-2 liters of sterile saline.
-
The patient is positioned and draped so that entry and exit wounds are accessible and a
contralateral burr hole can be made if needed. The head should be elevated slightly above
heart level, to encourage venous return, but not so high as to risk air embolism.
-
Devitalized scalp and foreign bodies are removed. Incisions are made along lines that
can be utilized to rotate the scalp, should it become necessary to perform plastic repair
of the scalp. As much scalp as possible is preserved.

Figure 29 A
-
Contaminated pericranium is removed. Burr holes are made in intact bone adjacent to the
area of damage. A margin of normal dura is exposed. Bone is removed with rongeurs toward
the area of contamination.
Figure 29 B
Figure 29 C
-
Contaminated dura is removed, preserving as much as possible for closure.

Figure 29 D
-
Damaged brain, blood clots, and foreign bodies are removed with gentle saline irrigation
and suction. Removal of all bone fragments is of greater importance than removal of all
metal fragments. The use of intraoperative ultrasound facilitates localization of
fragments. The debrided track should remain open after debridement. Closure of the track
suggests the presence of deeper or adjacent clot or necrotic brain tissue exerting
pressure on the track.
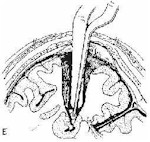
Figure 29 E
With high velocity injuries, there is more destruction at the wound of
exit than the wound of entry, and debridement of the exit wound initially may provide the
most rapid decompression. Complete hemostasis is accomplished before closure.
The brain is copiously irrigated with normal saline solution containing 1000u/l
bacitracin at body temperature. A concentrated bacitracin solution (500u/cc) should be
used to irrigate the track.
-
Massive swelling of the brain is an uncommon but serious occurrence during operation
that may represent the development of an intracerebral hematoma or a contralateral
subdural hematoma. It may also represent an anesthetic complication or loss of
autoregulation of the cerebral vasculature After determining that there is no technical
difficulty with anesthesia, swelling is treated in a stepwise fashion by increasing the
ventilatory rate to obtain a PaCO2 of about 25mm Hg, by tapping the ventricle
and draining CSF and by administering barbiturates. Pentobarbital sodium, 100-300 mg, is
given intravenously. Additional doses of 100 mg may be required hourly. If the brain is
swollen at the time of closure, an intracranial pressure monitoring catheter is placed,
preferably intraventricularly, and the intracranial pressure is monitored in the
post-operative period.
-
The dura is closed without tension. Dural grafts may be harvested from pericranium,
temporalis fascia, or fascia lata.
-
The scalp is closed primarily without tension. Rotation of scalp flaps with closure of
the secondary defect with split-thickness skin grafts or a myocutaneous pedicle flap may
be necessary.
-
Post-operative X-rays or CT scans are obtained to check for the presence of retained
fragments.
-
The need for reoperation for retained fragments is a difficult judgment call that
requires much experience. It need not be done routinely if optimal follow-up neurosurgical
and CT scan capability is anticipated.
Approved for public release; Distribution is unlimited.
The listing of any non-Federal product in this CD is not an
endorsement of the product itself, but simply an acknowledgement of the source.
Operational Medicine 2001
Health Care in Military Settings
Bureau of Medicine and Surgery
Department of the Navy
2300 E Street NW
Washington, D.C
20372-5300 |
Operational Medicine
Health Care in Military Settings
CAPT Michael John Hughey, MC, USNR
NAVMED P-5139
January 1, 2001 |
United States Special Operations Command
7701 Tampa Point Blvd.
MacDill AFB, Florida
33621-5323 |
This web version is provided by
The Brookside Associates Medical Education Division.
It contains original contents from the official US Navy NAVMED P-5139, but has
been reformatted for web access and includes advertising and links that were not
present in the original version. This web version has not been approved by the
Department of the Navy or the Department of Defense. The presence of any
advertising on these pages does not constitute an endorsement of that product or
service by either the US Department of Defense or the Brookside Associates. The
Brookside Associates is a private organization, not affiliated with the United
States Department of Defense.
Contact Us · ·
Other Brookside
Products
|