Chest X-ray
The Chest X-ray
is probably one of
the most commonly seen plain films, and is one of the most difficult to master.
There are many ways to evaluate the chest.
A systematic approach is usually the best.
One method is described here.

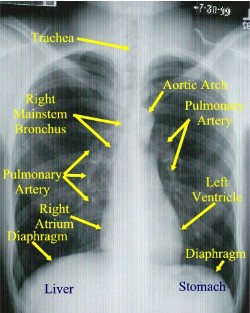
Normal Posterior to Anterior (PA) Chest X-ray
Normally a PA and Lateral View are
obtained. By convention on the PA View, the x-rays enter the patient posteriorly
and exit anteriorly (with the patients chest on the film cassette), therefore
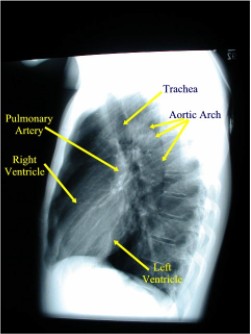
minimizing the cardiac magnification. On the lateral view, the patients left
side is against the film, therefore the right side would be magnified.

Normal Lateral Chest X-ray
How to Read the CXR
-
Get
a mental image of
the patient:
-
Evaluate
soft tissues systematically:
Don’t forget:
-
Evaluate
the lungs (Interstitium, airways and Pleura):
-
Change
your attention to the blood vessels:
-
The
size, location and distribution (the left pulmonary artery usually is
higher the left).
-
Don’t
forget to check the lateral as this is the best way to look at the
posterior costophrenic recess, anterior/posterior mediastinum, and help
you localize lesions suspected on the frontal view.
-
Note
the “Special Interest” and
often missed areas twice:
-
Apices
(esp. RUL- where most
cancer lives)
-
Peripheral
lung margins
-
Hilar,
retrocardiac, cardiophrenic and costophrenic angles.
-
Focus
attention now to the Mediastinum:
Evaluate Size, shape, position in both views PA/LAT.
Attention to the mediastinal lines
-
Heart:
Check both PA/LAT views. Size,
shape, and silhouette. Look for any chamber enlargement.
Evaluate course of Aorta and position of arch, Pulmonary
Arteries.
-
Margin
of SVC (frontal View).
-
Right
Paratracheal Stripe (normal is <5mm, usually 2-3mm), which terminates
at the azygous vein (this portion should be 1.0cm or less). Never
extends below the right bronchus.
-
Left
Subclavian Stripe: Normally 1.0-1.5 cm.
-
On
the lat view, the posterior tracheal wall if seen should measure no more
than 4mm
-
Paraesophageal
line: seen only on the PA view. (interface between right lower lobe and
mediastinal edge along the esophagus/azygous vein – also called the
azygoesophageal line.) It should be straight, bulging could indicate a
node or mass (90% of all localized paraspinal masses are neurogenic
tumors (particularly neruofibromas and ganglioneuromas.)
-
Aorticopulmonary
window: Seen on
frontal view formed by overlap of the Aortic arch and left pulmonary
artery. Space should be
clear as the left upper lobe fills in this area. It should also be
concave, any bulge could signify nodes or mediastinal mass.
-
Bones:
-
Chest wall
-
Bony thorax
including spine.
-
Look for abnormal
joints, bony lytic/blastic or soft tissue lesions,
and free air, etc
Several signs help evaluate
processes:
-
Silhouette sign:
Silhouette sign is extremely
useful in localizing lung lesions.
(e.g. loss of right heart border in RML pneumonia)
-
Air Bronchogram:
As the bronchial tree branches, the cartilaginous rings become thinner and
eventually disappear in respiratory bronchioles. The lumen of bronchus
contains air as well as the surrounding alveoli. Thus usually there is no
contrast to visualize bronchi.
If you see branching
radiolucent columns of air
corresponding to bronchi
, this usually means air-space (alveolar) disease. Usually one of these: blood, pus, mucous, cells, protein.
-
Extra pleural sign:
Signifies Chest Wall disease. Peripheral
location with concave edges.
-
Anatomic landmarks
-
Anterior & Posterior
junction lines: respectively,
the anterior and posterior conjunction of the right and left visceral
and parietal pleural layers at the midline of the thorax.
-
2mm linear line projecting
over the trachea. Note the posterior junction line extends above the
clavicles
This section written by:
LCDR Ron Boucher, MC, USN
LT Hugh McSwain, MC, USN
With some assistance from:
CDR Michael Puckett, MC, USN
ENS Robert Post, MC, USNR
|
|
Approved for public release;
Distribution is unlimited.
The listing of any non-Federal product in this CD is not an endorsement of the
product itself, but simply an acknowledgement of the source.
Bureau of Medicine and Surgery
Department of the Navy
2300 E Street NW
Washington, D.C
20372-5300 |
Operational Medicine
Health Care in Military Settings
CAPT Michael John Hughey, MC, USNR
NAVMED P-5139
January 1, 2001 |
United States Special Operations
Command
7701 Tampa Point Blvd.
MacDill AFB, Florida
33621-5323 |
*This web version is provided by
The Brookside Associates Medical Education Division. It contains
original contents from the official US Navy NAVMED P-5139, but has been
reformatted for web access and includes advertising and links that were not
present in the original version. This web version has not been approved by the
Department of the Navy or the Department of Defense. The presence of any
advertising on these pages does not constitute an endorsement of that product or
service by either the US Department of Defense or the Brookside Associates. The
Brookside Associates is a private organization, not affiliated with the United
States Department of Defense.
Contact Us · · Other
Brookside Products
|
|
Operational Medicine 2001
Contents
|

|