|
Fetopelvic Disproportion
Clinical Pelvimetry
· X-ray Pelvimetry
· Estimation of Fetal Weight
· Progress of Labor
Fetopelvic disproportion is any clinically significant mismatch between
the size or shape of the presenting part of the fetus and the size or
shape of the maternal pelvis and soft tissue. A 12-pound fetus trying to
squeeze through a maternal pelvis that is only adequate for a 7-pound
baby would be an example of fetopelvic disproportion.
The problem of
disproportion may be based strictly on size, or may be related to the
way in which the fetus is trying come out. Occiput anterior is the usual
position for a fetus and that position is generally the most favorable
for negotiating the diameters and turns of the birth canal. Should a
fetus attempt to come through the birth canal in the occiput posterior
position, it is more difficult for the fetal head to negotiate the
turns. If the fetus is small enough and the pelvis large enough, it can
still deliver as a posterior. Otherwise, the fetal head will need to be
turned to anterior, or a cesarean section performed.
Some disproportions are relative, while others are absolute. The
relative disproportions may allow for non-operative vaginal delivery, if
labor is allowed to continue long enough and there is sufficient molding
or re-shaping of the fetal head to allow it to squeeze through. In the
case of absolute disproportion, no amount of fetal head re-shaping will
allow for unassisted vaginal delivery, and it may not allow for a
vaginal delivery at all. Even in the case of relative disproportion,
that fact that eventually a fetus might squeeze through doesn't
necessarily mean that continued labor is wise.
Even if highly accurate measurements of the maternal pelvis and fetal
size were possible (and they are not), it would still be difficult to
predict in advance those who will deliver vaginally easily and those who
will not. All measurements are essentially static, and do not take into
account the inherent "stretchiness" of the maternal pelvis or the
compressibility of the fetus. The pelvis is not a single solid bone, but
is comprised of many bones, held together by cartilage and ligaments.
During pregnancy, these soft-tissue attachments become more pliable and
elastic, allowing considerable movement. Similarly, fetal tissues can be
safely compressed, to a certain extent. For these reasons, trying to
predict whether a dynamically-shaped fetus will fit through a
dynamically-shaped pelvis, based only on static measurements, becomes
nearly impossible. Can a basketball fit through a rubber band? Of
course, it depends on how big the basketball is, how big the rubber band
is, how inflated the basketball is, and how stretchy the rubber band is.
Accurately measuring the size of the basketball and the rubber band
won't answer all of those questions.
Clinical Pelvimetry
Methods of performing clinical pelvimetry range from the very simple
to very complex. Simple digital evaluation of the pelvis, allows the
examiner to categorize it as probably adequate for an average sized
baby, borderline, or contracted. Other methods include the following:
-
Measuring the diagonal conjugate. Insert two fingers into the
vagina until they reach the sacral promontory. The distance from the
sacral promontory to the exterior portion of the symphysis is the
diagonal conjugate and should be greater than 11.5 cm.
-
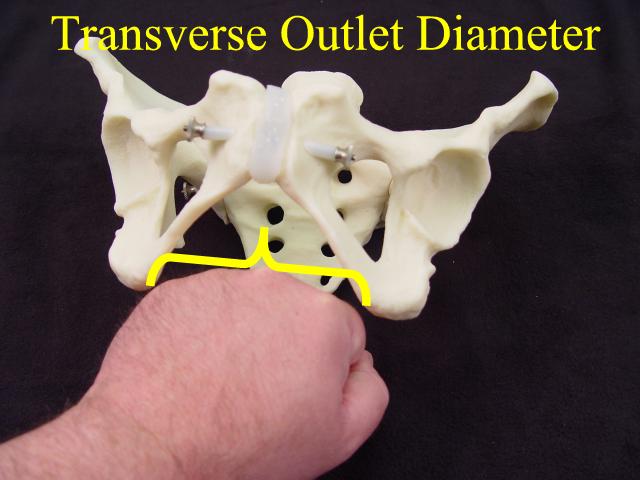
Measure the bony outlet by pressing your closed fist against the
perineum. Compare the previously-measured diameter of your fist to the
palpable distance between the ischial tuberosities. Greater than 8 cm
bituberous (or bi-ischial, or transverse outlet) is considered normal.
-
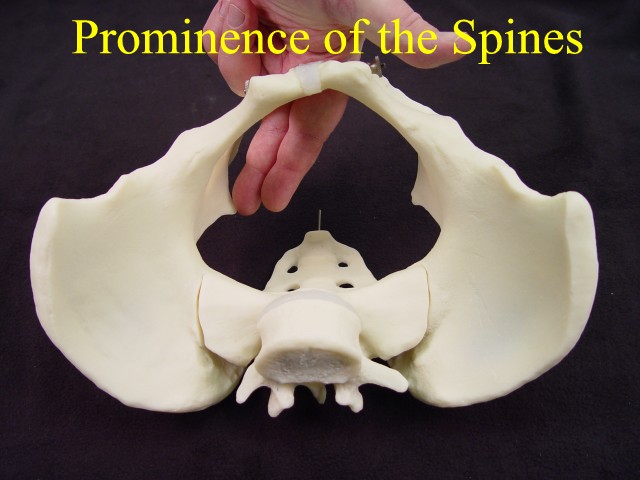
Feel the ischial spines for their relative prominence or flatness.
Spinal prominence narrows the transverse diameter of the pelvis.
-
Feel the pelvic sidewalls to determine whether they are parallel
(OK), diverging (even better), or converging (bad). True outlet
obstruction is fortunately rare.
X-ray Pelvimetry
This technique is primarily of historical interest. It was believed in
the past that accurate x-ray measurements of the pelvis would allow for
identification of those patients who would have disproportion. X-ray
pelvimetry (or CT pelvimetry) allows for reasonably accurate measures of
various internal measurements not available to clinical examination.
Among these ate the true obstetrical conjugate, transverse diameter of
the inlet, and bispinous diameter (transverse diameter of the midpelvis)..
In numerous studies since then, the usefulness of x-ray pelvimetry
has been discredited to the point that x-ray pelvimetry is rarely
performed today. The problem is not that the internal measurements
cannot be assessed with reasonable accuracy, but that the measurements
rarely have any clinical meaning. Vaginal delivery may still occur (and
usually does) despite small measurements. Cesarean section may still be
needed even if the internal measurements look acceptable. Finally, the
most contracted of pelvises can usually be defined on clinical
examination alone.
Occasionally, x-ray pelvimetry is still used. One example could be a
maternal history of pelvic deformity where the wisdom of allowing a
vaginal trial of labor is in question.
Estimation of Fetal Weight
Estimates of pelvic capacity and shape are only half of the fetopelvic
disproportion evaluation. The other half is the estimate of fetal size.
Estimates can be made by feeling the mother's abdomen, by ultrasound
scan estimates, or by asking the mother how big she believes the fetus
is.
 Ultrasound estimates of fetal weight are based on formulas that
weigh various fetal dimensions (biparietal diameter, abdominal
circumference, femur length, etc.), then apply mathematical modeling to
come up with an estimated fetal weight. Ultrasound estimates are
considered by many to be the most accurate means of predicting fetal
weight. Accuracy of ultrasound varies, but its predictions generally
come within 10% of the actual birthweight two-thirds of the time, and
within 20% of the actual birthweight in 95% of cases. That means that if
ultrasound predicts and average-sized, 7 1/2 pound baby, that most of
the time (95% of the time), the baby will weigh somewhere between 6
pounds and 9 pounds, and occasionally (5% of the time), the baby will
weigh less than 6 pounds or more than 9 pounds. We would all prefer that
ultrasound be more consistently reliable in its estimates of fetal
weight. Ultrasound estimates of fetal weight are based on formulas that
weigh various fetal dimensions (biparietal diameter, abdominal
circumference, femur length, etc.), then apply mathematical modeling to
come up with an estimated fetal weight. Ultrasound estimates are
considered by many to be the most accurate means of predicting fetal
weight. Accuracy of ultrasound varies, but its predictions generally
come within 10% of the actual birthweight two-thirds of the time, and
within 20% of the actual birthweight in 95% of cases. That means that if
ultrasound predicts and average-sized, 7 1/2 pound baby, that most of
the time (95% of the time), the baby will weigh somewhere between 6
pounds and 9 pounds, and occasionally (5% of the time), the baby will
weigh less than 6 pounds or more than 9 pounds. We would all prefer that
ultrasound be more consistently reliable in its estimates of fetal
weight.
Clinical estimates by an experienced examiner, based on feeling the
mother's abdomen, are, in some studies, just as accurate as ultrasound
(in other words, somewhat reliable). Interestingly, some studies also
demonstrate that the mother's guess about her own baby's size is also
about as accurate as ultrasound, if she has delivered a baby in the
past. If she hasn't, then her estimates are less accurate.
 Progress of Labor Progress of Labor
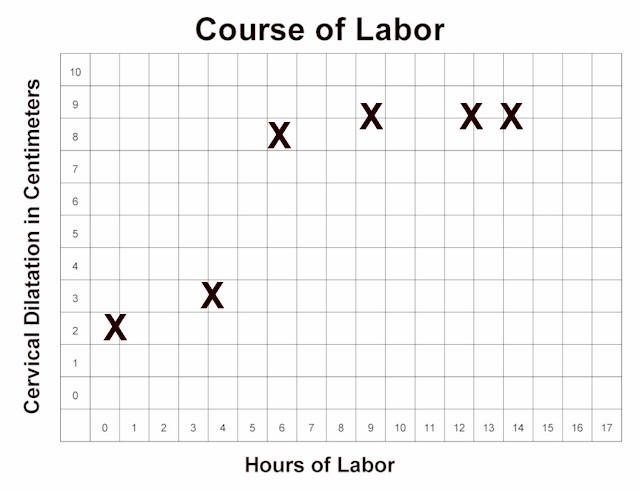
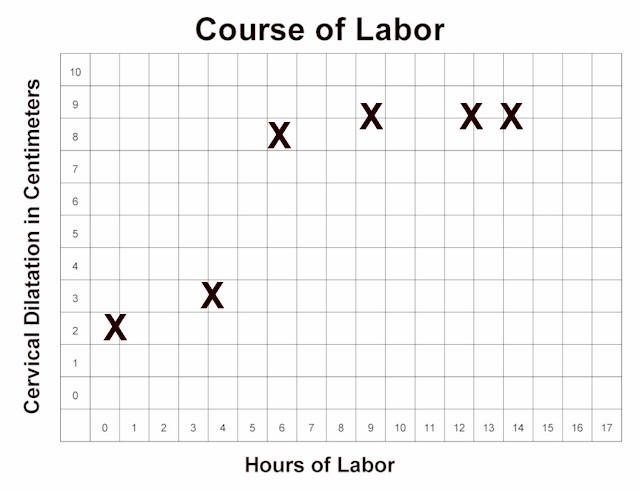
Monitoring the progress of labor is another technique that is used to
assess the presence or absence of fetopelvic disproportion. This
technique hinges on the belief that if the fetus is too big to come
through, there will be an arrest of progress of labor. After confirming
that the arrest is not due to other factors (inadquate contractions, for
example), and allowing adequate time for the arrest to resolve,
fetopelvic disproportion is presumed to be present and operative
delivery (usually cesarean section) is undertaken. Many physicians use a
"2-hour rule," depending on the clinical circumstances, to allow for
active labor to show advancement before resorting to cesarean section.
Others have different time frames in mind.
|