Hypertensive Issues
During Pregnancy
Elevated blood pressure during pregnancy is a significant problem affecting many
pregnancies. In some cases, the hypertension is pre-existing, while in others,
it develops over the course of pregnancy. Occasionally, it does both.
Normal Blood Pressure
Changes During Pregnancy
During the middle trimester, blood pressure (both systolic and diastolic)
normally drop below early pregnancy and prepregnancy levels. Not uncommonly,
there is a widening of the pulse pressure (difference between systolic and
diastolic levels). These changes are associated with the significant reduction
in peripheral vascular resistence and some degree of AV shunting within the
uterus and intervillous space. The decreased peripheral resistance is
compensated by the relative tachycardia so often found among pregnant women.
In the third trimester, blood pressure usually rises to approximately
pre-pregnancy levels. Elevations significantly higher than that are considered
abnormal.
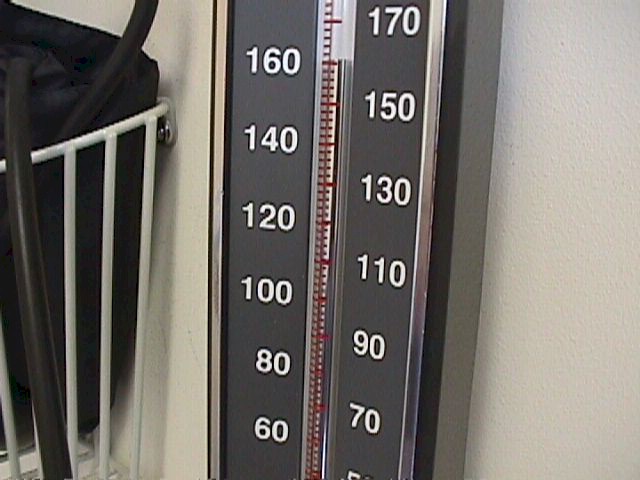
Hypertension
The definition of hypertension varies, but one common definition is the
sustained elevation of BP above 140/90. Most obstetricians believe that if either the systolic or the diastolic pressure is elevated on a sustained
basis, that hypertension exists. A few require that both be elevated. As
a practical matter, in most cases of hypertension, both are elevated.
The diastolic pressure elevation is probably the more important of the two
and mean arterial pressure (MAP) during the second or third trimester are used
by some to assess risk. Conceptually, the MAP is one-third the distance from the
diastolic pressure to the systolic pressure. This can be expressed
mathematically as:
MAP = ((2 x diastolic) + (systolic))/3
During the second trimester, if the average of all MAPs ≥ 90, there is a significant increased risk
for perinatal mortality, morbidity and impaired fetal growth dynamics.
During the 3rd trimester, MAP ≥ 105 indicates
and increased risk
Women with pre-existing hypertension face increased risks during pregnancy
for diminished uterine blood flow, pre-eclampsia, and if uncontrolled, maternal
stroke. For these reasons, it is important that those with pre-existing
hypertension be appropriately treated and followed during pregnancy.

Pitting Edema |
Toxemia of
Pregnancy
Toxemia of pregnancy is a clinical syndrome characterized
by elevated blood pressure, protein in the urine, fluid retention and increased reflexes.
It occurs only during pregnancy and resolves completely after pregnancy. It is seen most
often as women approach full term, but it can occur as early as the 22nd week of
pregnancy. It's cause is unknown, but it occurs more often in:
-
Women carrying their first child
-
Multiple pregnancies
-
Pregnancies with excessive amniotic fluid (polyhydramnios)
-
Younger (<17) and older (>35) women
Ordinarily, blood pressure decreases during the middle
trimester, compared to pre-pregnancy levels. After the middle trimester, blood pressure
tends to rise back to the pre-pregnancy levels. Sometimes, blood pressure becomes
elevated.
Sustained blood pressures exceeding 140/90 are considered
abnormal and may indicate the presence of toxemia of pregnancy. For women with
pre-existing hypertension, a sustained worsening of their hypertension over pre-pregnancy
levels by 30 systolic and 15 diastolic is often used to indicate the possible presence of
super-imposed toxemia.
Diagnosis
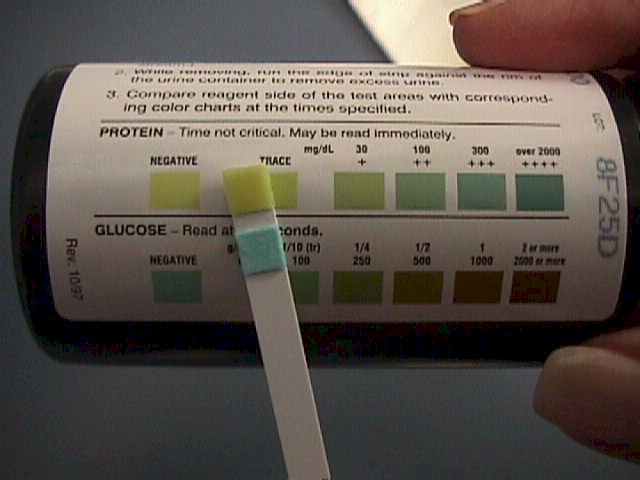
The presence of hypertension and proteinuria are essential
to the diagnosis of toxemia of pregnancy.
Pregnant women can normally lose up to 200 mg of protein
in the urine in 24 hours. If protein loss exceeds 300 mg in 24 hours, this is considered
proteinuria. Urine dipstick analysis for protein measures only a single point in time and
does not necessarily reflect protein loss over 24 hours. Nonetheless, assuming average urine production of about a liter a day, and consistent loss throughout the
24 hour period*:
Category |
Negative |
Trace |
1+ |
2+ |
3+ |
4+ |
Dipstick Results |
<15 mg/dL |
15-29 mg/dL |
30 mg/dL |
100 mg/dl |
300 mg/dl |
>2000 mg/dL |
Equivalent
24-hour Results* |
<150 mg |
150-299 mg |
300-999 mg |
1000-2999 mg |
3-20 g |
>20 g |
Some but not all women with toxemia demonstrate fluid
retention (as evidenced by edema or sudden weight gain exceeding 2 pounds per week). Some
but not all women with toxemia will demonstrate increased reflexes (clonus).
Most women toxemia of pregnancy have no
symptoms. Among the few with symptoms are such findings as:
-
Headache, usually frontal but sometimes
occipital, analgesic-resistent.
-
Visual disturbances, including blurring
and scotomata
-
Aching pain in the right upper
quadrant, caused by stretching of the liver capsule.
Cause(s) of Toxemia of Pregnancy
The cause or causes are not known. Some common associations are first
pregnancies, pre-existing hypertension, hydatidiform mole, and those conditions
which lead to overdistension of the uterus, such as polyhydramnios and multiple
gestation.
Physiologically, women with
this condition demonstrate peripheral vascular spasm, leading to injury of the
capillary walls and leakage of intravascular fluids into the extracellular
spaces. Due to the modestly impaired kidney function that accompanies this
condition, serum creatinine levels are usually modestly increased (>1.0 mg%).
Hemoconcentration results in a modest increase in hemoglobin and hematocrit.
Both contribute to an elevation of BUN, usually >12 mg%. Uric acid is typically
>5.5 mg% due to increased production in association with peripheral vascular
sluggishness.
Consequences
Toxemia of pregnancy, including pre-eclampsia, eclampsia and the HEELP syndrome,
are very dangerous, with potentially serious consequences for both the mother
and fetus. Among these are:
-
Preterm delivery
-
Placental abruption
-
Precipitous delivery
-
Maternal convulsions
-
Decreased uteroplacental perfusion
-
Fetal growth restriction
-
Increased perinatal mortality
-
Maternal renal failure
-
Maternal disseminated intravascular
coagulation (DIC) and hemorrhage
-
Liver failure
-
Pulmonary edema
-
Maternal stroke
Fortunately, most cases of toxemia of pregnancy
are mild, and most of the more severe forms are successfully treated (delivered)
before the serious consequences can unfold. In some severe cases, even early
diagnosis and treatment will prove unsuccessful in avoiding the more serious
consequences.
Pre-eclampsia
Toxemia of pregnancy is subdivided into two categories: pre-eclampsia and eclampsia.
The difference is the presence of seizures in women with eclampsia.
The clinical course of pre-eclampsia is variable. Some women demonstrate a mild, stable
course of the disease, with modest elevations of blood pressure and no other symptoms
(mild pre-eclampsia). Others display a more aggressive disease, with deterioration of both
maternal and fetal condition (severe pre-eclampsia). Some of the points of differentiation
are listed here. Notice that there is no "moderate" pre-eclampsia, only mild and
severe.
Problem |
Mild Pre-Eclampsia |
Severe Pre-Eclampsia |
Blood Pressure |
>140/90 |
>160/110 |
Proteinuria |
1+ (300 mg/24 hours) |
2+ (1000 mg/24 hours) |
Edema |
+/- |
+/- |
Increased reflexes |
+/- |
+ |
Upper abdominal pain |
- |
+ |
Headache |
- |
+ |
Visual Disturbance |
- |
+ |
Decreased Urine Output |
- |
+ |
Elevation of Liver Enzymes |
- |
+ |
Decreased Platelets |
- |
+ |
Increased Bilirubin |
- |
+ |
Elevated Creatinine |
- |
+ |
The definitive treatment of pre-eclampsia is delivery. The urgency of delivery depends
on the gestational age and the severity of the disease.
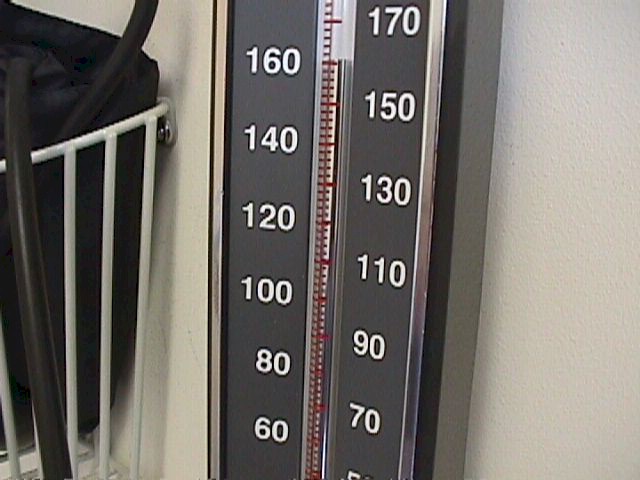
Severe pre-eclampsia is associated with blood
pressures in excess of 160/110 |
Severe pre-eclampsia usually
requires urgent delivery (within hours) more or less regardless of gestational age. In
this situation, the risk of serious complications (placental abruption, growth
restriction, liver failure, renal failure, hemorrhage, coagulopathy, seizures, death) will
generally take precedence over the fetal benefit of prolonging the pregnancy. Induction of
labor is preferred, unless the maternal condition is so tenuous and the cervix so
unfavorable that cesarean section is warranted.
In milder cases, particularly if remote from term or with an unfavorable cervix,
treatment may range from hospitalization with close observation to initial stabilization
followed by induction of labor following preparation of the cervix over the course of
several days. In the most mild, selected cases, outpatient management might be considered
with careful monitoring of maternal and fetal condition.
Traditionally, magnesium sulfate(MgSO4) has been used to treat pre-eclampsia. Magnesium
sulfate, in high enough doses, is a reasonably effective anti-convulsant, mild
anti-hypertensive and mild diuretic. While other agents may be more potent in each of
these individual areas, none combines all three of these features into a single drug. The
world's experience with magnesium
sulfate to treat pre-eclampsia is extensive and these
unique features provide considerable reassurance in employing it in these clinical
settings. Magnesium
sulfate is given IM, IV or both. All are effective reasonably
effective in preventing seizures. Because the risk of eclampsia continues after delivery, MgSO4 is frequently continued for 24 to 48 hours after delivery.
-
Magnesium
sulfate 10 gm in a 50% solution, one-half (5 gm) IM, injected deeply into each
upper outer buttock quadrant. Every 4 hours thereafter, Magnesium
sulfate 5 gm IM is
injected into alternating buttocks. Repeat injections are postponed if patellar reflexes
are absent. Because these injections are painful, 1 ml of 2% lidocaine is sometimes added
to the magnesium. This schedule gives therapeutic levels of magnesium (4-7 meq/L)
-
Because IM magnesium sulfate does not initially achieve its therapeutic levels for 30 to
45 minutes, in cases of severe pre-eclampsia, an IV bolus of magnesium sulfate can be
added. 4 gm magnesium sulfate as a 20% solution can be given slowly over at least 5
minutes, followed by the IM injections described above.
-
Magnesium
sulfate 4 gm IV, slowly, over at least 5 minutes, followed by 2 gm IV/hour.
The therapeutic
margin (distance between effective dose and toxicity) is relatively thin with magnesium sulfate, so some precautions need to be taken to prevent overdose. The biggest problem
with MgSO4 is respiratory depression (10 meq/L) and respiratory arrest (>12 meq/L).
Cardiovascular collapse occurs at levels exceeding 25 meq/L. Magnesium levels can be measured
in a hospital setting, but clinical management works about as well and is non-invasive.
The patellar reflexes (knee-jerk) disappear as magnesium levels rise above 10 meq/L. Periodic checking of the patellar reflexes and withholding MgSO4 if
reflexes are absent will usually keep your patient away from respiratory arrest. This is
particularly important if renal function is impaired (as it often is in severe
pre-eclampsia) since magnesium is cleared entirely by the kidneys.
In the case of respiratory arrest or severe
respiratory depression, the effects of MgSO4 can be reversed by the administration of
calcium.
If BP is persistently greater than 160/110,
administer an antihypertensive agent to lower the BP to levels closer to 140/90. One
commonly-used agent for this purpose is:
Eclampsia
Eclampsia means that maternal seizures have occurred in
association with toxemia of pregnancy.
These tonic/clonic episodes last for several minutes and
may result in bite lacerations of the tongue. During the convulsion, maternal respirations
stop and the patient turns blue because of the desaturated hemoglobin in her bloodstream.
As the attack ends, she gradually resumes breathing and her color returns. Typically, she
will remain comatose for varying lengths of time. If convulsions are frequent, she will
remain comatose throughout. If infrequent, she may become arousable between attacks. If
untreated, convulsions may become more frequent, followed by maternal death. In more
favorable circumstances, recovery occurs.
Eclampsia should be aggressively treated with magnesium
sulfate (described above), followed by prompt delivery, often requiring a cesarean
section. If convulsions persist despite MgSO4, consider:
HELLP Syndrome
The HELLP Syndrome is characterized by:
This serious condition is associated with severe
pre-eclampsia and the treatment is similar...delivery with prophylaxis against maternal
seizures.
Unlike pre-eclampsia, patients with HELLP syndrome may
continue to experience clinical problems for days to weeks or even months.
If the HELLP syndrome is mild, it may gradually resolve
spontaneously, but more severe forms often require intensive, prolonged care to achieve a
favorable outcome. |