TEXT ASSIGNMENT Paragraphs 4-1 through 4-5.
TASKS TAUGHT
-
- 081-831-0046, Administer External Chest Compressions.
LESSON OBJECTIVES After completing this lesson, you should be able to:
4-1. Identify the proper procedures for performing one-rescuer CPR on an adult.
4-2. Identify the proper procedures for performing two-rescuer CPR on an adult.
4-3. Identify the proper procedures for switching positions while performing two-rescuer CPR.
4-4. Identify the proper procedures for switching from one-rescuer CPR to two-rescuer CPR.
4-5. Identify the causes of problems associated with CPR, including severe gastric distention, and how the problems can be corrected and/or prevented.
SUGGESTION After you have completed the text assignment, work the exercises at the end of this lesson before beginning the next lesson. These exercises will help you to achieve the lesson objectives.
4-1. ADMINISTER CARDIOPULMONARY RESUSCITATION TO AN ADULT USING THE ONE-RESCUER METHOD
There are two basic methods of administering cardiopulmonary resuscitation (CPR) to an adult casualty–the one-rescuer method and the two-rescuer method. The one-rescuer method is used when you have no one available to help you perform CPR. The two-rescuer method is used when you have an assistant available. The one-rescuer method is presented in this paragraph and the two-rescuer method is presented in paragraph 4-2.
In this paragraph, it is assumed that you have already moved the casualty to safety if required (paragraph 3-1), checked for spinal injury (paragraph 3-4), opened the airway and administered two ventilations (paragraphs 3-6 through 3-9), found the airway unblocked or have removed any blockage (Lesson 5), and have found the casualty’s carotid pulse to be absent (paragraph 3-11).
a. Position the Casualty on a Firm Surface. Chest compressions must be performed with the casualty lying on a firm surface. If you have not already placed the casualty on a firm surface, do so now. The casualty’s body should be in the same position as used in initiating rescue breathing (paragraph 3-5).
b. Position Yourself. Kneel at the side of the casualty’s chest.
c. Call for Help Again. If help has not arrived, call for help again. If an assistant is available, have him seek help (telephone, radio, and so forth). Remember, for the adult chain of survival (figure 4-1), you should phone first before initiating CPR.
d. Locate the Compression Area. Locate the site on the casualty’s chest where the force of the chest compression is to be applied. The method described below is normally used, but other methods can be used if they locate the same compression site.
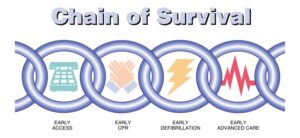
(1) Take the index and middle finger of your hand that is nearest the casualty’s feet and locate the lower edge of the casualty’s rib cage (figure 4-2A).
(2) Push your fingers along the lower edge of the rib cage toward the center of his chest until you come to a notch. The notch is the location where the ribs meet the sternum, and where the xiphoid process begins.
(3) Place the tip of your middle finger in the notch and against the bottom of the sternum.
(4) Place your index finger next to the middle finger and over the sternum (figure 4-2B). The index finger is now above the xiphoid process.
NOTE: The xiphoid process is a bone shaped somewhat like an arrowhead. It is located at the bottom of the sternum. Force is never applied directly to the xiphoid process.
(5) Place the heel of your other hand so that the thumb side is next to your index finger (figure 4-2C). The heel is now over the lower half of the sternum and covers the compression site. Having the long axis of the heel of your hand placed along the long axis of the sternum keeps the main line of the force of compression on the sternum only rather than on the sternum and the ribs together. This decreases the chance of fracturing a rib during chest compressions. This hand position also ensures that the heel of the hand is not over the xiphoid process. A fractured rib or a xiphoid process that has broken free of the sternum can result in damage to the heart, lungs, and/or major blood vessels. It is common, even with proper CPR, to fracture a rib or ribs in the process of good resuscitation. The 2005 AHA guidelines state that it is extremely important to ensure proper force and depth of compressions and that this outweighs the risk associated with fracturing ribs.
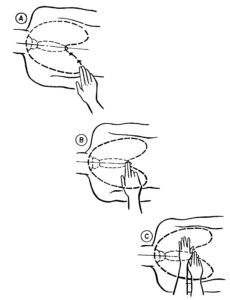
e. Position Hands for Compression. Lift your hand that is closest to the casualty’s feet (the one you ran along the bottom of the casualty’s rib cage) and place the heel of that hand on top of the hand that is on the compression site. The long axis of both heels should be parallel with the long axis of the sternum with the fingers of both hands pointing away from you. Either extend the fingers of both hands so that the fingers are straight or interlace your fingers. (Figure 4-3 shows the fingers interlaced.) Keep your fingers and palms off the casualty’s chest.
f. Position Your Body to Deliver Compressions. To be efficient and effective (the best heart compression for the least amount of energy expended), the thrust must be straight down. If the thrust is not straight down, the casualty’s body will tend to roll. Such a rolling motion will decrease the force of the compression, lead to early fatigue on your part, and could cause fractured ribs or a fractured xiphoid process.
(1) Lock elbows. Straighten your arms and lock your elbows. If your elbows are not locked, your arms will bend somewhat when you deliver the compression and your compression will not be as effective.
(2) Position shoulders over hands. Move your shoulders so that they are directly over your hands and directly above the casualty’s sternum. You will probably be at a point of imbalance when you assume this position. That is, you will feel that you would fall forward if you were not being supported by your hands on the casualty’s chest. This imbalance actually helps in performing external chest compressions since your weight is added to the force of the compressions.
g. Perform 30 Chest Compressions. A compression consists of a thrust which compresses the heart and a release which allows the heart to refill with blood. These compressions are delivered at a rate of approximately 100 per minute. Figure 4-3 shows a rescuer delivering chest compressions. It is recommended to push hard and fast to make sure adequate depth and rate of compressions are maintained.

(1) Thrust. When performing the thrust, keep your elbows locked and push straight down. Do not push with all of your strength, but do use enough force to push the casualty’s sternum down 1 1/2 to 2 inches (4 to 5 centimeters). Instead of pushing down using your muscles only, let the weight of your body move forward and use that force to help depress the sternum.
(2) Release. Releasing the pressure allows the heart to refill with blood. Release the pressure completely so that the sternum resumes its normal position, but do not remove the heel of your hand from the compression site.
NOTE: If you do lose the compression site, quickly repeat the procedures given in paragraphs d and e.)
(3) Rhythm. You should establish a definite rhythm when performing external chest compressions. The release part of the cycle should be equal in time to the thrust part of the cycle. Both parts should be distinct–do not “bounce.” Use a system to keep the compressions regular, smooth, and uninterrupted. One system for keeping track of the number of compressions administered is given below.
(a) Count out loud, “One and two and three and four and five and six and seven and eight and nine and ten and eleven and twelve and thirteen and fourteen and fifteen and….”
(b) Push down on the sternum when you say a number.
(c) Release the pressure when you say “and.”
h. Administer Two Breaths. Immediately after giving the thirtieth chest compression, move your hands to the casualty’s head, open his airway (paragraph 3-6), and administer two breaths (paragraph 3-9). Each breath should take about 1 second to administer. Observe the casualty’s chest out of the corner of your eye to make sure that the chest rises when you blow into the casualty’s mouth (or nose or stoma). The procedure should be completed within 3 to 5 seconds.
i. Prepare to Administer Chest Compressions. After the second breath, relocate the compression site (landmark) over the lower half of the casualty’s sternum. Use the procedure given in paragraph d. Do not guess where the site is located. Position your hands, lock your elbows, and move your shoulders over your hands.
j. Perform Four More Cycles of Cardiopulmonary Resuscitation. Administer four more CPR cycles. A one-rescuer CPR cycle is sometimes referred to as a 30:2 cycle. Each cycle consists of administering 30 chest compressions (paragraph g) followed by administering two breaths (paragraph h). You have now administered five complete CPR cycles (150 compressions and 10 breaths). About 2 minutes have elapsed since you began the first cycle.
k. Check for Pulse and Breathing. After you have administered the two full breaths of the fifth CPR cycle, check the carotid pulse (paragraph 3-11) again to see if his heart has resumed beating on its own. At the same time, check for signs that spontaneous breathing has resumed (paragraph 3-7). The check should take about 5 seconds. CPR should not be stopped for more than 10 seconds.
l. Evaluate Your Findings.
(1) If the casualty has resumed adequate breathing on his own, stop administering CPR and begin checking for other injuries. Remember to keep his airway open and check his breathing every few minutes if he does not regain consciousness. Resume administering rescue breathing or CPR if the breathing stops.
(2) If the casualty has a pulse, but has not resumed breathing on his own, proceed to administer rescue breathing (paragraph 3-12). Check the casualty’s pulse after every 12 breaths. If you find the casualty’s pulse to be absent, resume administering CPR.
(3) If the casualty does not have a pulse, give the casualty two full breaths and resume administering CPR. (Note: If there is no possibility of help arriving unless you make a telephone or radio call and a telephone or radio is readily available, quickly telephone or radio for help.) Continue to check for the return of pulse and breathing after every five cycles (5 cycles = approximately 2 minutes) of compression/ventilation.
m. Evacuate the Casualty. If possible, evacuate the casualty to a medical treatment facility. Continue administering CPR or rescue breathing en route if needed. If the casualty is breathing on his own, continue to observe him and be prepared to resume administering CPR since his condition could deteriorate rapidly without warning. Even if the casualty appears to recover, he needs to be examined by a physician as soon as possible.
n. Terminate Efforts, If Required. Keep administering CPR until one of the following occurs.
(1) The casualty’s heart resumes beating adequately on its own. (If this happens, continue rescue breathing.)
(2) The casualty’s heart resumes beating on its own and he also resumes breathing adequately on his own. (If this happens, look for injuries.)
(3) You are joined by another qualified person. (If this happens, change to two-rescuer CPR as described in paragraph 4-3.)
(4) You are relieved by a physician or other medical personnel. (If this happens, perform other duties as required.)
(5) You are ordered to stop by a physician or other qualified person authorized to pronounce the casualty as being dead. (In a military treatment facility, only a physician has this authority.)
(6) You are too exhausted to continue.
CAUTION: In general, when in the tactical environment, serious consideration should be given before administering CPR to the combat casualty. Cardiopulmonary resuscitation actions require your entire concentration and will prohibit you from attending to casualties that you may be able to save.
4-2. ADMINISTER CARDIOPULMONARY RESUSCITATION TO AN ADULT USING THE TWO-RESCUER METHOD
If you have another person qualified to administer CPR ready to help you, two-rescuer CPR should be performed. In two-rescuer CPR, one rescuer is responsible for administering chest compressions while the other rescuer is responsible for administering ventilations. In this paragraph, it is assumed that you have already moved the casualty to safety if required (paragraph 3-1), checked for responsiveness (paragraph 3-2), called for help (paragraph 3-3), checked for spinal injury (paragraph 3-4), and positioned the casualty on his back on a firm surface (paragraph 3-5). It is also assumed a soldier who is qualified to perform two-rescuer CPR has answered your call for help.
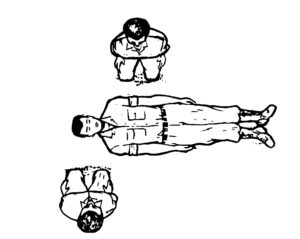
a. Position Yourselves. One rescuer positions himself at the side of the casualty’s head. This rescuer (called the ventilator rescuer from now on) will administer ventilations to the casualty. The other rescuer positions himself at the casualty’s chest on the opposite side from the ventilator rescuer (figure 4-4). The second rescuer (called the compressor rescuer from now on) administers the chest compressions. Rescuers should be on opposite sides of the casualty so that each rescuer has room to perform two-rescuer CPR. If both rescuers must be on the same side (in a ground ambulance, for example), both rescuers must be careful to avoid accidental contact which could interfere with the efficiency of their CPR efforts.
b. Evaluate Casualty. The ventilator rescuer (the rescuer at the casualty’s head):
(1) Opens the casualty’s airway (paragraph 3-6).
(2) Checks for signs of breathing (paragraph 3-7).
(3) Administers two full breaths if spontaneous breathing is not present and observes the casualty’s chest to make sure that it rises (paragraph 3-9).
(a) If the airway is blocked, the ventilator rescuer opens the casualty’s airway more and tries to administer two ventilations again. If the ventilations are unsuccessful, he tells the compressor rescuer to administer thrusts (paragraph 5-6f) while he (ventilator rescuer) performs finger sweeps (paragraphs 5-6c) as needed until the obstruction is removed.
(b) After the obstruction is removed, the ventilator rescuer administers two breaths and two-rescuer CPR is continued.
(4) Checks for a pulse by feeling the carotid artery for 5 to 10 seconds (paragraph 3-11).
(5) Informs the compressor rescuer of the need for chest compressions by saying, “No pulse,” if a pulse is not detected.
c. Prepare for Chest Compressions. While the ventilator rescuer is evaluating and ventilating the casualty, the compressor rescuer (the rescuer at the casualty’s chest):
(1) Locates the site for administering chest compressions (paragraph 4-1d).
(2) Positions himself to administer the compressions (paragraphs 4-1e and 4-1f).
d. Administer 30 Compressions. When the ventilator rescuer says, “No pulse,” the compressor rescuer administers 30 chest compressions at the rate of approximately 100 compressions per minute. The sternum is depressed 1 1/2 to 2 inches with each compression.
(1) The force of the compression should be delivered straight down without rocking the casualty. The fingers should not touch the casualty.
(2) The release part of the compression should be equal in time to the thrust part of the compression. Both parts should be distinct (no bounce).
(3) The compressor rescuer must keep his compressions regular and keep track of compression by counting out loud, “one and two and three and four and five and….” He must also push fast and hard to ensure a fast enough rate of compressions and adequate depth.
(a) The compressor rescuer pushes down on the sternum when he says a number.
(b) The compressor rescuer releases the pressure when he says, “and.”
e. Administer Two Breaths. After the compressor rescuer says “thirty,” the ventilator rescuer blows two breaths into the casualty’s mouth (or nose). This must be done while the chest compression is in the “release” portion. If the ventilator rescuer blows air into the casualty’s lungs while the compressor rescuer is performing the “push” portion of a chest compression, the actions would interfere with each other and be inefficient. Each ventilation should take about 1 second.
f. Continue Cardiopulmonary Resuscitation Cycles. After the ventilator rescuer administers the ventilations, the compressor rescuer administers 30 more chest compressions. Although there is a slight break between the last compression of a cycle and the first compression of the next cycle to allow for the ventilation, the compressor rescuer should not remove his hands from the casualty’s chest between cycles. While the compressor rescuer is delivering compressions, the ventilator rescuer feels the casualty’s pulse to ensure that the compressions are being effective. Both rescuers continue administering two-rescuer CPR cycles until 5 cycles have been administered. Each two-rescuer CPR cycle (sometimes called a 30:2 cycle) consists of thirty chest compressions followed by two full ventilations. At this rate, a casualty will actually receive about 150 compressions and 10 breaths after two minutes.
g. Check for Spontaneous Pulse and Respiration. After the first five cycles (2 minutes), the compressor rescuer stops administering compressions and the ventilator rescuer checks for spontaneous pulse and respiration. The check should take about 5 seconds.
(1) If the casualty has spontaneous heartbeat and respiration, the ventilator rescuer informs the compressor rescuer that the casualty is breathing on his own. The compressor rescuer then checks the casualty for injuries while the ventilator rescuer continues to maintain the casualty’s airway and monitor the casualty’s respirations and pulse.
(2) If the casualty’s heart is beating on its own, but the casualty is not breathing on his own, then the ventilator rescuer informs the compressor rescuer of the situation and begins administering rescue breathing. The compressor rescuer then checks for other injuries. If the casualty’s pulse stops again, two-rescuer CPR is resumed.
(3) If no pulse is detected after checking for 5 seconds, the ventilator rescuer opens the casualty’s airway, administers two breaths, and says, “No pulse.” The compressor rescuer resumes administering chest compressions and two-rescuer CPR is continued.
h. Continue Cardiopulmonary Resuscitation Cycles and Checks. If the pulse is absent, continue to administer two-rescuer CPR using the cycle of thirty chest compressions followed by two breaths. After administering CPR for about two minutes, both rescuers stop their efforts and the ventilator rescuer checks the casualty for spontaneous pulse and breathing. If the check shows no change, two-rescuer CPR is resumed. A check is made every five cycles (about every 2 minutes).
i. Switch When Needed. If the rescuer administering chest compressions becomes tired, the rescuers can switch functions. (Note: The same general procedures can be used if another qualified rescuer appears and wishes to give one of the rescuers a rest.) It is important to change compressors about every two minutes to ensure adequate rate and depth of compressions.
(1) The rescuer administering the chest compressions calls for the switch by counting “CHANGE and two and three and four and five…”
(2) After the compressor rescuer gives the thirtieth chest compression, he moves to the position for giving rescue breathing at the casualty’s head without moving to the casualty’s other side.
(3) The ventilator rescuer administers two breaths after the thirtieth compression and moves to the casualty’s chest without changing sides.
(4) The rescuer at the casualty’s head (formerly the compressor rescuer, now the ventilator rescuer) checks for spontaneous heartbeat and breathing (about 5 seconds).
(5) The other rescuer (formerly the ventilator rescuer, now the compressor rescuer) locates the chest compression site and positions himself to deliver chest compressions.
(6) If the casualty still has no pulse, the new ventilator rescuer says, “No pulse,” and administers two ventilations. The new compressor then begins administering chest compressions. Both rescuers continue to administer two-rescuer CPR.
(a) If the casualty’s heart has resumed beating but the casualty is not breathing, the new ventilator rescuer continues to administer rescue breathing while the other rescuer looks for injuries.
(b) If the casualty has spontaneous pulse and respiration, the new ventilator rescuer maintains the casualty’s airway and monitor his respirations and pulse, while the other rescuer checks the casualty for injuries.
j. Evacuate the Casualty. If possible, evacuate the casualty to a medical treatment facility. Continue administering CPR or rescue breathing as needed. If the casualty is breathing on his own, one must monitor his respirations and pulse closely, since his condition could deteriorate rapidly without warning.
k. Terminate Efforts, If Required. Keep administering CPR until one of the following occurs.
(1) The casualty’s heart is beating on its own.
(2) You are relieved by another qualified person.
(3) You are ordered to stop by a physician or other authorized person.
(4) You are too exhausted to continue your efforts.
4-3. CHANGE FROM ONE-RESCUER CARDIOPULMONARY RESUSCITATION TO TWO-RESCUER CARDIOPULMONARY RESUSCITATION
One of the first actions a lone rescuer takes is to call for help. If another person who is qualified to administer CPR comes to his aid after he has begun one-rescuer CPR, he can change from one-rescuer CPR to two-rescuer CPR. In the procedures given below, the original rescuer (the one administering one-rescuer CPR) is called the first rescuer. The new person coming to help the first rescuer is called the second rescuer.
a. Identify Self. The second rescuer informs the first rescuer that he is qualified to assist the first rescuer by saying, “I know CPR,” or a similar comment.
b. Kneel. The second rescuer positions himself on the opposite side of the casualty from the first rescuer in order to give each rescuer room to perform his functions and to lessen the chance of physical contact between the rescuers. The second rescuer then kneels near the casualty’s chest in position to administer chest compressions.
NOTE: The first rescuer continues to perform one-rescuer CPR while the second rescuer identifies and positions himself.
c. Administer Chest Compressions. After the first rescuer administers two full breaths to the casualty, the second rescuer administers thirty chest compressions. The first rescuer remains at the casualty’s head and checks the casualty’s carotid pulse to determine the effectiveness of the chest compressions.
(1) If the second rescuer’s chest compressions are actually causing the heart to pump blood, a pulse will be felt.
(2) If no pulse is felt within 5 seconds, the first rescuer informs the second rescuer that no pulse is being felt. The second rescuer then alters his compression technique so that a pulse is felt.
d. Continue Efforts to Aid Casualty.
(1) If the casualty has spontaneous heartbeat and respiration, one rescuer can check the casualty for additional injuries while the other rescuer continues to monitor the casualty.
(2) If the casualty’s heart is beating on its own but the casualty is not breathing on his own, the one rescuer administers rescue breathing while the other rescuer looks for injuries.
(3) If no pulse is detected after checking for 5 seconds, the first rescuer opens the casualty’s airway, administers two breaths, and says, “Continue CPR.” The second rescuer resumes administering chest compressions. Both rescuers now administer CPR using two-rescuer CPR cycles (thirty compressions followed by two ventilations). After five cycles, the rescuers again check for spontaneous heartbeat and respiration, and change positions.
(4) If the first rescuer is fatigued, the first rescuer administers two ventilations and tells the second rescuer to administer one-rescuer CPR. While the second rescuer is performing one-rescuer CPR, the first rescuer checks the effectiveness of the ventilations by observing the casualty’s chest, checks the effectiveness of the compressions by feeling for a carotid pulse, and (if needed) seeks additional help. When the first rescuer has recovered sufficiently, he informs the second rescuer that he will assist in administering two-rescuer CPR, positions himself by the casualty’s head, and checks for spontaneous heartbeat and spontaneous respiration (paragraph d).
4-3. CHANGE FROM ONE-RESCUER CARDIOPULMONARY RESUSCITATION TO TWO-RESCUER CARDIOPULMONARY RESUSCITATION
One of the first actions a lone rescuer takes is to call for help. If another person who is qualified to administer CPR comes to his aid after he has begun one-rescuer CPR, he can change from one-rescuer CPR to two-rescuer CPR. In the procedures given below, the original rescuer (the one administering one-rescuer CPR) is called the first rescuer. The new person coming to help the first rescuer is called the second rescuer.
a. Identify Self. The second rescuer informs the first rescuer that he is qualified to assist the first rescuer by saying, “I know CPR,” or a similar comment.
b. Kneel. The second rescuer positions himself on the opposite side of the casualty from the first rescuer in order to give each rescuer room to perform his functions and to lessen the chance of physical contact between the rescuers. The second rescuer then kneels near the casualty’s chest in position to administer chest compressions.
NOTE: The first rescuer continues to perform one-rescuer CPR while the second rescuer identifies and positions himself.
c. Administer Chest Compressions. After the first rescuer administers two full breaths to the casualty, the second rescuer administers thirty chest compressions. The first rescuer remains at the casualty’s head and checks the casualty’s carotid pulse to determine the effectiveness of the chest compressions.
(1) If the second rescuer’s chest compressions are actually causing the heart to pump blood, a pulse will be felt.
(2) If no pulse is felt within 5 seconds, the first rescuer informs the second rescuer that no pulse is being felt. The second rescuer then alters his compression technique so that a pulse is felt.
d. Continue Efforts to Aid Casualty.
(1) If the casualty has spontaneous heartbeat and respiration, one rescuer can check the casualty for additional injuries while the other rescuer continues to monitor the casualty.
(2) If the casualty’s heart is beating on its own but the casualty is not breathing on his own, the one rescuer administers rescue breathing while the other rescuer looks for injuries.
(3) If no pulse is detected after checking for 5 seconds, the first rescuer opens the casualty’s airway, administers two breaths, and says, “Continue CPR.” The second rescuer resumes administering chest compressions. Both rescuers now administer CPR using two-rescuer CPR cycles (thirty compressions followed by two ventilations). After five cycles, the rescuers again check for spontaneous heartbeat and respiration, and change positions.
(4) If the first rescuer is fatigued, the first rescuer administers two ventilations and tells the second rescuer to administer one-rescuer CPR. While the second rescuer is performing one-rescuer CPR, the first rescuer checks the effectiveness of the ventilations by observing the casualty’s chest, checks the effectiveness of the compressions by feeling for a carotid pulse, and (if needed) seeks additional help. When the first rescuer has recovered sufficiently, he informs the second rescuer that he will assist in administering two-rescuer CPR, positions himself by the casualty’s head, and checks for spontaneous heartbeat and spontaneous respiration (paragraph d).
4-5. SUMMARY OF CARDIOPULMONARY RESUSCITATION PROCEDURES
a. Check for responsiveness and for spinal injury.
b. Call for help; place casualty on his back and on a firm surface.
c. Open the airway.
d. Check breathing (look, listen, feel).
e. Give two breaths.
f. Check carotid pulse.
g. Locate compression site.
h. Administer CPR cycles (thirty compressions to two ventilations).
i. Check for spontaneous breathing and heartbeat after five cycles of 30:2 (about 2 minutes).
j. Continue CPR, rechecking for spontaneous breathing and heartbeat every minute.
k. Evacuate the casualty.