|
Lesson 1: Preoperative Care of the Surgical Patient
The patient who consents to have surgery, particularly surgery that requires a general anesthetic, renders himself dependent on the knowledge, skill, and integrity of the health care team. In accepting this trust, the health care team members have an obligation to make the patient's welfare their first consideration during the surgical experience. This lesson consists of your duties as a practical nurse to provide preoperative care for the surgical patient.
a. Anesthesia. A partial or complete loss of sensation, with or without loss of consciousness, as a result of a disease, an injury, or administration of a drug.
b. Cyanosis. A Greek word for the slightly bluish-gray or purple discoloration of the skin due to a deficiency of oxygen and an excess of carbon dioxide in the blood. (Oxygen in the blood makes it look red and gives the skin a pink tone.)
c. Narcotics. A group of drugs producing stupor, sleep, or complete unconsciousness; used to allay pain. Narcotics are regulated by federal laws. d. NPO. Nothing by mouth (Latin, nulli per os).
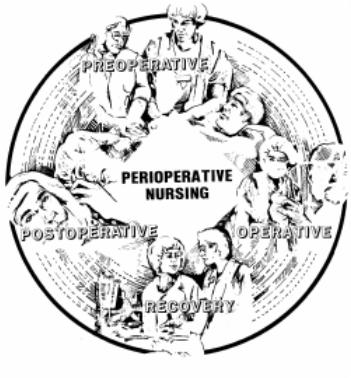
e. Perioperative Period. The period extending from the time of hospitalization for surgery to the time of discharge (see Figure 1-1).
f. Preoperative Phase. That phase of the perioperative period during which the nurse admits the patient to the surgical unit and helps the individual prepare physically and emotionally for the operation. Refer to Figure 1-1.
g. Prosthesis. An artificial organ or part; for example, an artificial limb, eyeglasses, or dentures.
h. Thrombophlebitis. Inflammation of a vein associated with thrombus formation.
i. Thrombus. A blood clot.
|
NOTE: Figure 1-1 shows: A. Teaching the patient and spouse during the preoperative phase B. Nurse handing sponge to surgeon in the operative phase C. Patient being observed and monitored during the recovery phase; and nurse checking patient's bandage during the postoperative phase.
|
1-3. PREOPERATIVE PHASE
Although the physician is responsible for explaining the surgical procedure to the patient, the patient may ask the nurse questions about the surgery. There may be specific learning needs about the surgery that the patient and support persons should know. A nursing care plan and a teaching plan should be carried out. During this phase, emphasis is placed on:
a.
Assessing and correcting physiological and psychological problems that may increase surgical risk.
b.
Giving the patient and significant others complete learning and teaching guidelines regarding the surgery.
c.
Instructing and demonstrating exercises that will benefit the patient postoperatively.
d. Planning for discharge and any projected changes in lifestyle due to the surgery.
Surgery is an important event in any individual's life. It represents a serious decision involving the patient's body and his health. It also produces physical and psychological stress on the body relative to the extent of the surgery and injury to the tissue involved. The patient must understand what is proposed, understand all the risks, and give his consent.
a. Physical Stress. Surgery produces actual physical damage to tissues of the body.
(1) An incision is a cutting of the skin and other tissues. The internal
organs and tissues of the body are handled by the surgeon and assistants. This could lead to bruising of tissues, injury to tissues, or inflammation of tissues that could result in pain after the anesthesia wears off.
(2) Incisions through the skin and mucous membranes penetrate the protective barriers of the internal organs. This puts a patient at risk of microorganisms entering the body and causing infection. Surgery requires strict attention to aseptic technique, use of sterile materials, and thorough disinfecting of the skin around the operative site.
(3) The effects of anesthesia and other medications tend to last well into the postoperative recovery period. These drugs could have a depressant effect on the body; they decrease pain and reduce awareness of one's surroundings. The effect on the body systems is to slow the systems down and make them hypoactive.
b. Psychological Stress. The physical stress of surgery is greatly enhanced by the psychological stress of anxiety and worry, which uses up energy that is needed for healing of tissues in the postoperative period. When surgery is needed, one's deepest and worst fears are often felt. A preoperative patient may experience a number of fears. However, the following fears are common among surgical patients:
(1) Loss of part of the body.
(2) Unconsciousness and the inability to know or control what is happening.
(3) Pain.
(4) Death
(5) Separation from family.
(6) Effects of surgery on home and employment.
(7) Exposure of his body to strangers.
c. Managing Preoperative Fears. Psychological preparation of the patient before surgery can not be overlooked. Along with other members of the health care team, the practical nurse must show warmth, sensitivity, and caring to the patient. Each patient may express his fears in different ways. You may find that a patient may not talk about his fears. He may be quiet and withdrawn, cry, or talk constantly. Some patients may prefer pacing, be extremely cheerful, or, on the other hand, exhibit unusual behavior. You, as a practical nurse, must recognize these fears and deal with them properly. You can help to manage preoperative fears by:
(1) Providing an opportunity for the patient to describe his reactions and feelings in the stressful situation.
(2) Providing or reinforcing patient teaching.
(3) Arranging for a clergy to visit if the patient desires. (Religious faith can be a strong source of strength.)
(4) Being truthful and honest when answering patient questions. If there are questions that you should not or are unable to answer, refer them to the Charge Nurse or physician.
1-5. PREOPERATIVE TEACHING PRINCIPLES
a. The value of preoperative instruction to the patient is very important. Each patient should be taught as an individual, in terms of his anxieties, need, and hope. Patients should be taught postoperative exercises they will be required to do and their role in preventing complications. The postoperative exercises include turning, deep breathing, coughing, and extremity movement.
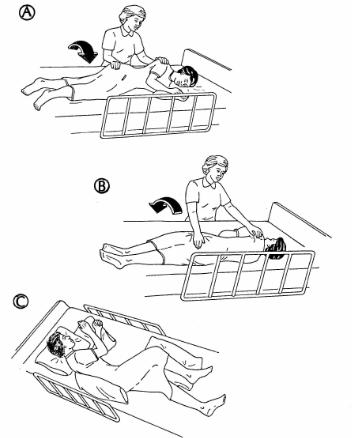
(1) Turning. Turning in bed and early ambulation helps patients maintain blood circulation, stimulate respiratory functions, and decrease the stasis of gas in the intestines and resulting discomfort. Practice before surgery usually makes it easier for the patient to do it postoperatively. In some instances, the patient may need special aids, such as a pillow between the legs, to help maintain body alignment. See Figure 1-2.
|
A. Patient turned away from the nurse with arms and legs crossed. B. Patient turned toward the nurse with arms and legs crossed. C. Patient on side in middle of bed with a pillow in front of the bottom leg with the top leg on the pillow in flexed position, a pillow against the back, a small pillow supports the arm and hand, pillow under head and shoulder.
|
|
|
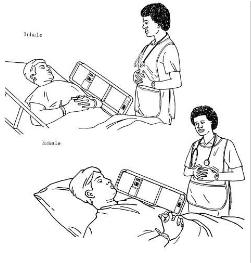
2) Deep breathing. Deep breathing helps prevent postoperative pneumonia and atelectasis (incomplete expansion of the lung or a portion of the lung). In deep breathing, the patient should inhale and exhale as much air as possible. You are to explain the procedure and its purpose to the patient. Instruct the patient to:
a) Inhale slowly through the nose, distending the abdomen and exhaling slowly through pursed lips (see Figure 1-3).
(b) Deep breathe as often as possible, preferably 5 to 10 times every hour during the postoperative, immobilized period.
(3) Coughing. Coughing is done to mobilize and expel respiratory
system secretions which, because of the effects of anesthesia, tend to pool in the lungs and may cause pneumonia. The patient should be in a sitting or lying position. Instruct the patient to:
(a) Lean forward slightly while sitting in bed.
(b) Take a deep breath.
(c) Inhale fully with the mouth slightly open.
(d) Let out three to four sharp "hacks."
(e) With mouth open, take in a deep breath and give one or two strong coughs.
(f) Repeat steps (a) through (e) ten times, as tolerated.
NOTE: The above steps should be repeated every two hours during the postoperative phase or as prescribed.
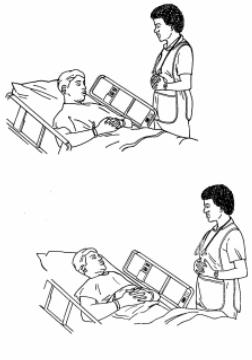
(g) The patient may lace his fingers and hold them tightly across the incision before coughing. This is used as a splint to minimize pressure and helps to control pain when the patient is coughing. A small pillow or folded towel may be used in place of laced fingers. See Figure 1-4. NOTE: Encourage the patient to perform deep breathing exercises before coughing. This stimulates cough reflex.
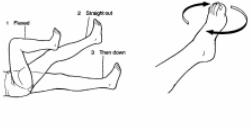
(4) Extremity exercises. These exercises help to prevent circulatory problems, such as thrombophlebitis, by facilitating venous return to the heart. It also decreases postoperative "gas pains." See Figure 1-5 for legs and feet exercises. The patient should:
(a) Flex and extend each joint, particularity the hip, knee, and ankle joints, keeping the lower back flat as the leg is lowered and straightened.
(b) Move each foot in a circular motion.
b. Time of Instruction. The best time to teach patients is relatively close to the time of surgery, which is usually the afternoon or evening before the surgery.
(1) If instruction is given several days in advance, the patient may forget.
(2) If instruction is given just before surgery, the patient may be too apprehensive to listen or too heavily sedated to comprehend.
(3) If the patient is undergoing minor surgery (one-day or same-day surgery), the patient may receive preoperative instructions several hours before surgery.
1-6. NURSING IMPLICATIONS FOR PREPARING A PATIENT FOR SURGERY
a. Patient's Chart. The preoperative patient's chart must be complete before the patient leaves the nursing unit. It will contain all the information that may be needed by the physicians and nurses in the operating room or later in the recovery room. The chart should be prepared by using DD Form 1924, Surgical Checklist (see Figure 1-6). DD Form 1924 is attached to the front of the patient's chart for easy access by all involved hospital staff. It contains the following information:
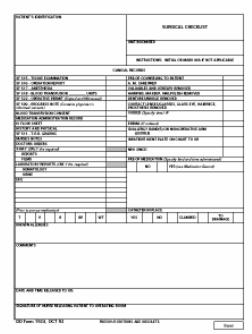
Figure 1-6. DD Form, 1924, Surgical Check List.
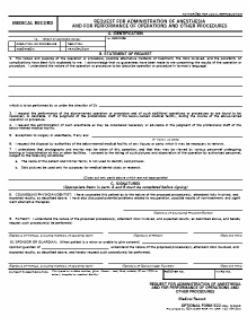
Figure 1-7. SF 522, Request for Administration of Anesthesia and for Performance of Operations and Other Procedures.
(1) Patient's identification.
(2) Checklist for pertinent health records.
(3) Block for recording the most current set of vital signs taken prior to preoperative medications. (4)
Block to indicate allergies. (5)
Block to document all preoperative nursing measures. (6)
Block to document comments. Any special comment that indicates something very special about this particular patient will go in this block (hard of hearing, removal of a prosthesis, etc.).
(7) Block for signature of release when all actions are completed. b.
Procedures Used to Prepare the Patient's Chart. You will use
DD Form 1924, Surgical Checklist, as a checklist to assemble the patient's chart and to document compliance as each step is completed.
(1)
DD Form 1924. Enter the patient's identifying information in the patient's identification block. This information may be entered by using the addressograph plate or by hand. If you enter the information by hand, enter the patient's ward, room, and bed in the appropriate block.
(2)
Patient's chart. Ensure that all required forms are included, complete as necessary, and in order dictated by local policy. Document compliance or insert form(s) as necessary. (a)
Place your initials in the box to indicate that the form is in the chart and completed. (b)
If forms are missing or incomplete, notify the Charge Nurse or physician as indicated.
(c) Required forms are:
(1) SF 515, Tissue Examination -- 2 copies.
(2) SF 516, Operation Report -- 3 copies.
(3) SF 517, Anesthesia -- 2 copies.
(4) SF 518, Blood or Blood Component Transfusion -- 3 copies.
(5) SF 522, Request for Administration of Anesthesia and for Performance of Operations and Other Procedures (see Figure 1-7.) This is the legal document that satisfies the requirement of informed consent.
(a) It must be signed by the physician and anesthesiologist to indicate that all risks of surgery and anesthesia have been fully explained to the patient.
(b) The preoperative patient must sign the form in the presence of a witness to consent for a surgical procedure.
(c) The witness must NOT be anyone on the surgical team.
(d) The date and time that the patient signed must be
written on the form. (f) Legal consents must be signed PRIOR to the preoperative administration of narcotics or any type of mind altering medication, or the form is not legally binding. (6) History and Physical,
SF 511 (T.P.R. Graphic),
SF 510 (Nursing Notes), and
Doctor's Orders. Check the patient's health record for inclusion of these forms and document compliance.
(e) Minors (patients under legal age) cannot sign for
themselves; it must be signed by a parent or legal guardian. NOTE: Legal age is established on a state-by-state basis.
(a) Each form will be checked for date, signature, and accurate transcription.
(b) Stamp and insert new forms for use during surgical experience, if needed,
(3) Acquire required x-ray reports and films as necessary, insert reports into patient's chart, and document compliance.
(a) Ensure x-rays have been taken.
(b) Check for x-ray results in health records.
(c) If the results are not on the record, call x-ray for results and write report in comments section. Make an attempt to locate written x-ray report and films.
(d) Notify the Charge Nurse or physician immediately of previously unreported abnormal x-ray findings.
(4) Acquire laboratory reports as required, insert reports into the patient's chart, and document compliance.
(a) Ensure ordered lab work has been done.
(b) Check for laboratory results on health records.
(c) If the laboratory results are not in the record, call the laboratory for results and write the report in the "comments" block. Make an attempt to locate written lab reports to place in the patient's chart.
(d) If laboratory reports indicate abnormal values which may not have been known by the physician and which could could influence surgery, notify the Charge Nurse or physician immediately.
(5) Acquire EKG report as required, insert the report into the patient's chart, and document compliance.
(a) Ensure EKG was completed for all patients over 40 years of age and others as ordered.
(b) Check with appropriate department (Internal Medicine or Cardiology) for EKG readings if not in record.
(c) If the results are not on the health record, call the department for the report and place the information in the "comments" block. Make an attempt to locate the written report to place in the health record.
(d) Notify the Charge Nurse or physician immediately of previously unreported abnormal EKG results.
c. Final Preparation of the Preoperative Patient. Document compliance on DD Form 1924 and on SF 510, Nursing Notes.
(1) Preoperative care. Implement doctor's orders for preoperative care.
(a) Administer an enema the night before surgery, if ordered. An enema is used to cleanse the colon of fecal material, thus reducing the possibility of wound contamination during surgery.
(b) Ensure that the operative site skin prep is done. An operating room technician or other designated person will clean and shave the area surrounding the side of the planned incision(s).
1 The skin prep is done to make the skin as free of microorganisms as possible, thus decreasing the possibility of microorganisms entering the wound from the skin surface during surgery.
2 A wide area of skin around the site of the incision is shaved and cleansed to further reduce the possibility of infection.
(2) Personal hygiene. Assist the patient with personal hygiene and related care.
(a) Bathe or shower. This is done to remove excess body dirt and
oils. It gives the patient a sense of relaxation. Depending upon the extent of surgery, it may be several days before a patient may take a "real bath."
(b) Shampoo hair. This is also done for the same reasons as in the previous paragraph.
(c) Remove nail polish and make-up. During surgery, numerous areas must be observed carefully for evidence of cyanosis to include the face, lips, and nail beds. Make-up and nail polish hide true coloration.
(3) Mouth care. All preoperative patients should have thorough mouth care before surgery. A clean mouth makes the patient more comfortable and prevents accidental aspiration of food particles. Chewing gum must be removed before the patient goes to the operating room.
(4) Attire. Give the patient a clean hospital gown. The wearing of his own gown or pajamas to surgery is not permitted because of potential loss or damage.
(5) Prostheses. Ask the patient to remove his dentures, contact lenses, and artificial limbs. Be sure to place all items in a container labeled with the patient's name and room number. Take extra care not to break or loose patient's prostheses. If possible, send the prostheses home with a relative.
(6) Jewelry. Jewelry should be removed for safekeeping. Do NOT store in bedside stand -- give the jewelry to a relative. The patient may wear a wedding band to surgery secured with tape or gauze wrapping. Do not secure it so tightly as to impair circulation.
(7) Food and fluids. Follow the doctor's orders for type of diet preoperatively. Usually, the patient will be NPO from midnight on. Remove the patient's water pitcher. Place an NPO sign outside patient's room (see Figure 1-8). Mark the diet roster.
(8) Offer emotional support. Answer questions concerning surgery. Provide explanation of each preoperative nursing measure. Ask the patient about spiritual needs. Provide family members with information concerning their role the morning of surgery, waiting room location, postoperative visit by surgeon, rational for stay in recovery room, and presence of any special tubes or machines attached to their loved one.
(9) Sedative. Administer the patient a sedative for a good night's sleep, if ordered.
d. Communication. Good communication between all members of the health care team will ensure that the patient is well prepared and ready to undergo surgery. All shifts and nursing personnel must be an active participant in the preoperative phase of the surgical patient.
1-7. THE MORNING OF SURGERY
 a.
Awaken the patient early enough so that he may:
a.
Awaken the patient early enough so that he may:
(1) Perform morning care.
(2) Complete last-minute personal measures.
(3) Remove nightclothes.
(4) Visit with family.
b. Take and record vital signs.
c. Recheck accuracy of DD Form 1924.
d. Administer preoperative medication if ordered. This medicine:
(1) Enhances the effectiveness of anesthesia.
(2) Decreases the side effects of nausea/vomiting from anesthesia.
(3) Produces anti-anxiety.
(4) Dries up secretions.
e. Provide for the patient's security by placing side rails in the up position and by placing a call bell within the patient's reach once preoperative medication is given.
f. Assist the operating room technician to position the patient on the OR litter and make the patient comfortable.
g. "Sign out" the patient on SF 510, Nursing Notes, to include:
(1) Date.
(2) Time.
(3) Event.
(4) Status of patient.
h. "Sign off" in the appropriate block on DD Form 1924, Surgical Checklist.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved