|
Lesson 4: Vital Signs
Being human, we are homeothermic; we are warm-blooded and maintain body temperature independently of our environment. Our body generates heat as it burns food. It loses heat through the lungs (breathing), through the skin (sweating), and in body discharges (urine, feces, vomitus, or blood). Body temperature is defined as the measure of the heat inside the body: the balance between heat produced and heat lost.
a. Heat is produced through the metabolism of food (chemically). Food is used as energy by muscles and glands to generate most of the heat in the body. Heat is also gained (physically) from the environment.
b. During exercise, the muscles become active and the person feels warm. Increasing muscular tone (shivering or gooseflesh) produces heat. The process of digestion also increases body temperature.
c. When a person becomes angry or excited, the adrenal glands become very active and the body warms as a result of the action of certain body chemicals such as epinephrine.
d. Cold, shock, and certain drugs, which depress the nervous system, decreases heat production.
e. The hypothalamus is the body's thermostat. It is located in the central nervous system at the base of the brain. This heat-regulating center in the brain senses any changes in the temperature of blood it receives and makes the appropriate adjustments.
f. Heat loss occurs through the following:
(1) Conduction--direct physical contact with an object.
(2) Convection--when body heat warms surrounding air which rises and is replaced by cooler air.
(3) Radiation--body heat warms surrounding objects without physical contact.
(4) Evaporation--perspiration that is removed from the body surface by change from a liquid to a vapor.
Table 4-1. Average, normal temperatures for well adults.
|
A thermometer is placed in the patient's mouth to obtain an oral temperature, in the anal canal to obtain a rectal temperature, and in an axilla (armpit) to obtain an axillary temperature. Table 4-1 shows the average normal temperature for well adults at these various body sites.
a. Temperature is measured on the Fahrenheit (F) or the Celsius (C) scale. The average, normal, oral temperature for an adult is 98.6 degrees Fahrenheit or 37.0 degrees Celsius (old term: centigrade).
b. You can convert Fahrenheit to Celsius or vice versa. To convert Fahrenheit to Celsius, subtract 32 and multiply by 5/9. To convert Celsius to Fahrenheit, multiply by 9/5 and add 32. See Table 4-2 for a conversion chart.
c. Body temperature may wary by 0.5ºF either way and still be within normal limits.
4-7. FACTORS WHICH INFLUENCE NORMAL BODY TEMPERATURE
a. Individual metabolism differs. An increase in the emotional state of the patient may increase the temperature.
b. Body temperature is usually lowest in the morning and highest in the late afternoon or evening.
c. Normal temperature for infants and children is usually higher than the normal adult temperature. At birth, heat-regulating mechanisms are not fully developed, so a marked fluctuation in body temperature may occur during the infant's first year of life.
d. In some women, ovulation may be signaled by a slight drop in body temperature 12 to 24 hours before a postovulation rise in temperature of about 0.4ºF to 0.8ºF.
4-8. TERMINOLOGY RELATED TO BODY TEMPERATURE
Body temperature rises when heat production increases or when heat loss decreases; both may be going on at the same time.
a. Everyone has a temperature; when the temperature is elevated, then pyrexia or a fever is present. A fever is a symptom of some disorder. It often accompanies illness; usually when the body is fighting an infection. An antipyretic is a fever-reducing agent such as aspirin.
b. A temperature significantly below normal is called hypothermia. Such temperatures often precede normal death. Hypothermia may occur as a result of overexposure to winter elements or to cold water. Accidental hypothermia is life threatening and must be treated immediately. Clinical hypothermia is often used to perform surgical procedures because the lowered body temperature slows metabolism and thus decreases the need for oxygen.
c. The patients most at risk of hypothermia are:
(1) Postoperative patients.
(2) Newborn infants exposed to room temperatures before their body temperature has stabilized.
(3) Elderly or debilitated patients.
Regardless of the type of thermometer or measuring probe used, certain rules apply.
a. The bulb or electronic probe is placed so it will be completely surrounded by body tissues.
b. Multi-use thermometers and temperature probes are covered when used. The cover is removed and discarded after the temperature is taken. Prelubricated covers are used for rectal thermometers.
c. The temperature is recorded on the patient's graphic chart to the even two tenths of a degree (unless the electronic thermometer is used). An electronic thermometer is not calibrated with multiple numbers. It displays only the measured temperature. Record the measured temperature.
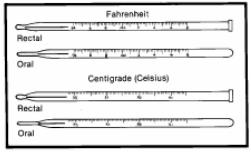
a. Clinical. The clinical thermometer is a glass bulb containing mercury, with a stem in which the mercury can rise. The stem has lines representing the measuring scale. It must read below normal range before the temperature is taken. It should be rinsed in cold water to avoid distribution of the mercury and breakage. If the thermometer is kept in a chemical solution, dry it with a wipe in a twisting motion starting at the bulb. The clinical thermometer may be oral or rectal.
(1) The oral thermometer has a long, slender bulb. It may also be used for axillary measurement.
(2) The rectal thermometer has a blunt, short, fat bulb. It should not be stored with the oral thermometers.
b. Electronic. The electronic thermometer is portable and battery operated. It registers the temperature in 10 seconds or less and displays it digitally. It must be fully charged to give an accurate reading, so be sure the thermometer's base is plugged into an electrical outlet between uses. Separate oral and rectal probes are supplied with each unit.
c. Disposable. The disposable is single-use and has a sensor at the end of the shaft, which measures the temperature.
d. Patch. The thermometer patch is a strip, which contains liquid crystals that change colors as the temperature changes. It is usually placed on the forehead. The scale is adjusted to convert skin-surface temperature to inner-body temperature. The calibration is not as detailed as that of a glass thermometer.
4-11. METHODS OF OBTAINING A TEMPERATURE
|
a. To obtain an oral temperature, place the thermometer in the sublingual pocket and have the patient close his mouth around it. Instruct him not to bite down. Leave the thermometer in place 3 to 4 minutes. If the patient has been eating, drinking, smoking, brushing his teeth, or chewing gum within the past 15 minutes, wait at least 15 minutes to take the temperature.
b. To obtain a rectal temperature, lubricate the bulb and the area up to 1 inch above it. Use a lubricated probe cover with an electronic thermometer. Turn the patient on his side, fold back the bedding and separate the buttocks so that you can easily see the anal opening. Insert the thermometer approximately 1.5 inches into the anus. Hold the thermometer in place for 3 to 4 minutes.
c. To obtain an axillary temperature, place the thermometer in a dry axilla. Keep the arm close to the body to ensure contact with the bulb or probe for 8 to 10 minutes. Axillary is the method of choice for an infant.
d. Precautions.
(1) Oral temperatures are contraindicated for an unconscious patient, for an infant, or when the patient must breathe through the mouth.
(2) The rectal method of obtaining the temperature is contraindicated if the patient has diarrhea, rectal disease, or has recently had rectal surgery.