2-33. INTRODUCTION
The forms selected for discussion are those that provide basic information to the specialist concerning his work in the OR suite. The specialist checks the OR Schedule to identify the operations to which he is assigned. The specialist may obtain detailed information for the performance of his assigned tasks by referring to the procedure manual. The assignment roster may be prepared for the entire week, but the specialist should check it at least twice daily because a change in assignments may have been entered.
2-34. NURSING SERVICE PERSONNEL TIME SCHEDULE
a. Discussion. DA Form 3872, Nursing Service Personnel Time Schedule (see figure 2-2) is used to list the days on duty and off duty for all OR personnel. The NCOIC assists in the preparation of the time schedule for the OR specialists. The schedule is posted for one week at a time and is usually prepared several weeks in advance.
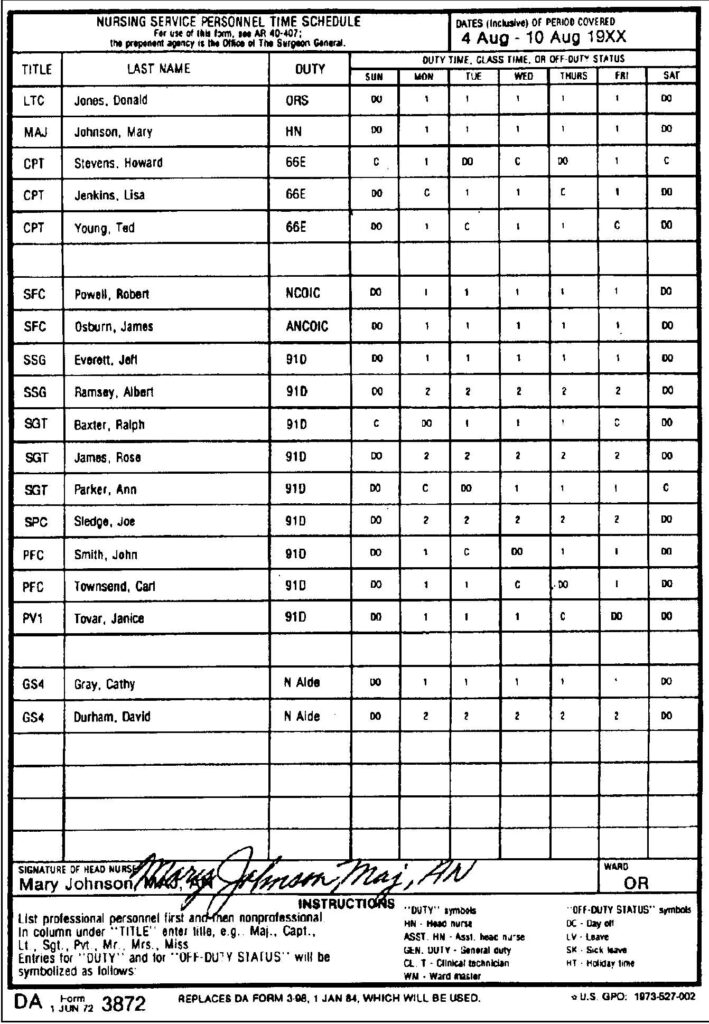
b. Need for a Time Schedule. The use of a time schedule enables the personnel responsible to plan for the adequate coverage of the suite at all times and enables personnel assigned to make plans ahead of time. If the hospital has a “call system” for coverage after normal duty hours, the time schedule should indicate the personnel who are “on call” for the week.
c. Coverage After Normal Duty Hours. All surgical suites must plan for adequate coverage in the event that emergency surgery must be performed after normal duty hours. In large OR suites, or in a hospital where a great deal of emergency work is done, coverage is provided by scheduling personnel on shifts around the clock. In surgical suites not using shifts, personnel should be placed “on call” to provide coverage for emergency operations. Some installations assign call personnel as well as having shifts. Persons on call must be highly skilled in all kinds of surgery since the types of emergency operations cannot be predetermined. The specialist taking call must be available within a very short time and must inform the person responsible for calling him of his whereabouts at all times. Local policy will indicate whether personnel taking call are to sleep in a room in the hospital or in quarters. The shifts and call duty are rotated frequently so that a person does not work the same shift all the time or take excessive call.
d. Planning for the Time Schedule. The time schedule is planned and prepared in order to provide an opportunity for the specialist to have learning experiences. This is accomplished by scheduling a person who needs further training to be on duty with a person having the appropriate training and experience. Such considerations make the planning and the preparation of the time schedule a difficult task.
e. Operating Room Specialist’s Requests Concerning Time Off. The OR specialist should write his routine requests for specific days off duty, for passes, and for leaves, and he should give such requests to the NCOIC before the time schedule is prepared. The specialist should not ask to have his time changed after the schedule has been prepared unless he has a true emergency. He should make all requests concerning his time to the NCOIC.
2-35. THE OPERATING ROOM SCHEDULE
a. Discussion. DD Form 1923, OR Schedule (see figure 2-3) is used for one day’s surgery. It contains the basic information needed by the scrub and the circulator in the planning and organization of their work for that day. In order to be able to use the information on the schedule, the specialist must know what each brief entry means in terms of his tasks as the scrub or the circulator. While studying the interpretation of the various entries on the schedule, refer to figure 2-3. NOTE: The OR schedule is distributed to all units concerned. In addition to the surgical suite, these include the surgical nursing units, the recovery room, the anesthesiology and operative service, the Chief, Department of Surgery, the commanding officer, the Chief, Department of Nursing, the Laboratory, the Department of Radiology, and the Chaplain.
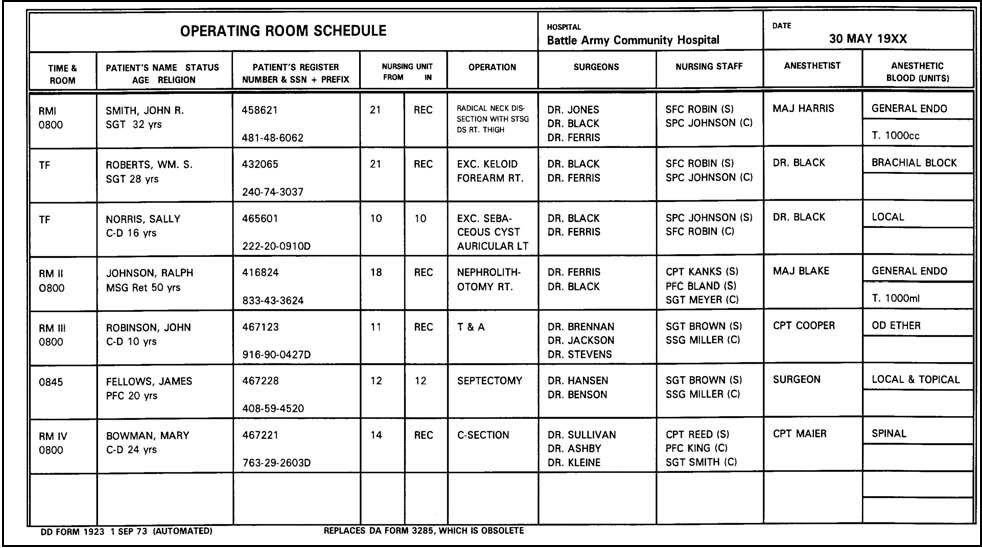
b. Room Number. (See figure 2-3). The individual ORs are assigned to the various surgical services by the OR Supervisor in coordination with the Chief Anesthesiologist and Chiefs of Surgical Services. For example, the general surgical service may use room one on Mondays, Wednesdays, and Fridays and the urology service may use the same room on Tuesdays and Thursdays. Such an arrangement enables greater efficiency and economy in the use of the equipment required by a particular service and also lets the scrub and the circulator know ahead of time what equipment will be needed in a room on a given day of the week.
c. Time. (See figure 2-3). The time entered means that the incision is to be made at that hour. The patient should have been previously anesthetized, positioned, prepared, and draped. Therefore, the scrub and the circulator should perform their tasks in the preparation of the room sufficiently ahead of time in order not to delay the case. To follow means “TF” when used in this column and indicates that the room is to be prepared as quickly as possible upon completion of the preceding operation. The time required for this preparation is about 20 minutes. (A patient whose surgery is scheduled “TF” is given the preoperative hypodermic “on call.”) That is, OR personnel will notify the ward nurse to give the hypodermic about 1/2 hour before the completion of the operation preceding the “TF” operation).
d. Patient’s Grade. (See figure 2-3). The patient’s grade is inserted following his name if he is a member of the Army; the abbreviation “ret” is added for retired personnel. The term “C-D” indicates civilian dependent. The inclusion of age is important to personnel in both the OR suite and the anesthesiology service. Children are scheduled before adults to avoid excessive dehydration in the children. In addition, the instruments required for the operation will likely be different when the patient is a child than when the same operation is to be performed on an adult. As an example, a hernioplasty on a child requires fewer and smaller hemostatic forceps and scissors than does this surgery on an adult.
e. Register Number. (See figure 2-3). The register number is used to help identify the patient. The circulator must see that it is entered on the pathology forms so that the specimen from a patient is properly identified (if two patients have identical names, the register number may be the only accurate means of identification). In Army hospitals, the social security account number is used (in addition to the register number) to identify the patient and his clinical records.
f. Nursing Unit. (See figure 2-3). The column headed “NURSING UNIT” indicates the location of the patient prior to surgery as well as the nursing unit to which he will be sent upon completion of his surgery. Patients who have been given general or spinal anesthesia are sent to the recovery room. Those who have been given local or regional block anesthesia are usually returned to their original-nursing units.
g. Operation. (See figure 2-3). The circulator and the scrub must know the location of the operative area and the site of the incision. These are often (though not always) obvious to the specialist if he knows the definition of the operation (see paragraphs 2-1 through 2-11). For an operation that might be performed using one of several sites for the incision, the incision site should be specified immediately following the name of the operation. Once the specialist is assigned to select the instruments for the case, he obtains the instrument card (see paragraph 2-31) for that operation and assembles the items recorded on the card. The inexperienced OR specialist may need to use references for an understanding of some operations, especially those named after individuals.
(1) Normally, Dorland’s Illustrated Medical Dictionary is available in every OR suite. This volume includes a brief description of operations named for the surgeon who originated or modified the procedure. These are examples: Albee’s operation–for ankylosis of the hip, consisting of cutting off the upper surface of the head of the femur, and so forth; Bergenhem’s operation–surgical implantation of the ureter into the rectum.
(2) Other more detailed references may also be available. Some books describe the operative procedure, the operative area, the site and kind of incision, the position, and the draping. One that includes these descriptions (and is established as an Army field manual) is Alexander’s Care of Patient in Surgery. This book also lists instruments and sutures necessary for operative procedures; however, these lists are not always applicable to all hospital ORs. NOTE: Many terms pertaining to an operation are abbreviated. As an example, in the listing, (see figure 2-3), of the radical neck dissection. “STSG. DSRT. THIGH” indicates that the patient will have a split thickness skin graft and his right thigh will be used as the donor site. If the specialist assigned to scrub or circulate for an operation is uncertain of the meaning of any abbreviation of the schedule, he should ask the NCOIC or an AN Officer. Operative procedures performed on a bilateral structure should always indicate the side of the procedure. T and A (see figure 2-3) stands for tonsillectomy and adenoidectomy. C-section is the abbreviation for cesarean section.
h. Surgeons. (See figure 2-3). The name listed first denotes the surgeon in charge of the operation. The names that follow are other MC Officers assigned in the order of first assistant, second assistant, and so forth.
(1) The circulator. The number of surgeons listed indicates to the circulator the number of gowns necessary. The circulator also finds out the glove sizes for the MC Officers listed.
(2) The scrub. Before scrubbing up, the scrub obtains the surgeon’s preference card (see paragraph 2-32) for the surgeon in charge of the operation. He follows the information on the card with regard to preparation of sutures and any special equipment listed. The scrub also determines what his position at the table should be in relation to this group–to the right or left of the surgeon and at which side of the operating table. In making this decision, the scrub considers a number of factors, including the following–the location of the operative area and any special needs imposed due to either the location or the nature of the surgery; the working habits and preference of the surgeon; the number of members of the sterile team and their tasks; and whether or not any members of the sterile team are left-handed. The scrub then sets up the Mayo stand, the back table, and the basin (ring) stand for his use in accordance with his position at the OR table. Note the grouping of the sterile tables in figure 1-30A, B, C, and D.
i. Nursing Staff. (See figure 2-3). The OR specialist and other OR personnel assigned to work on the cases are listed in the column headed “Nursing Staff.” “Scrub” and “circulate” may be abbreviated “S” and “C.” Duties of the scrub and the circulator include those set forth in paragraph 2-18. Whenever two team members are assigned to scrub, the first listed is the senior (or the more skilled) team member and the other serves as the assistant.
j. Anesthetist. (See figure 2-3). If the patient is to be given local infiltration anesthesia, the surgeon’s name is repeated in this column, or the word “surgeon” may be entered. For anesthesia administered by a member of the anesthesiology service, the name of the anesthetist assigned for the operation (either MC or AN Officer) is entered. The circulator should put a revolving stool in place for the anesthetist (see paragraph 1-17a and figure 1-15). If the surgeon is scheduled to administer the anesthetic agent, the circulator should see that a source of oxygen is available in the room. (The gas anesthesia apparatus provides this source of oxygen unless piped-in oxygen is available.)
k. Anesthetic. (See figure 2-3). The information entered in this column indicates whether a local or a general anesthetic will be given, the method of administration, and often the anesthetic agent to be used. The word “endo” (an abbreviation for endotracheal) is usually added if the anesthetist is going to intubate the patient (insert a tube which provides an artificial airway into the patient’s trachea by way of his nose or mouth). Additional time (15 or 20 minutes) is required for anesthetizing when a patient is to be intubated.
(1) The listing of the type of anesthetic may be of assistance in the selection of instruments. For example, an operation scheduled as “excision of keloid, right forearm” gives no information about the size of the surgical wound. If it is scheduled for local anesthesia rather than general, the specialist can safely assume that the incision will be small, to be closed without skin grafting.
(2) The letter “T” followed by a number of ml (1000, 1500 ml, and so forth) indicates that whole blood has been ordered from the laboratory and is available in the amount listed, and the patient has been typed and cross matched in anticipation of his need for a transfusion during the operative procedure.
l. Summary.
(1) Practice and experience will increase the student’s knowledge greatly. Both the scrub and the circulator can obtain much information from the references available in the OR suite. These references include the procedure manual, instrument card file, surgeon’s reference cards, the various DA Forms (especially the OR Schedule), standing operating procedures or policy file, and available dictionaries.
(2) The references listed serve to give assistance and direction to all members of the surgical team. The OR specialist enhances his value to other members of the surgical team and provides more effective care of the patient when he is able to interpret and apply the information available.