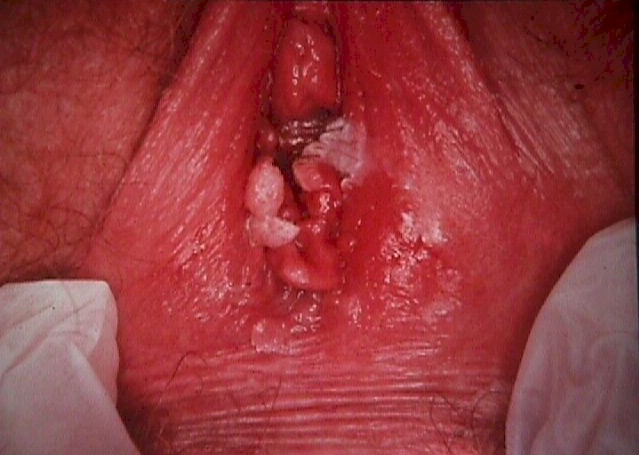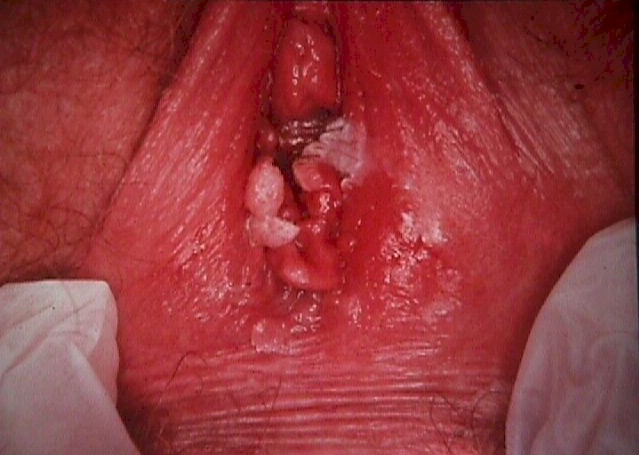
Vulvar Warts (Condyloma accuminata)
|
Human papilloma virus is a common skin virus, responsible for the common
skin wart (usually HPV type 1). HPV Type 1 prefers to grow on cornified,
squamous epithelium, such as the fingers or the feet. HPV Type 1 has no
gynecologic significance.
Other HPV Types do have gynecologic
significance. Some of them are associated with the development of
genital warts. These benign neoplasms are not dangerous but can be
annoying. Venereal warts (condyloma accuminata) can appear on the vulva,
inside the vagina, or on the cervix. They are painless, firm,
cauliflower-like growths. If watched over the course of a year, about
half will disappear spontaneously, while the other half will persist or
grow. A number of treatments are effective in making the warts
disappear, including excisional surgery, cryosurgery, electrocautery,
topical acid (trichloracetic acid or bichloracetic acid), podophyllin or
podophyllin-like applications, or Aldara topical applications. Any of
these will make the warts go away, but the HPV virus will still persist
(dormant) within the skin cells. Under the right set of circumstances
(trauma, immune system distraction, etc.) the HPV can reactivate and new
warts can grow, although usually this doesn't happen. Usually, once
treated, the HPV lies dormant forever. There is no known cure for the
HPV infection.
HPV infections are common, affecting as many as half the
sexually-active adult population. They are transmitted by skin-to-skin
contact from an individual shedding the virus to their sexual partner.
Those with multiple sexual partners are more likely to have been
infected with the HPV virus, as are immunocompromised hosts, and tobacco
smokers. Immunocompromised hosts are particularly vulnerable to the
effects of HPV, often demonstrating severe cases, rather than the
occasional small wart.
More dangerous is the association between HPV and cervical neoplasia.
Studies of cervical cancer cells and high-grade dysplasia cells have
routinely found HPV. That is not to say that everyone who acquires HPV
will develop cervical cancer. Rather, it appears that HPV is
pre-requisite for the development of cervical cancer. Whether it
develops or not hinges on many other factors, including genetic
predisposition, immunologic state, and gynecologic interventions.
One important factor related to the subsequent development of
cervical dysplasia and cervical canceris the particular HPV type that is
present. Some are more dangerous than others.
| Low Risk HPV Types |
High Risk HPV Types |
| 6, 11, 42, 43, 44 |
16, 18, 31, 33, 35,, 39, 45, 51,
52, 56, 58, 59, 68 |
The knowledge of which HPV type is present can be useful in some
situations. For patients with a mildly abnormal Pap smear (ASC) or a
low-grade cervical dysplasia, the absence of any high-risk HPV types can
be moderately reassuring to the patient. A high-risk HPV type could
warrant more aggressive management. However, HPV typing is not 100%
accurate in predicting biologic behaviour. |