This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
Lesson 9: Newborn Nutrition
Newborn nutrition is a vital part of the well-being of an infant. The period of rapid growth in infancy requires careful nutritional support to continue the growth and development that began at conception. The first decision that parents need to make about feeding their infant is whether to breast-feed, bottle feed, or a combination of both. An early assessment of feeding should have began during the first months of pregnancy. Nutritional information should be provided so that an informed decision can be made. It is important that the parents know that there is a relationship between food and health. They should be given basic information about their infant's nutritional needs and how they relate to breast milk, formula, or solid foods. After the baby is born, feeding practices should be examined, modified where necessary, and reinforced. Proper nutrition is essential for optimal growth and development of the newborn infant.
9-2. NUTRITIONAL REQUIREMENTS OF THE NEWBORN
a. Fluid. Newborns require more fluid relative to their size than adults require. Additional fluids are required with fever, diarrhea, and vomiting.
(1) Dehydration. Until the ability to retain body water through kidney function improves in the early months of life, the infant is at risk for dehydration. Signs of dehydration are:
(a) Depressed fontanels.
(b) Rapid, weak pulse.
(c) Elevated low-grade temperature.
(d) Dark, concentrated urine.
(e) Dry, hard stools.
(f) Dry skin with little turgor.
(g) Elevated specific gravity (1.020).
(2) Water. Prepared infant formulas provide sufficient water under normal environmental conditions. Water intoxication may result from excessive feeding of water to infants. It may occur when water is fed as a replacement for milk. Signs of water intoxication are:
(a) Hyponatremia.
(b) Weakness.
(c) Restlessness.
(d) Vomiting, diarrhea.
(e) Polyuria or oliguria.
(f) Convulsions.
(3) Nursing care.
(a) Maintain accurate input and output (I&O).
(b) Observe frequently for signs of dehydration or water intoxication.
b. Vitamin, Mineral, and Caloric Requirements.
(1) The newborn's rapid growth makes him especially vulnerable to dietary inadequacies and iron deficiency anemia. Adequate vitamin intake is especially important to support normal growth and metabolism. When the mother is well-nourished throughout her pregnancy, the full-term neonate can be expected to have adequate vitamin stores at birth. Calcium and iron are the two basic minerals that are of particular importance in maintaining adequate nutrition.
(a) Calcium is essential for the rapid bone mineralization that takes place during the first year of life, muscle contraction, blood coagulation, nerve irritability, tooth development, and heart muscle action.
(b) Iron is an essential element needed for synthesis of hemoglobin and cell metabolism.
(2) Due to the limited nutritional stores, newborns require vitamin and mineral supplements. An infant may become hypoglycemic and require feeding sooner than normal. His blood glucose is checked at one hour of age and if it is decreased, the baby is first fed sips of water to ensure sucking swallowing coordination and is then fed formula to increase calories and decrease utilization of glucose.
9-3. FIRST FEEDING FROM THE MOTHER
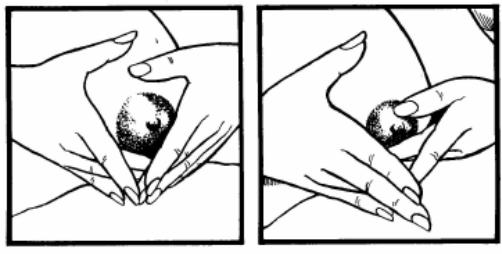
Signs of hunger are demonstrated by the infant searching for food, sucking motions, and crying. The mother may begin to breast-feed at this time if she had planned to breast-feed, her condition is stable, and she desires to feed the infant. See figure 9-1 for common breast-feeding positions

Figure 9-1. Common nursing positions.
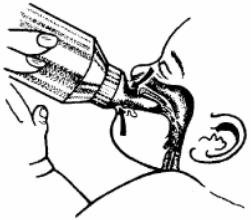
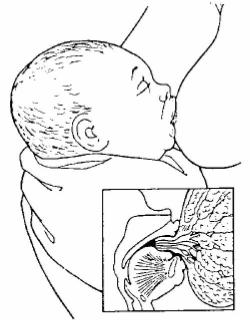
Figure 9-2. Feeding infant.
a. Formula Requirements. A formula must satisfy the infant's requirements for water, calories, vitamins, and minerals. Commercially prepared formulas are made according to established standards.
b. Types of Formulas.
(1) Ready-to-feed. These are liquids packaged in cans and bottles. They are convenient and considered relatively expensive.
(2) Concentrate. These are packaged in cans and are to be diluted 1:1 with water. This is less expensive.
(3) Powder. This must be mixed thoroughly with water and may have difficulty dissolving. This is considered the least expensive.
c. Formula Preparation in the Home.
(1) The choice of method is determined by the type of formula used, the safety of the home water supply, the availability of adequate refrigeration, the ability to utilize the method, and the amount of formula needed each day.
(2) The aseptic method is used when preparing formula. Cleaning the equipment before preparing the formula is essential. Formula is prepared according to directions and bottles assembled. As long as refrigeration is available, any number of bottles may be prepared.
d. Instructions for Feeding Formula.
(1) Formula at room temperature is usually well tolerated by the infant.
(2) Feeding should take place in a comfortable setting and in an unhurried manner.
(3) The newborn should be held in an elevated position (see figure 9-2). Bottles should not be propped because of the danger of the choking and aspiration.
(4) An increased amount of air may be sucked in if the infant is fed when lying flat.
(5) The bottle should be tilted to keep the nipple filled with milk/formula at all times.
(6) When the infant is held close during feedings, he gets more enjoyment from the security of being held by the parent or other person.
(7) Air bubbles can be seen going up into the bottle during feeding. This indicates that the baby is getting the formula.
(8) The infant must take at least one ounce every four hours.
e. Advantages of Formula Feeding.
(1) The mother can be sure the baby is getting enough milk for nutrition.
(2) There is an opportunity for other members of the family to get close to the baby. This allows the mother to give more of her time to her other children, to herself, or to her husband.
a. Preparation of the Nipples. Preparation of the nipples should begin during pregnancy.
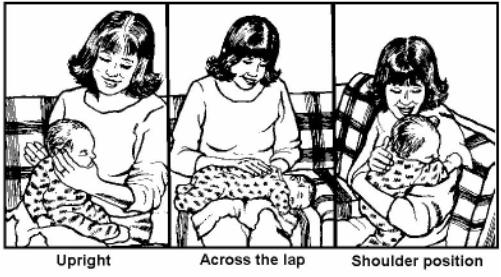
(1) Roll nipples. The mother should roll her nipples with her thumb and forefinger two to three times each day (see figure 9-3).
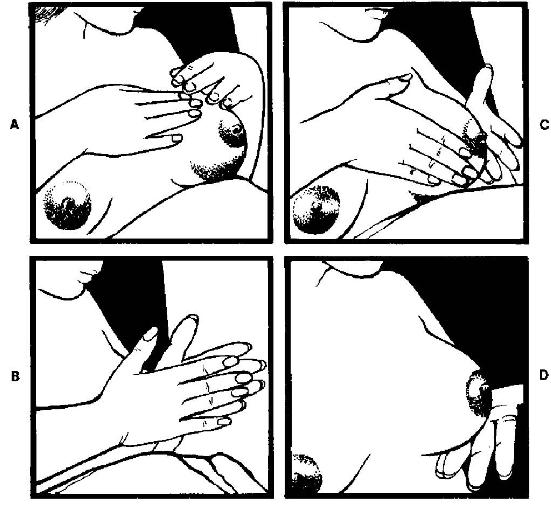
Figure 9-4. Massaging the breasts.
(2) Massage breast (see figure 9-4).
(a) Place hand over the other above the breast.
(b) Gently, but firmly, exert pressure evenly with the thumbs across the top and fingers underneath the breast.
(c) Come together with the heel of the hand on each side and release at the areola, being careful not to touch the areola and nipple.
(d) Gently lift the breast from beneath and drop lightly.
NOTE: The above procedure should be repeated 4 to 5 times with each breast.
(3) Roughen nipples with a towel.
|
b. Initiation of Breast-feeding.
(1) Initial feeding is usually with one ounce of sterile water to determine if the newborn can swallow. The mother should begin feeding with five minutes of actual sucking time on each breast and increase feeding time after the baby has fed three consecutive times without difficulty. Each feeding should be initiated by alternating the breasts. The baby may receive glucose water after feeding until the milk comes in the breast.
(2) The advantages of breast-feeding are as follows:
(a) Colostrum contains less fat and sugar and more protein and salts than breast milk. It also contains large amounts of antibodies and vitamins and acts as a laxative to help expel meconium.
NOTE: Colostrum is the thin yellowish fluid secreted for the first several days after birth. Colostrum comes before the milk in the mother's breast.
(b) Protein is more digestible than cow's milk.
(c) The fat that is present is rich in essential fatty acids needed for brain growth.
(d) Colostrum contains lactose, which favors the development of bacteria in the intestines that serves as a protective function during infancy.
(e) The calcium-to-phosphorous ratio is ideal for the absorption of calcium needed for bone growth.
(f) It appears less likely to produce an obese child, promotes better tooth and jaw alignment, and protects against allergy development during infancy.
(g) Breast-feeding is convenient and eliminates formula preparation.
(h) Breast-feeding is economical.
c. Contraindications.
(1) Nipple or breast lesions may appear (depending on the type).
(2) If the mother becomes pregnant, the milk will usually start to dry up.
(3) Maternal illness.
(4) Need of mother to return to work (although excellent battery operated breast pumps are now available and very inexpensive).
(5) Inability of the mother to psychologically adjust.
(6) A woman with cardiac or established renal disease may be discouraged from nursing.
(7) Infections.
d. Common Breast-Feeding Problems.
(1) Delayed milk production (see figure 9-5). This is usually the earliest of breast-feeding problems. It occurs if the baby is not breast-fed within a short time after birth or not fed frequently enough.
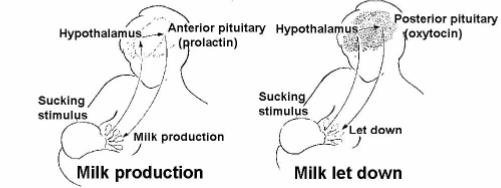
Figure 9-5. Maternal breast-feeding reflexes.
(2) Sore breasts.
(a) The mother should let the baby breast-feed initially for ten to thirty minutes every two to three hours and gradually increase the amount of time. If her breasts are not empty after feeding, have the mother to express the milk into a bottle and refrigerate for later feedings.
(b) Improper position may cause soreness. Advise the mother that the infant should have a portion of the areola, in addition to the nipple in his mouth (see figure 9-6). Just chewing or sucking on the nipple may cause breast soreness.
(3) Engorgement. This normally occurs on or about the third postpartum day. It results from an increase of milk into the milk ducts combined with increased blood and lymph supply to the breast. The breast becomes hard and painful. It is usually more common in the first-time breast-feeding mother. Engorgement can be prevented by:
(a) Manual expression of milk (figure 9-7) if the breasts are full but the infant is not ready to nurse, or if the infant can't get hold of the nipple because the skin is too tight.
(b) Wearing a supportive bra.
(c) Frequent nursing, if not too painful.
(d) Warm compresses applied to the sore breasts.
NOTE: The thumb and forefinger are placed on opposite sides of the breast just behind the areola. The lactiferous sinuses (ampulla A) are compressed, and milk is forced out.
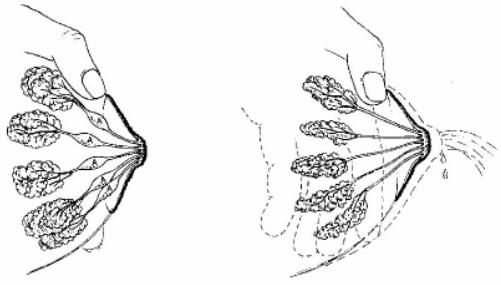
Figure 9-7. Manual expression of milk.
(4) Leaking breasts.
(a) This is a common annoyance. A conditioned response will occur in the mother when she sees or hears a baby that causes the milk to let down.
(b) The mother should fold her arms across her breasts and press them firmly against her chest wall. This will stop the leaking. Advise her to place absorbent pads in her bras.
(5) Maternal anxiety. This will decrease milk production.
(a) An infant reacting to maternal anxiety will usually act in one of two ways.
1 He will suck, stop, cry, suck, stop, cry, and then may regurgitate.
2 He will suck, stop, cry, refuse to nurse, and continue to cry.
(b) Teach the mother relaxation techniques. Tell her to feed her baby in a quiet area.
(6) Sore, cracked, or fissured nipples.
(a) Causes.
1 Infant not having the nipple and areola properly in the mouth.
2 "Friction" of the baby's gums on the nipple.
3 Infant being allowed to suck on an empty breast.
4 Washing the nipples with soap, which is drying.
5 Failure to break suction before removing the infant from the breast.
(b) Nursing interventions. Teach the mother proper nursing techniques and proper breast care.
(7) Breast infection.
(a) Most often caused by the causative organism, Staphylococcus areus.
(b) Entry is gained through a cracked or fissured nipple.
(c) The infection is usually interstitial and not intraductal, so the infection will not harm the baby.
(d) Nursing interventions. Instruct the mother on proper breast care. If breast soreness is present, have the mother to express milk into a bottle to feed to her baby.
a. Methods used to bubble the baby are baby placed on shoulders, baby held upright leaning slightly forward, and baby held across the lap (see figure 9-9). Rub or gently pat his back until air is expelled.
b. When no belch follows feeding, position the baby on his right side or abdomen.
NOTE: Hiccupping is common.
c. The baby should be bubbled frequently.
(1) Bottle-feeding-every 1/2 ounce initially.
(2) Breast-feeding-between each breast.
d. Always be sure to support the head.
9-7. EVALUATING NUTRITIONAL STATUS
a. Observe.
(1) Behavior (crying, content, short sleeper).
(2) Measure either fluid intake from bottle fed newborn or number of minutes at each breast.
(3) Watch for signs of dehydration.
(4) Daily weights (evaluate increases and decreases).
(5) Elimination pattern.
(a) Dark, concentrated urine means too little fluid intake.
(b) Hard stools mean too little fluid intake.
(c) Frequency of stools or urine.
(6) Low-grade temperatures and/or increasing, weak pulses.
b. Determine impact of your observations over a 24-hour period rather than at each feeding.
a. All babies lose weight directly after birth, which should cause no concern unless the weight loss approaches 10 percent of the birth weight.
b. Within a week a newborn should regain his birth weight.
c. A gain of about an ounce a day is average.
d. At the end of 5 months, most babies have doubled their birth weight.
9-9. FIRST ORAL FEEDING AND RECORDING PROCEDURES BY THE NURSE
a. Review the mother's health record to verify the order.
b. Wash your hands.
c. Assemble the necessary equipment (sterile water in bottle, nipple and cap combination, tissue or cloth, and gown (if necessary)).
d. Wash your hands.
e. Put on clean gown (if not already in scrubs).
f. Approach and identify the newborn.
g. Invert the bottle and shake some water on your wrist.
(1) Test the patency of the nipple hole.
(2) Ensure that the water drips freely, but not in a stream. If the hole is too large, the newborn may aspirate water. If the hole is too small, the newborn may tire before the end of feeding.
h. Sit comfortable and cradle the newborn in a semi-reclining position in one arm. The infant's head and back are easily supported. Air is allowed to rise to the top of the infant's stomach where it is more easily expelled.
i. Place the nipple in the newborn's mouth. Do not insert if far enough to stimulate a gag reflex. The newborn should begin to suck. If he doesn't, stroke him under the chin or on the side of his cheek, or touch his lips with the nipple to stimulate a sucking reflex.
j. Tilt the bottle upward as the newborn feeds. Keep the nipple filled with water. This prevents him from swallowing air. Watch for a steady stream of bubbles in the bottle. This indicates proper venting and flow of water.
k. Reinsert the nipple if the newborn pushes the nipple out with his tongue. This is a normal reflex. It does not necessarily mean that he is finished eating.
l. Burp (bubble) the newborn after each 1/2 ounces of water. Some air will be swallowed by the newborn even when fed correctly. Positions to bubble the newborn are:
(1) Hold the newborn upright in a slightly forward position. Use one hand to support his head and cheek. Rub or gently pat his back until air is expelled.
(2) Hold the newborn upright over your shoulder or place him face down across your lap. A change in position helps bring up the bubble. Rub or gently pat his back until air is expelled.
m. Place the newborn on his stomach or right side. This prevents aspiration if he regurgitates.
n. Discard any remaining formula and properly dispose of all equipment.
o. Record the procedures and significant nursing observations in the patient's health record. Give the same report to the Charge Nurse. This will include:
(1) Time of feeding.
(2) Amount taken.
(3) How well the newborn fed.
(4) Did neonate appear satisfied.
(5) Occurrence of any regurgitation or vomiting.
9-10. FORMULA PREPARATION INSTRUCTIONS TO THE MOTHER
Reinforce instruction to the mother about formula preparation.
|
a. Identify the mother requiring reinforcement of teaching.
b. Review the mother's records to identify information previously given.
(1) Facts about formula preparation and storage.
(2) Facts about feeding equipment.
c. Formula preparation and storage.
(1) Commercially prepared formulas should be stored in cool places until opened. Once opened, the formula should be refrigerated at temperature and times suggested by the manufacturer.
(a) Once formula (or powder) has been constituted with water, follow the manufacturer's suggestions for length of time constituted formula is good.
(b) Once the newborn starts to feed, constituted formula should be used within 30 minutes. If not discarded, formula serves as an excellent medium for bacterial growth.
(2) Formulas prepared in the home should be stored in the refrigerator after the initial cool-down period following sterilization.
(a) Bottles of formula that have been sterilized are considered "good" until opened.
(b) Once opened, these bottles should be used within 30 minutes time frame. The unused portion should be discarded and not saved for the next feeding.
(3) Ready-to-feed formulas should be stored in a cool place. Once opened, these feedings should be used within 30 minutes and not saved for subsequent feedings.
(4) Dilution of formulas is of extreme importance. Improper dilution may cause problems such as diarrhea (if too concentrated) and weight loss (if too dilute).
d. Feeding equipment.
(1) Bottles.
(a) May be sterilized at home.
(b) May be cleansed by meticulous washing with warm, sudsy water and rinsing in hot water, and then air-dried.
(c) Plastic bottle inserts may be used but should be discarded after each use. The folds of plastic around the junction of the bottle's neck and the nipple provide a good source of growth medium.
(d) Ready-to-feed bottles pre-filled with formula may be purchased but are quite expensive.
(2) Nipples may be meticulously cleansed at home or may be purchased as a nipple-cap combination.
e. Clarify the mother's understanding of initial instructions.
(1) Provide information to correct any misunderstanding.
(2) Refer any questions you cannot answer to the Charge Nurse.
f. Provide additional instruction, as necessary, to the mother.
g. Determine the mother's understanding by questioning key points.
h. Report and record the mother's instruction appropriately.
Continue with Exercises
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved