|
|
General
Medical Officer Manual: Clinical Section
Operational Dermatology*
|
|
Home
· Military Medicine
· Sick Call ·
Basic Exams
· Medical Procedures
· Lab and X-ray ·
The Pharmacy
· The Library ·
Equipment
· Patient Transport
· Medical Force
Protection ·
Operational Safety ·
Operational
Settings ·
Special
Operations ·
Humanitarian
Missions ·
Instructions/Orders ·
Other Agencies · Video Gallery
· Phone Consultation
· Forms ·
Web Links · Acknowledgements
· Help ·
Feedback |
|
|
|
|
|
General
·
Prevention/Minimization of Skin Disease
·
Hot/Humid Areas
·
Cold Weather Operations
·
Miliaria (Prickly Heat)
·
Intertrigo
·
Acne
·
Furuncles (Boils)
·
Impetigo
·
Herpes Simplex (HSV)
·
Herpes Zoster
·
Varicella (Chickenpox)
·
Inclusion Cysts
·
Pseudofolliculitis Barbae (PFB)
·
Verrucae (Warts)
·
Condyloma
·
Molluscum Contagiosum
·
Eczema and Contact
Dermatitis
·
Psoriasis
·
Seborrheic Dermatitis
·
Scabies
·
Lice (Head and Body)
·
Tinea Pedis/Cruris (Athlete's
Foot/Jock Itch)
·
Tinea Capitis
·
Tinea Versicolor
·
Basal Cell Carcinoma
·
Melanoma
·
Actinic Keratosis
·
Pityriasis Rosea
·
Urticaria/Angioedema
(1)
General
Believe it or not, rare or exotic dermatoses are not the skin conditions
that create the greatest difficulty for deployed military personnel.
In fact, only about 20 or so conditions induce the majority of
outpatient dermatologic visits and generate the lion's share of morbidity.
Under field conditions, common dermatoses may have unusual clinical
appearances or become more severe than what is encountered in routine
"in garrison" or "in port" care.
This chapter of the GMO Manual is not just for Navy providers.
The intended audience is the primary care providers of all U.S. Armed
Forces. It is meant to
supplement but not replace the commonly available dermatologic textbooks,
online atlases, therapeutic manuals, PDR and CD-ROMs.
It does however contain diagnostic and therapeutic "pearls"
that are most useful to military primary care providers in an operational
setting.
The chapter is restricted to conditions that are highly prevalent or
produce disproportionate morbidity in a deployed military population.
(2)
Prevention
and Minimization of Skin
Disease
The old adage that “an ounce of prevention is worth a pound of cure”
is when applied to dermatologic conditions in the field. The presence of extremes of head and cold along with fewer
opportunities for personal hygiene and clothing change have been the
traditional enemies of deployed military personnel. Military unique dermatology can be thought of as a battle of
the Sailor and Marine versus the hostile environment.
Included below are some prevention tips for hot and cold climates written
by the U.S. Army in plain language for field troops.
Some phrases are quoted verbatim in the next few paragraphs.
This simple wisdom applies to any person in any of the Armed Forces.
These words are just as true today as when they were written.
(3)
Hot
and Humid Areas
These tips were published in 1977 by the US Army in a small field manual
entitled: FM 8-40 "Management of Skin Diseases in the Tropics at Unit
Level".
(a)
Keep the skin clean.
"Cleanliness helps preserve
the skin's health. Bathing
removes dirt, decreases the number of microorganisms and lessens body
odor. For all these reasons, keeping clean is preferable to
remaining dirty. In addition,
showers are great for relaxation, morale and personal comfort."
"If bathing facilities are
not handy, they (your personnel) can keep quite clean by washing with cold
water from their helmets. Potable
water is preferable for showers, but if not available, nonpotable water is
adequate."
"Soap and water must be
used judiciously and properly. Whatever
soap is used must be rinsed off completely.
As to the type of soap to use, scientific evidence does not support
the notion that germ killing or deodorant soaps or detergents reduce the
incidence of bacterial or fungal infections."
"Soldiers (military
personnel) must not shower excessively, such as three showers a day with
lots of lather. Too much soap
and water removes the skin's moisteners and protective oils, causes the
skin to become dry and irritated, and thereby reduces the skin's capacity
to protect the body."
"Even though cleanliness
helps preserve the skin's health, bathing cannot perform miracles in
preventing skin disease. This
is true regardless of the brand of soap used or the number of showers
taken."
(b) Keep the skin dry.
"Tropical skin diseases
would be greatly reduced if another rule of skin hygiene, keeping the skin
dry, could be adhered to."
"The realities of combat
and (other) military operations often make this difficult, but there are a
few rules to follow:"
"Remove wet socks and boots
as frequently as possible. If
dry socks are not available, wring out the wet ones."
"Rinse mud off boots.
Mud on boots prevents (the leather) from drying."
"Pay special attention to
the skin fold areas; the
armpits, groin, buttocks, and the areas between the toes, where several
common skin diseases can erupt. Dry
these areas frequently. In
addition, get in the habit of using talcum (or other nonfragranced)
powder. These two practices
will promote drying, reduce friction, and prevent infections."
"Do not starch jungle
fatigues (BDUs). Starch clogs
the openings in the cloth, blocks sweat from escaping, and therefore
prevents sweat from evaporating and cooling the skin."
"Air the skin as much as
conditions permit."
"If underwear is
aggravating an existing skin condition, do not wear it."
"In base camp, encourage
the wearing of as little clothing as the commander will allow.
Under some conditions, commanders may permit clothing, such as
shortened fatigue (BDU) pants, tennis shoes or shower clogs, at base camp
and particularly in the company area.
It is the commander's responsibility to prescribe the uniform,
however. The medic (medical
personnel) can only recommend a uniform that is consistent with command
policy."
“Unless you are reasonably
sure the patient has a fungal or bacterial infection, it is better to
soothe the skin than to “kill the germs”.
More damage can be done by “over treatment” than by under
treatment. As a rule, highly
inflamed, blistered, or oozing areas require gentle and calmative
treatment. The application of
wet soaks (e.g. Burow's solution), removal of restrictive clothing, can
encourage the patient to stop scratching by eliminating the itching.”
(4)
Cold
Weather Operations
These quotes are from the US Army
TC 21-3 (1986) "Soldier's Handbook For Individual Operations and
Survival In Cold-Weather Areas". This
1986 version is easily understood.
(a) Keep it Loose
"All items of the
cold-weather uniform are large enough to allow wearing of the appropriate
number of layers (of clothing). Your
field jacket may appear too large without all of the layers designed to
fit under it. If the uniform
items do not fit loosely, the insulation that keeps you warm (a layer of
warm air) will be greatly reduced."
(b)
Keep it dry
"It is important to keep
clothing dry, since wet clothing conducts heat away from the body more
quickly than dry clothing. Moisture
soaks into clothing from two directions: the inside and the outside. From the outside you must guard against melting snow; from
the inside you must guard against sweating.
Brush snow and frost from clothing before entering any heated
shelter or vehicle, and avoid overheating."
(5)
The Cold Weather Uniform
"The feet are hard to keep
warm and dry, so protect them."..."When you are active, your
feet will sweat and....the moisture will remain in the socks or in the
bottom (and leather) of the boots. Drying (the feet), massaging with foot
powder, warming and putting on dry socks will correct
this."..."Don't wear socks that are too
tight."..."Change your socks at least twice a day."
Dermatologic
Conditions
(6)
Miliaria
(Prickly Heat)
This common condition is most frequently seen in service members who have
been recently put in hot, humid environments.
The trunk is commonly involved.
Wearing occlusive clothing and military gear further exacerbates the
effects of the climate. As a
result, the patient does not sweat onto the skin.
Instead, he or she sweats "into" the skin.
The most common form seen in the deployed military population is little
discrete pink to red itchy papules on the trunk.
Besides being a nuisance, the presence of miliaria reduces the
service member's ability to cope with heat stress.
Removal of the occlusive clothing, thereby allowing the skin to air is
effective yet simple. The use
of calamine lotion with 1 % hydrocortisone
as a shake lotion is effective for relief of symptoms.
The good news is that most personnel will spontaneously resolve after
acclimatization.
(7)
Interigo
and Irritancy in Body Folds (Crotch Rot, Pit Rot)
Perspiration as well as other skin
irritants (e.g. soap residue, petroleum products, sawdust, fiberglass
etc) can collect in body folds and cause an irritant dermatitis.
The condition is most commonly seen in patients in whom the
body folds predispose to trap moisture and irritants rather than vent
to the air. As you can
imagine, service members who are constitutionally sweaty, who serve in
hot, sweaty places, doing hot sweaty things or who are pregnant
(figure 1) are more prone to this condition.
In addition, what starts as a simple case of Interigo may, with
time, become secondarily colonized with Staph and/or Candida.
The best way to prevent interigo is the use of hygienic measures
outlined above. Strongly
counsel your patient not to be overzealous in personal hygiene
measures. Recommend avoiding over the counter (OTC) remedies and harsh
soaps. If it occurs
despite these measures, the use of mild topical corticosteroids (e.g.
hydrocortisone or desonide cream) should be considered.
(8)
Acne
All acne treatments require several weeks to
work. Your patient will not
wake up with a clear face tomorrow, next week or even next month.
Be patient!
Patients
should not "squeeze their zits" because it may enhance scarring
and will delay resolution of the manipulated lesion.
Dietary effects on acne are inconsistent at best.
If your patient repeatedly breaks out a couple of days after eating a
certain food, tell him/her to avoid it.
However, the complexions of most patients are not affected by diet.
(a)
Comedonal (predominantly
blackhead/whitehead acne)
Benzoyl Peroxide
Benzoyl peroxide (BOP) products are available in wash, gel, or cream
forms. All of these products
will bleach colored fabrics. Use
the BOP washes in place of and exclusive of any other facial soaps or
cleansers. They should be used
as one would use a liquid soap washing using only fingertips or lightly with
a white washcloth and rinsed thoroughly.
The gel or cream BOP preparations should be applied just before sleep
and left on overnight.
Benzoyl peroxide products will
induce some drying. If you
decide to start a patient on a wash and a gel/cream together, remember that
you may end up inducing quite a bit of irritation (see Facial Dryness below).
Retinoids:
Tretinoin (Retin-A)
Another alternative is the vitamin
A derivative tretinoin. Facial
irritation and dryness are the usual limiting factors for this medication.
Most of the time this can either be avoided or minimized if some
simple common sense guidelines are followed.
Start using the lower concentration
of the appropriate medication. For patients with very greasy
complexions, the 0.01% gel (green label) is appropriate while the 0.025% cream
(gray label) is better tolerated by average complexions. Application
should be just before sleep waiting at least 20-30 minutes after washing the
face. Significant facial irritation, dryness, and scaling can be
practically guaranteed if this is ignored. Only a "pea sized"
amount of Retin-A is needed to cover a face and forehead. Avoid the skin
immediately adjacent to the mouth, nose, and eyes.
A mild amount of irritation will
occur and can usually be controlled (see Facial Dryness below). Another way to minimize irritation is to have your patient
use Retin-A every other night for 2 weeks before advancing to every night
treatment.
Retin-A is not a true
photosensitizer in the classic sense of the word.
It does however make the face more sensitive to all potential irritants
such as sunlight, wind, salt water, fragrances, and/or irritating vapors.
Retin-A will make acne worse for a
several weeks before it begins to improve.
If your patient tolerates the initial therapy, you can advance after
3-4 months to the 0.025% gel or the 0.05% cream as appropriate.
If your patients complain about
excessive irritation from Retin-A, ask them in some detail how they are using
the product. You may be quite surprised to find that they have either never
been told how to correctly use it or just have not followed the directions.
Alternative
topical retinoids such as microsphere tretinoin and adapalene gel (Differin®)
are niche products that are not widely used due to their expense.
Ensure that your patient has CORRECTLY used Retin-A before trying these
products.
(b) Facial Dryness and Irritation
from Acne Therapy
Topical acne therapy will always
create some mild dryness and irritation.
It is usually easily controlled with a non-fragranced facial lotions
(e.g. Purpose Facial Lotion, Lubriderm etc.) applied once or twice a day.
Some facial drying is acceptable;
a lot of dryness and irritation is not acceptable.
If severe drying or irritation occurs, your patient needs to stop the
treatment.
(c) Papulopustular Acne (red
pimples, pustules, no cysts)
Benzoyl
peroxide products are appropriate (as above).
(d)
Topical
Antibiotics
These
must be applied twice a day to be effective.
Most of them are compounded in water/alcohol based solutions (Cleocin-T,
T-Stat, Staticin, and Erycette Pads) and will induce some drying.
Patients with complexions that are prone to dryness (or who also have
seborrheic dermatitis) should use Cleocin-T Lotion instead of the
water/alcohol products. Patients
taking disulfuram (Antabuse) should not use these water/alcohol products.
(e)
Azaleic Acid
A newer product is 20% azeleic acid
cream. This is a niche product
primarily meant for resistant cases of simple papulopustular, inflammatory
acne. This product is quite
expensive and will have only limited use in a primary care setting.
(f)
Oral Antibiotics
These
are appropriate for patients with substantial numbers of inflamed acne lesions
and a few small cysts.
Tetracycline
Tetracycline is the old standby.
Unfortunately, it must be taken 1 hour before eating or 2 hours after
eating... a real inconvenience. Particularly
avoid dairy products, iron, and certain antacids.
These interfere with the intestinal absorption of the medication.
Start with 250 mg BID advancing to 250 mg (2) BID if needed.
Side effects to consider are mostly G-I upset and candida vaginitis.
Photosensitivity, while reported, is not a frequent problem.
Whether or not the tetracyclines
interfere with the action of oral contraceptives is controversial. It would be prudent to counsel the patient about this issue
and broach the possibility of using a supplemental form of contraception.
The patient who has been previously stable on oral contraceptives
should immediately report the new appearance of “spotting” to you.
This potential problem has not been reported with Depo-Provera or
Norplant.
Doxycycline
This cousin of tetracycline has the
advantage of being able to be taken with food (although not large amounts of
dairy products, or mineral supplements).
In fact, taking it on an empty stomach is usually rewarded by G-I
upset. As with all oral
antibiotics, vaginal candidiasis is a possibility.
The starting dose is 100 mg per day advancing to 100 mg BID if
necessary.
Photosensitivity is a real
possibility with this drug. It
should be used with caution to those with significant sunlight exposure.
Although it appears to be allowed by the Naval Aerospace Medical
Institute (NAMI) for patients in flight status, a review of the current NAMI,
Air Force, or Army flight medicine "allowable medications" list is
highly advised. If in doubt,
consult a flight surgeon from the appropriate service.
It is not to be given to those in undersea status or patients in whom
large exposures of ultraviolet light are probable.
Minocycline
This is another first cousin of
tetracycline that should be taken with food as above.
The side effect spectrum is the same as other tetracyclines. The
risk of photosensitivity is much less than doxycycline.
Headaches and vertigo are a real possibility.
The starting dose is 100 mg per day advancing to 100 mg BID if
necessary. It is contraindicated
for aviation or undersea personnel in the Navy.
Erythromycin
This drug is best given on an empty
stomach with two glasses of water. However,
if G-I upset occurs, it can be given with a small amount of food, but about 20
percent of the drug will not be absorbed.
Vaginal candidiasis is a possibility.
The starting dose is 250 mg BID, advancing to 500 mg BID if needed.
Beware of multiple
drug interactions: theophylline,
digoxin, terfenadine, astemizole, loritidine, coumadin, barbiturates,
phenytoin, and carbamazepine. Check
the PDR for details.
(g)
Other Oral Antibiotics
While many other antibiotics have
been used in the treatment of acne, their use is probably best initiated by a
dermatologist.
(h) Other Oral
Medications
The use
of medications to modify the hormonal milieu of acne is probably best left to
the specialist.
(i)
Nodulocystic Acne
Use of the medications above should
be considered initially. Oral
medications should be used at the higher doses listed above. If the patient does not respond within 2-3 months, a
dermatology consult is appropriate. The
use of isotretinoin (Accutane) may be indicated.
The decision to use isotretinoin is
not a casual one and should be left to a dermatologist.
This medication has predictable morbidity and teratogenicity as well as
requiring monthly follow-up visits and lab testing (including serum pregnancy
testing in women). The risk of
teratogenicity in pregnant women is exceptionally high.
There are also several
military-unique considerations to using this medication.
In addition to the predictable dryness and skin fragility, frequent
musculoskeletal side effects will further degrade combat readiness of
personnel in a large number of military occupations.
The dermatologist is obligated to coordinate this treatment and follow
up with the service member's operational primary care provider.
(9)
Boils (Furuncles)
If the lesion is fluctuant, incise and
drain it. If not yet fluctuant, hot
soaks three times a day are appropriate to "bring it to a head".
Oral antistaphylococcal antibiotics (preferably beta
lactams) are
indicated for 10 days (e.g. dicloxacillin 500 mg QID).
The majority of these lesions are staphylococcal and as such pose a
public health risk in an operational setting if not aggressively treated.
In particular, these patients should not be food handlers until treatment
is complete.
(10) Impetigo
This rapidly spreading, highly
contagious condition should be aggressively treated topically and systemically.
The oozing lesions should be dried with Burow's Solution (1 tablet
dissolved in 1 pint of water) used as a compress for 5 to 10 minutes, 3 times a
day.
Topical antibiotic ointments
are optional. Systemic anti-staph
drugs are your safest option.
Like
a furuncle, impetigo is a public health hazard.
These patients should not be food handlers until resolved.
If the impetigo is on the central face, examine carefully to see if the
lesions represent secondarily infected herpes simplex.
(11) Herpes
Simplex (HSV), oral and genital
If there is a question of diagnosis,
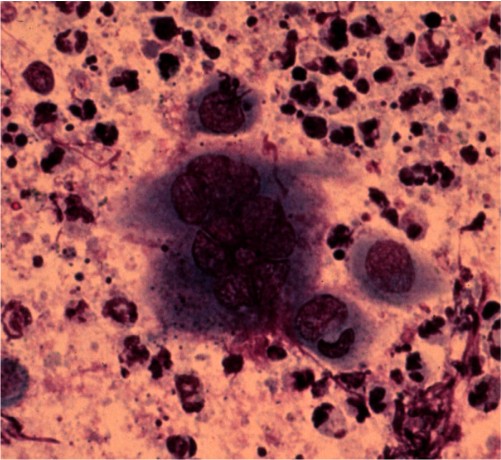
do a Tzanck smear (see technique below). While
oral or genital HSV is usually painful, this is not always the case.
Be suspicious, especially with penile erosions and ulcers.
Treatment should be individualized.
Topical acyclovir ointment is useless.
Tea bag soaks are quite helpful to dry out the blisters. Have the patient make a cup of tea, squeeze out the teabag,
and then apply the bag to the lesions after it has cooled.
The residual tannic acid in a tea bag is a surprisingly effective drying
agent.
(a) Acyclovir
Oral acyclovir is effective only if
given EARLY in the herpetic episode. In
addition, it is not useful for the patient who gets only the occasional mild
episode. Acyclovir is helpful for
patients with an initial outbreak. They
are frequently systemically ill and in pain.
For patients with recurrent disease,
acyclovir should be reserved for those patients whose outbreaks are frequent,
very painful, or have associated systemic findings (fever, painful adenopathy,
malaise, etc.) The dose for
treatment of an acute episode is 200 mg five times a day for 5 days.
The use of 200 mg TID to 400 mg BID is useful for suppression in
patients with frequent recurrences.
(b) Valacyclovir
This drug is a pro-drug of acyclovir.
Its mechanism of action is identical to acyclovir.
The advantage is that the medication needs to only be used twice a day
instead of five. The dose for recurrent HSV is 500 mg BID for 5 days.
The use of 500 mg QD is useful for suppression.
(c)
Famcyclovir
The dose is 125 mg BID for 5 days.
(d)
Other Considerations
In the case of genital HSV,
evaluation for concomitant STD should be strongly considered on an initial
visit. STDs are a chummy group
and are frequently transmitted in twos or threes.
Look for them!
Although patients are most
infectious when they have active lesions, they may continue to shed virus
(albeit at a smaller rate) between outbreaks. As such, barrier contraception (e.g. condoms) is recommended at all
times unless a couple is trying to conceive.
A couple trying to determine
"who gave what to whom and when" is engaged in a hopeless and
psychologically destructive task. Either partner may have had a dormant
infection for weeks, months or even years. While serologic testing for antibodies to HSV I and II is available, a
positive result is of little clinical utility because over 90 percent of
adults will test positive due to previous exposure to oral or genital HSV.
Instructions for performing a Tzank Smear
-
Open an intact vesicle at the edge using a surgical blade. If no
intact vesicles, gently soak off the crust.
-
Scrape the base of the vesicle (or the advancing border from an
erosion/ulcer after crust soaked off) and smear on slide. Do not
scrape to the point of bleeding, it makes the slide difficult to
interpret.
-
Fix the slide using heat or 20 seconds in absolute alcohol.
-
Stain using Wright, Wright-Giemsa, Pap, etc. stains following the
lab's standard operating procedures manual.
-
Dry the slide using gentle blotting motions of a paper towel and air
movement.
-
Place 2 small drops of immersion oil on slide and then mount a cover
slip.
-
Scan under 10-X for presence of multinucleated giant cells.
(12)
Zoster
The presence of itchy or painful vesicles on an erythematous base in a
dermatomal distribution should be considered Zoster (shingles) until proven
otherwise. Use a Tzanck smear (see
Herpes Simplex above) to confirm the diagnosis.
Thoracic segments are the most frequently affected.
The branches of the trigeminal nerve are also frequently involved and can be
quite painful. The ophthalmic
branch in particular is quite problematic.
For patients with cranial nerve V1 involvement, be sure to ask
about eye symptoms and do examine the eye.
Keratoconjunctivitis and/or iridocyclitis are potentially serious
complications. Consult with an
ophthalmologist.
Treatment of Zoster is threefold in nature:
antiviral medications (if indicated), pain relief, and drying of the
vesicles. Acyclovir 800 mg orally
five times a day is helpful only if given with 48 hours of the onset of the
rash. The appropriate doses of
valacyclovir and famcyclovir are 1000 mg TID and 500 mg TID respectively.
The pain can be quite severe; prescribe narcotics if required.
The use of Burow's solution to compress the vesicles (see Impetigo above)
is soothing and will desiccate the blisters.
While the vesicular fluid of zoster lesions is minimally contagious, this is
usually not a problem in immunocompetent patients.
Patients can return to work with active vesicles as long as the involved
area is covered with clothing.
(13) Varicella
This condition is highly contagious and can cause a great deal of morbidity
in the active duty age group. Even
though the varicella vaccine is now commonly in use, there are still many
service members who are susceptible.
For Chickenpox, treat the active duty age group with acyclovir 800mg 5 times
a day for 10 days if the condition is recognized within 2-3 days of onset of
rash. The course of the illness can
be somewhat shortened. Unfortunately,
it is unclear whether the serious complications of varicella (e.g. pneumonitis,
meningoencephalitis, etc.) can be prevented with therapy.
(14) Epidermal
Inclusion Cysts (Sebaceous Cysts)
If the cyst is inflamed and fluctuant, surgically drain it.
Larger amounts of local anaesthetic than expected are usually required to
deaden the skin before incision and drainage.
After irrigation and removal of all visible cyst wall, pack it with iodoform
gauze and let it granulate. Premature
closure of the surgical wound is counterproductive...let it drain.
Antibiotics are optional because this is not initially an infectious
process. A few weeks later,
evaluate the site to see if any cyst remains and consider the feasibility of
elliptical excision.
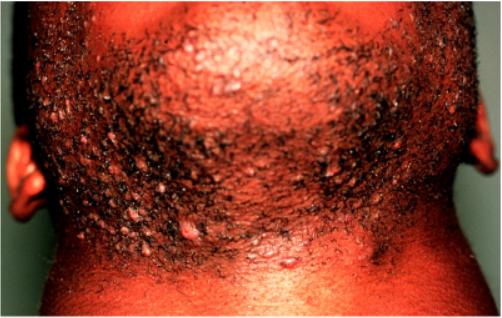
(15) Pseudofolliculitis
Barbae (PFB)
Although this is mostly an administrative problem, it is of importance to
the operational primary care provider.
The Department of Defense does not require clean shaven faces merely for the
sake of military appearance.
Grooming is important because bearded faces have greater difficulty in
obtaining gas tight seals on a gas mask or oxygen breathing apparatus. The practice of liberally giving "no shave chits" besides
being unprofessional may actually harm your patient in certain operational
situations. BUPERS instruction
1000.22 and Marine Corps Order 6310.1B outline the current program and
administrative procedures including the phases of therapy and how to properly
use them.
Although some patients truly must grow short, well-trimmed beards as the only
way to control their PFB, the majority of motivated patients can be helped by
simple measures. Most PFB patients
are quite motivated, but need your interest and guidance. Your attention to this frequently misunderstood problem will
reap great rewards. You will be
rewarded by the respect of your patients and better clinical results.
First of all, make sure that the patient truly has PFB. Some patients may also have coexistent acne, which is
worsened by the act of shaving. Examine
the skin carefully. Treatment of
PFB alone in the presence of coexisting acne is doomed to failure. Both conditions must be approached simultaneously.
Most cases of PFB require a period of no shaving to give the inflamed hairs a
change to grow out to let the inflammation die down.
Mild cases may require only 2 weeks of "no shave" whereas more
severe cases frequently need 4 weeks or longer. Impacted hairs can be delicately dislodged during this period
by gently massaging them (barely touching the face) using a circular motion with
an extra soft toothbrush.
Once grooming is resumed, remember that the goal is to have some
"stubble" remain on the problematic areas.
This is done by "shaving with the grain", whether one is using
a PFB razor, electric razor, beard clipper, or removing with a chemical
depilatory. Going "against the
grain" defeats the whole strategy of leaving "stubble" because
the hairs would be cut shorter. The
act of hair removal is more physically irritating to the skin.
Chemical depilitory products can play a role in some, but not all patients.
Several patients prefer to use these products despite an unpleasant smell during
their use. The most widely
available of several commercial products is Magic Shave.
The instructions on the container need to be explicitly followed or else
an irritant dermatitis will almost always occur. Even if properly used, many patients develop a mild tightness
and chapping of the face and neck. Be careful.
(16)
Verrucae
Everybody dislikes warts. Warts
are a challenge for both you as well as your patient.
Remember that the family of wart viruses is a lot smarter than we are.
Even after the wart is visibly gone, virus persists in the skin and may
recur later.
Make sure that both you and your patient have realistic expectations for
treatment. Your goal is to minimize
your patient's morbidity and encourage the immune system to control the
infection. Permanently ridding your
patient of the wart virus is not possible.
Overly aggressive therapy is usually only rewarded with extra morbidity
and is frequently not more likely to be successful.
Warts are passed between humans commonly in "communal" settings
such as berthing compartments, recreational facilities, and equipment.
Wear shower shoes, T-shirts, and weight lifting gloves to avoid exposure
and the spread of warts to others.
The most common encountered morbidity from warts (especially on the feet) is
pain. The pain is not caused by the
wart itself, but rather by the mass effect of having a hard knot within and on
top of the skin. Gently paring the
wart with a scalpel blade just barely to the point of pinpoint bleeding is an
easy way to debulk it, thereby decreasing the patient's discomfort as well as
preparing the site for other treatment. Control
any bleeding by applying Monsell's solution or 20% Aluminum chloride solution (DrySol).
Common treatments for warts whether chemical, electrical, or surgical are
skin destructive in nature.
Chemical salicylic acid wart varnishes (e.g. Duofilm, Occlusal HP, Compound
W, etc.) should be applied to the wart daily, preferably at bedtime.
Consider protecting the surrounding normal skin by applying petrolatum.
Place two or three coats on the wart, allowing each coat to dry; then
apply a bandaid. Salicylic acid
plasters (e.g. Mediplast) should be cut to fit the wart and then applied at
bedtime and overlaid with a bandaid. The
next day, the lesion can be pared or abraded with an Emory board or pumice
stone. Stop treatment if there is
substantial pain, irritation, or ulceration.
Trichloroacetic acid solution (TCA) can be used similar to the salicylic acid
preparations, but has a larger potential for tissue destruction.
Use it with respect.
Liquid nitrogen, if applied optimally, will induce a small blister allowing
the wart to peel away from the underlying dermis. Freeze the wart quickly to the point of turning it white with
a 1 mm zone of normal skin. A good
method to minimize the damage to surrounding normal skin is to apply an
appropriately sized otoscope speculum and spray the nitrogen through the open
end. Let the wart thaw slowly, then
repeat the freeze.
After freezing, the lesion will follow this sequence over the next few days:
pink, red, purple, brown, and then maybe even black.
A blister will likely form and should be approached as any other blister.
Once the vesicle has opened and dried, pare off any remainder
and see if any lesion remains. Repeat
treatment should be considered every 1-2 weeks or so if any lesion remains.
Electrosurgery should be used only if you have had some training in its use.
It can generate a fair degree of post-operative morbidity.
Areas over joints, near the nails, or over the bony prominences are
particularly difficult to treat.
Chemical vesicants such as cantharidin are quite destructive and are not
recommended as initial therapy.
(17)
Condyloma
Like other warts, subtypes of human papilloma virus also cause these lesions.
Like other warts, the infection is a lifelong one.
Sexually transmitted diseases such as condylomata love company.
Make sure that your patient does not have other STDs.
Evaluation for other STDs (e.g. syphilis, urethritis, and HIV) should be
considered on the initial visit.
Once a patient has had condylomata, the skin always sheds virus to some
degree. As such, barrier
contraception (e.g. condoms) is recommended unless a couple is actually trying
to conceive. The question of who
gave the virus to whom is not a useful one.
The virus may have been shed asymptomatically by either partner for quite
some time before lesions develop.
The goal is to make your patient free of visible warts for as long as
possible. Eradication of the virus
from the skin is impossible. Destructive
modalities delivered with precision such as liquid nitrogen, Trichloroacetic
acid, electrosurgery, and podophyllin are helpful.
Podophyllin resin in tincture of benzoin has long been a mainstay of therapy.
Apply it to external lesions (do not apply to vaginal or cervical warts
in women or use during pregnancy) and wash off with soap and water after 4 - 6
hours. Re-evaluate your patient 1
week after treatment to determine whether additional therapy is necessary.
A new form of podophyllin (Condylox) is commercially available and should
only be considered for emotionally mature, dexterous, and reliable patients.
The active ingredient is podofilox, a purified and standardized form of
podophyllin toxin suitable for self-application by a patient.
Podofilox is meant only for external condylomata and should not be used on
mucous membrane lesions or during pregnancy in females. Follow the PDR recommendations carefully because over
treatment will result in considerable irritation.
This should be applied only to lesional skin. This medication is also quite expensive.
It is not meant for everyone.
Other pharmacologic means to treat condylomata include biologic response
modifiers such as topical imiquimod cream (Aldara) and intralesional interferon.
These modalities are very costly and are only considered appropriate for
treatment when prescribed by Dermatologists.
(18)
Molluscum
Contagiosum
A DNA containing pox virus causes these
lesions. When seen in the
active duty population, they are frequently sexually transmitted.
As such, they are usually found on or near the genitalia, inner
thighs, and waistline areas. Clinically
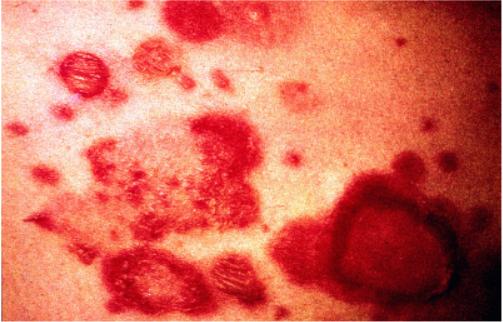
the lesions are asymptomatic 1-5 mm umbilicated milky papules (figure 3).
Treatment is best accomplished with destructive modalities such as
liquid nitrogen, light curettage, or light electrodessication.
The precise pinpoint application of salicylic acid wart varnish
(protecting the normal skin with petrolatum) covered by a band aid is an
alternative.
Vesicant agents,
such as cantharidin, are best avoided by primary care providers unless
they are quite experienced in the technique.
(19)
Eczema
and Contact Dermatitis
(a)
Administrative Notes
Hand eczema (endogenous and
exogenous), atopic dermatitis, and other forms of eczema are the second
most costly form of dermatologic, occupationally aggravated, or induced
"illness" in the civilian world and DoD. In particular, endogenous hand eczema and atopic dermatitis
are notoriously unpredictable.
For this and other reasons these
conditions are disqualifying for entry into the United States Armed
Forces. If present in a
currently serving member, these conditions are considered to be
disqualifying for aviation, submarine, and Special Forces duty as well as
other specialized military duty.
Why is this so?
The actuarial data of many decades gives us the answer. Even if a
patient's eczema has been minimally active (or even totally quiescent)
this is not an accurate predictor of future severity.
Military dermatologists (like our civilian occupational dermatology
colleagues) routinely encounter many patients whose "minimal"
eczema ultimately flared badly in the military or special occupational
environment.
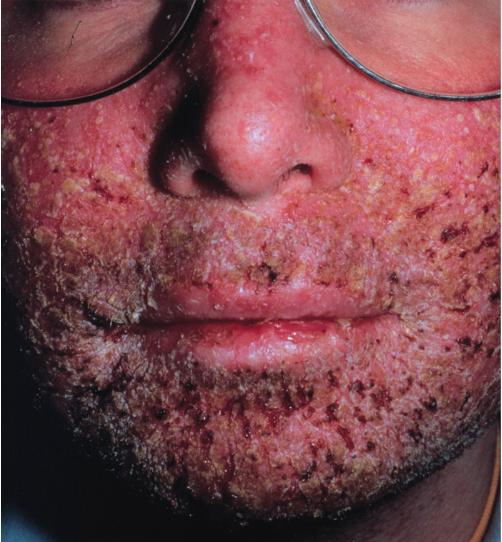
Figures 4 and 5 illustrate such
a case of Atopic Dermatitis in a Navy Mess Management Specialist. His eczema flared very badly during Operation Desert
Shield/Storm, ultimately impetiginized and was the source of an outbreak
of Staph food poisoning.
Figure 6 illustrates a case of a
man with known Dyshidrotic Eczema of the hands who was granted a medical
waiver for enlistment. His
hands flared very badly during his training as a jet engine mechanic.
He was ultimately medically separated from the Navy.
This group of skin diseases
causes a great deal of morbidity, lost productivity and administrative
burden to the military. Waivers
for entry in a patient with known endogenous eczema or hand dermatitis
should be rarely granted, only after thoughtful deliberation.
Please remember this fact if you are doing entry physicals or
special duty qualification exams.
(b)
Treatment
The treatment of eczema can be
likened to be a three legged footstool.
If you remove one or more of the legs, the footstool will not
stand. The same is true for
eczema therapy. The three
legs of this therapeutic footstool are lubrication, medication, and
control of the skin's environment.
Lubrication of dry eczematous
dermatitis can be done with a wide variety of emollients, the simpler the
better. Frequent use of bland
products such as Eucerin, Aquaphor, or Vaseline is preferable to the more
expensive fragrance containing and chemically complex products.
Fragranced products, while "elegant", are potential irritants
and/or allergens and should be avoided on irritated skin of any kind, but
especially in patients with eczema.
The medication leg of the footstool
usually involves topical steroids. The
advice here is similar; keep it simple. Topical
steroids are available in a variety of potencies and vehicles.
In general, do not use medium potency or higher products on the face or
genitals. Gels or aerosolized steroid sprays are appropriate for moist
and weepy dermatitis. Creams and
ointments are effective on drier more chronic lesions.
While topical steroid "allergies" do occur, the reactions to
topical steroid medications more likely represent a sensitivity to a
preservative, fragrance, or other ingredient in the vehicle.
Medication of acute or "wet"
eczema (e.g. poison ivy or flare of atopic or dyshidrotic eczema of the hands)
has additional considerations. Burow's
Solution compresses (see Impetigo) can dry out a wet oozing eczema within a few
days. Decrease the bacterial
colonization of the eczema with a few days of antistaphyloccal antibiotic
therapy.
Systemic steroids are reserved for
cases of substantial morbidity or widespread involvement. If required, use 1 mg/kg of prednisone in a tapering dose
over a 2-3 week period while initiating topical therapy. Shorter courses or lower doses frequently result in
"rebound" of the dermatitis. Otherwise
healthy active duty personnel tolerate brief courses of prednisone very well.
If a patient has reached this point of severity, dermatology consult is
highly advised.
The last leg of the footstool is
environmental control. This simply
means to decrease the skin's exposure to any identified offending substance,
harsh bath soaps, occupationally related chemicals and the like.
Most cases of hand eczema are irritant
or endogenous (i.e. a form of atopic dermatitis) rather than allergic. The
proper use of protective gear (e.g. work gloves), minimizing repeated wet/dry
exposures of the involved area etc will allow the skin to heal faster.
Here is a diagnostic "pearl"
concerning eczematous dermatitis on the foot. If vesicles are present,
especially on the plantar surface, do a KOH (potassium hydroxide) prep on the
roof of a vesicle. If positive, the therapeutic strategy involves
antifungal therapy. Eczematous dermatitis exclusively on the dorsum of the
foot is usually not fungal.
(20)
Psoriasis
(a) Administrative Aspects
Like atopic dermatitis and endogenous hand eczema, psoriasis and its variants
are listed as disqualifying for entry and the pursuit of certain special duty in
the Armed Forces of the United States. The reasons are the same as eczema;
the notorious unpredictability of the condition. A case of clinically
banal psoriasis can sometimes explode into disease of a debilitating nature in
the military environment. Waivers should be very judiciously granted for
this condition only after consultation with a military dermatologist.
The "three legged stool" of medication, lubrication, and
environmental control applies equally well to the treatment of psoriasis (see
Eczema above). The novice primary care practitioner inappropriately
neglects lubrication in favor of potent topical steroids. Psoriasis
perpetuates itself on dry cracked skin. Moisturize, moisturize, and
moisturize! Topical steroids are not a substitute for emollients.
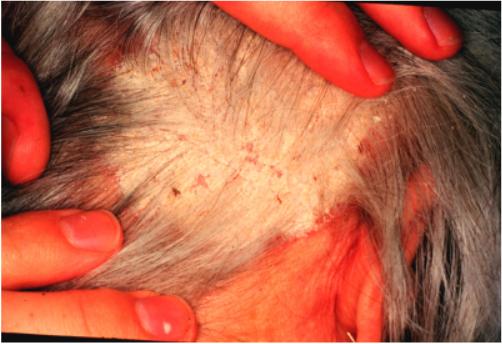
Scalp lesions are best approached with sulfur/salicylic acid, zinc pyrithione,
or coal tar based medicated shampoos. The key to success here is
sufficient contact time. The shampoo must have several minutes in place on
the scalp before rinsing. There are a large number of generic and
proprietary products on the market: Tarsum, T-Gel, Pentrax, Sebulex, Sebutone,
and other dandriff shampoo brands to name but a few.
Ketoconazole shampoo is also useful, but is best saved for situations where
conventional shampoos do not help. This product is very expensive and
should be used judiciously.
Topical steroid lotions (e.g. betamethasone valearate 0.1%) applied after
shampoo are a nice way to deliver medication to lesions within and near hair
bearing surfaces such as the scalp and eyebrows.
Do not use systemic steroids to control psoriasis. An impressive
"rebound" usually occurs which can be very difficult to treat.
(21)
Seborrheic
Dermatitis
Scalp lesions (i.e., dandruff) are treated the same as psoriasis (see
Psoriasis above). The areas of
greasy scale with background erythema on the central face, forehead,
retroauricular, genitalia, and periumbilical locations should be treated with a
low potency steroid cream or ointment (e.g., hydrocortisone 1% or desonide
0.05%).
(22)
Scabies
The itching and rash associated with scabies
is not due the infestation per se but are the consequence of the body's
immune response to the presence of the mite and its waste products.
Consider the diagnosis of scabies in any a patient with a
smoldering itchy rash with itchy papules on the genitalia, web spaces, or
wrists.
Some patients will have few if any symptoms with their infestation.
While a positive scabies scrape preparation taken from a typical
"burrow" is diagnostic, it is frequently negative, even in a
"classic" case (figure 7).
While conceptually simple,
the treatment of scabies is sometimes difficult to execute properly in practice.
Do not use Kwell shampoo to treat scabies...it won't work.
Use Kwell cream/lotion or Elimite cream at bedtime exactly as written in
the PDR.
Thirty to sixty grams of the cream or 60-120 ml of lotion should cover the
whole body. Be sure to treat from
the neck all the way to the toes being sure to get every crack and crevice in
between. Be sure to apply the
medication to the web spaces, underneath the fingernails, and the genitalia.
Do not wash the hands or fingers before going to sleep.
Retreat the patient the following evening.
The itching usually takes a few days to subside.
All scabies medications are somewhat irritating and drying to the skin.
Use bland emollients or if necessary medium potency topical steroids
after the second application is rinsed off to control residual irritation and
dryness.
All clothing, underwear and nightclothes, linen and towels used in the past 2
weeks by the patient require washing in hot water or dry cleaning.
All household and/or sexual contacts should be treated.
Aboard ship or in a barracks or any other very "close living"
situation, persons nearby should be checked carefully for evidence of
infestation. If in doubt, treat the
patient.
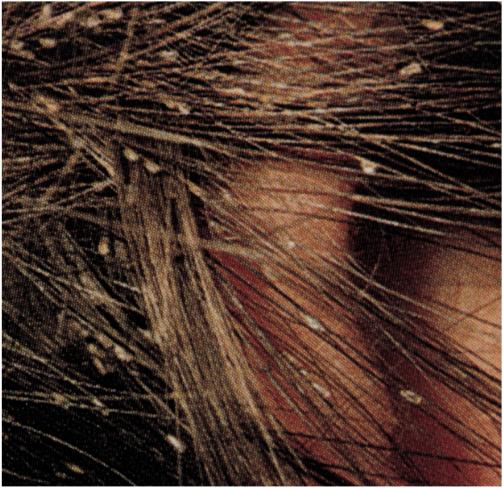
(23)
Lice
(head or crab)
Like scabies, the presence of one patient with
lice should prompt the search for other cases involving personnel who are
billeted nearby. Look around,
you might be surprised what you discover.
The washing of involved clothing in water greater than 50 degrees
celsius will kill the lice and any nits.
Use Kwell, Nix or Rid shampoos, or similar products. Adequate pre-cleaning followed by adequate medication contact
time is the key. The hair
should be routinely shampooed clean and toweled dry (i.e. moist but not
dripping wet) before the application of the pediculocide shampoo.
The pediculocide shampoo should be directly applied from the bottle onto the
affected areas and worked into lather without the addition of water.
Kwell shampoo should have at least 4-5 minutes and other products about
10 minutes of contact time before rinsing off with water.
Retreat one week later. Treatment
failure is not due to resistant lice. The
pediculocides available today do not kill nits as well as they kill live lice. Treatment failure is most frequently due to reinfestation or
inadequate contact time.
If treating the scalp, be sure to treat behind the ears and the base of the
neck. It is very easy to
inadequately treat patients with long hair.
Longer haired patients should use a plastic shower cap to insure
coverage. Avoid the eyes.
Nits can be removed with a nit comb or picked off with tweezers (see figure
8). Rinsing the hair with a 2:1
dilution of table vinegar before combing will help loosen the nits.
Combs and brushes should be soaked in the pediculocide shampoo for about
an hour or heated to about 65 degrees Celsius for 5-10 minutes.
The treatment of crab lice should not just involve the pubic hair.
It should also cover the hairy skin from the umbilicus down to mid thigh.
In particularly hairy individuals, check the axilla and chest for
involvement.
Lice on the eyelashes can be treated by thickly applying Vaseline 2-3 times a
day for a week. This treatment
smothers the lice. Ammoniated
Mercury ointment 0.1% applied to the lids is also quite effective. The nits can
then be mechanically removed.
(24)
Fungal
Infections
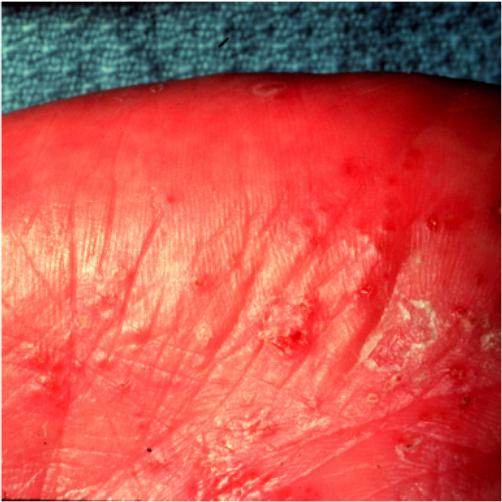
(a) Tinea Pedis and Cruris
Not all that is red, itchy, and scaly on the feet or groin is
fungal. Be sure to consider
other causes such as contact dermatitis, eczema, and bacteria.
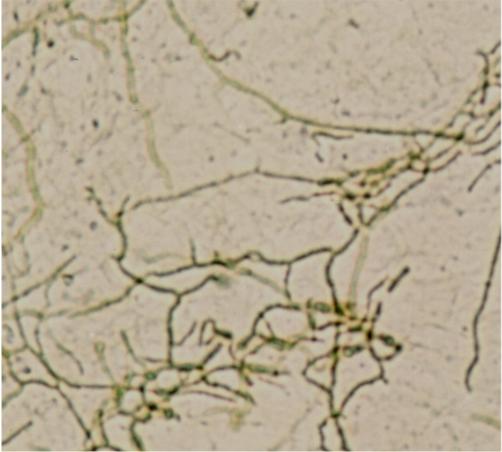
Take a KOH preparation from the scaly advancing border of a groin rash or
from scaling on the feet adjacent to (but not within) an area of maceration,
or the roof of a vesicle on the foot to confirm the diagnosis. Branching
hyphae should be visible (figure 9).
Fungus lives where it is wet, warm, and dark.
The groin and foot are ideal locations for growing fungus.
Control of the milieu is important to controlling tinea.
Potent medications are not a substitute for simple preventative
measures to make the fungus less welcome. Web spaces and groins should be thoroughly dried after
gently showering, followed by applying simple antifungal powders containing
tolnaftate or miconazole. Shoes
should fit well and socks should be frequently changed. If possible, two sets of
routine footwear should be maintained; one for odd days, one for even days.
In this fashion, the shoes will dry out on the "off day".
Sweating of the feet can be treated with antiperspirants such as aluminum
chloride solution (e.g. DrySol, Xerac AC, or Certain Dri) applied at bedtime.
Boxer shorts are preferable to briefs... especially if wearing BDUs.
If tinea develops, remember to use the preventive
steps outlined previously in addition to the treatment plan. These actions
will make the treatment much more effective, provide more rapid relief, and
allow for better results over the long run.
Wet, very macerated tinea of the web spaces is
best treated with antifungal lotions such as miconazole or clotrimazole
after astringent compresses with Burow's solution (see Impetigo above) or
dilute vinegar. These areas
are frequently overgrown with a potpourri of gram negative bacteria
(figure 10). The concurrent
use of a drug such as oral ciprofloxacin accelerates recovery.
Typical web space tinea is treated with a cream or solution vehicle
antifungal drug. Miconazole
or clotrimazole are effective. Nizoral, Spectazole, Naftin, or Lamasil cream is also
effective but quite a bit more expensive.
At least 3 weeks of treatment are required. Chronic, hyperkeratotic, cracked and
peeling "moccasin foot" tinea is treated with keratolytics such as
Whitfield's ointment, 10% salicylic acid in petrolatum or 12% ammonium lactate
lotion (Lachydrin). Antifungal creams are also effective but are quite a
bit more expensive. Localized vesicular plantar tinea can be treated with
cream. Extensive vesicular tinea of the feet requires the addition of
astringent soaks (see above) and strong consideration of oral antifungal therapy
(see below).
Not all itchy perineums and groins are
caused by tinea. Strongly consider the diagnosis of Candida if
"satellite pustules" and extensive maceration are present, especially
in females. The differential diagnosis frequently includes contact
dermatitis (occupational and non-occupational), seborrheic dermatitis, and
psoriasis. Take a history and look for diagnostic hints. Remember,
in temperate climates Tinea and Candida rarely involve the scrotum.
Contact dermatitis as an overlay to
another diagnosis on the genital and crural skin occurs more often than is
appreciated. Patients with itchy groins are desperate to stop the itch and
will try anything topical; topical benzocaine, deodorants, rubbing
alcohol, strong antibacterial soaps, and Ben Gay to name a few. Insist
that all applications be ceased except the ones that you prescribe. Wet
and weepy groins need astringent solution compresses and ventilation to
facilitate drying.
If the diagnosis is tinea cruris,
begin with twice a day antifungal cream once if the area is not weeping.
Treat for at least 3 weeks. Remember
that nystatin powder, cream or lotion, while effective for Candida, will not
work against the dermatophyte fungi which cause tinea.
If the tinea is very macerated, strongly consider using oral antifungal
therapy (see below) as well as astringent solution compresses.
The diagnosis of Tinea of the nails (tinea
unguium) needs to be confirmed before you even consider treatment.
Not all distorted nails are due to fungal infection.
If you are not sure of the diagnosis, refer to dermatology.
Tinea unguium is not worth treating
and will only rarely be permanently cured.
While a period of remission can usually be achieved, the fungus usually
returns within 1-2 years. It is
frequently associated with tinea pedis in middle aged or older males who have
some immunologic anergy to the organism (Trichophyton rubrum).
Topical treatment alone will not work.
The use of oral therapy (e.g. griseofulvin, itraconazole, terbenifine)
therapy is frequently ineffective, expensive, and risks some side effects and
drug interactions (especially itraconazole).
Because this condition is prone to recurrence carefully advise the
patient about the various treatment regimens and the realistic potential for an
unsatisfactory result.
| |