LESSON 3 Initiate Rescue Breathing on an Adult.
TEXT ASSIGNMENT Paragraphs 3-1 through 3-12.
TASK TAUGHT
-
- 081-831-0018, Open the Airway.
- 081-831-0048, Perform Rescue Breathing.
LESSON OBJECTIVES After completing this lesson, you should be able to:
3-1. Identify the steps (in sequence) for evaluating a casualty and initiating rescue breathing.
3-2. Identify the proper procedures (in sequence) for opening a casualty’s airway using the jaw-thrust method and the head-tilt/chin-lift method.
3-3. Identify the proper procedures (in sequence) for administering mouth-to-mouth, mouth-to-nose, and mouth-to-stoma rescue breathing.
3-4. Identify the proper procedures for taking a carotid pulse.
SUGGESTION After you have completed the text assignment, work the exercises at the end of this lesson before beginning the next lesson. These exercises will help you to achieve the lesson objectives.
But many non-medically trained individuals have been unwilling or unable to evaluate spontaneous respirations, find an accurate pulse, and initiate effective respiratory support promptly. These problems have led to significant delays in initiating chest compressions.
To overcome this problem, 2020 CPR guidelines for non-medical personnel omit rescue breathing, instead going directly to chest compressions in the unconscious adult. Compression-Only CPR can still be very effective because of the emphasis on prompt delivery of oxygen to the brain, even if the oxygen concentration in the blood is not optimal.
3-1. REMOVE CASUALTY FROM ANY IMMEDIATE DANGER
If you see a possible casualty, you must evaluate the person to determine if rescue breathing should be initiated. Before you begin the evaluation procedure, however, evaluate your surroundings to determine the appropriate care for those surroundings. If you are in the “care under fire” phase of care, then opening the airway and controlling bleeding are your primary concerns; rescue breathing will not be initiated at this time. If other danger exists in the non-tactical environment, the hazards must be assessed for threat to life.
If a major life threat exists, then moving the patient prior to further evaluation and treatment would be necessary. Cardiopulmonary resuscitation is not considered an appropriate treatment under most battlefield conditions because most of these patients will be traumatized in a manner that would not support life without immediate and extensive surgery.
NOTE: The steps for evaluating a casualty and initiating rescue breathing are the same as for initiating cardiopulmonary resuscitation. These are also the same steps normally used to evaluate any casualty.
3-2. CHECK FOR RESPONSIVENESS
Establish responsiveness by using the AVPU system. Check to see if the patient is alert (A), responsive to verbal commands (V), responds to pain (P), or is unresponsive (U). Establishing responsiveness will usually take between 4 to 10 seconds.
CAUTION: If the casualty was injured in a motor vehicle accident, in a parachuting accident, in a diving accident, by a fall, by a blow to the back, or by some other violent incident that could result in injury to the back, take proper spinal precautions in treating the casualty. Be careful not to violently shake or move any patient. This will help to prevent aggravation of any injuries that may be present.
a. If the casualty answers, he is conscious and breathing, continue your examination of the casualty and render whatever aid is needed. (Evaluation and treatment procedures for injuries are presented in other 91W10 subcourses.)
b. If the casualty does not respond, he is unconscious. Perform the evaluation and treatment procedures given in the following paragraphs.
3-3. CALL FOR HELP
If the casualty does not respond (unconscious), attempt to obtain additional medical help. Do not leave the casualty to obtain help.
a. If you are alone with the casualty, shout for help. In the tactical setting, this would not be practical and other methods of signaling should be considered.
b. If another person is available, and if a radio or telephone is available, have the person use the radio or telephone to summon medical help. If you are alone, use the radio or telephone to call for help and return to the casualty and begin medical help.
c. If someone who is not medically trained is available, send him to get additional medical help.
d. If you are in a hospital and find an unconscious patient, summon help using available systems. These systems may include bells, lights, verbal calls for assistance, codes to alert medical personnel, and intercoms.
3-4. CHECK FOR SPINAL INJURY
Check the casualty for a spinal injury. If the casualty has a spinal injury, minimize any additional movement of the casualty (using the jaw-thrust method of opening the airway rather than the head-tilt/chin-lift method, for example). Moving a casualty with a fractured spine may cause additional damage to the spinal cord, which could result in paralysis or even death. If you suspect a spinal injury, perform your efforts as though you knew that a fracture of the spine were present. Do not try to straighten a fractured spine. Signs of spinal injury include:
a. Bruises and/or swelling over the spinal area.
b. Casualty lying in an abnormal (deformed) position.
c. Fluid draining from one or both ears.
3-5. POSITION THE CASUALTY
Position the casualty flat on his back and on a hard surface. Rescue breathing is most effective when the casualty is lying on his back. Chest compressions (part of CPR) are not effective unless the casualty is lying on his back and lying on a hard surface.
a. If the casualty is lying on a bed or cot, remove the casualty from the bed or cot and place him on the floor or ground. An alternative is to place a bed board or long backboard between the casualty’s back and the bed or cot.
b. If the casualty is lying on the ground in a supine (on his back) position, place his arms at his side and proceed to establish an open airway.
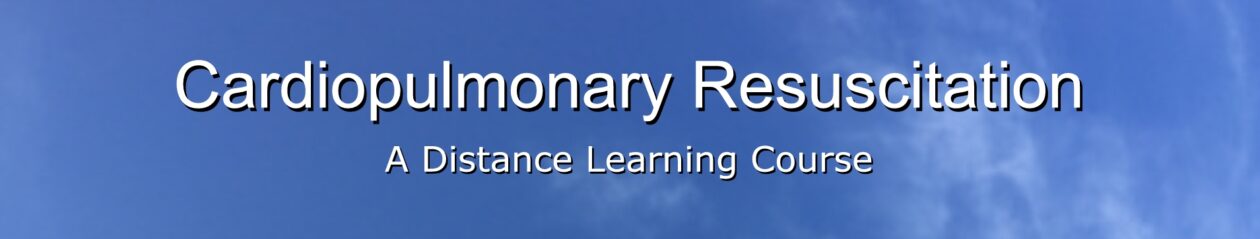
c. If the casualty is lying on solid ground in a prone (on his chest) position, turn him onto his back using the procedures given below. These procedures allow the casualty to be turned as a unit. Turning the casualty as a unit minimizes the likelihood that existing injuries will be aggravated, and also minimizes the chances that the head or neck will be injured during the turning. It is especially important to use these procedures if you suspect that the casualty has a spinal injury.
(1) Straighten the casualty’s legs.
(2) Kneel beside the casualty. Your knees should be near his chest area, but there should be enough space between you and the casualty for you to roll him onto his back.
(3) Take one of the casualty’s arms and move it so that the arm is straight and above his head. Then move his other arm so that it is also straight and above his head.
(4) Support the casualty’s head and neck by placing your hand that is nearest his head on the back of his head (figure 3-1A).
(5) With your other hand, reach across the casualty’s back and grasp the casualty’s uniform under his far arm.
(6) Pull on the casualty’s uniform and roll the casualty toward you (figure 3-1B). Use a steady and even pull so that the casualty’s head and neck stay in line with his back. (If you have a person to assist you, have the person to help roll the casualty’s hips and legs.)
(7) Once the casualty is lying flat on his back, return the casualty’s arms to his side (figure 3-1C). If his legs are crossed, uncross them.
3-6. OPEN THE AIRWAY
Once the casualty is in position for rescue breathing, open the casualty’s airway using either the head-tilt/chin-lift method or the jaw thrust method. Sometimes an unconscious casualty who is not breathing or breathing in a weak manner will resume normal respiration when his head is positioned correctly and his airway is opened. This is especially true if the casualty’s tongue is blocking the airway. The tongue is the most common cause of airway obstruction in unconscious casualties. Repositioning (lifting) the lower jaw forward lifts the tongue away from the back of the throat and unblocks the airway. Establishing an airway should take between 3 and 5 seconds.
NOTE: An unconscious casualty does not “swallow his tongue.” The muscles of the tongue simply relax and slide to a lower position which results in the pharynx being blocked.)
a. Head-Tilt/Chin-Lift Method. The head-tilt/chin-lift (figure 3-2) is the preferred method of opening the casualty’s airway if a neck fracture is not suspected. In addition, loose dentures can be handled easier using the head-tilt/chin-lift method.

(1) Kneel at the side of the casualty’s head or shoulders.
(2) Place your hand (the hand closest to the casualty’s head) on his forehead.
(3) Apply firm, backward pressure with the palm of your hand. This pressure will cause the casualty’s head to tilt back.
(4) Place the fingertips of your other hand under the bony part of his chin, not on the soft flesh under his chin. Pressing on the soft flesh under the chin could result in blocking his airway.
(5) Lift his chin with your fingertips. Continue to lift the lower jaw until his upper and lower teeth are almost brought together. The mouth should not be closed as this could prevent air from entering the casualty’s airway.
b. Jaw-thrust Method. The jaw-thrust (figure 3-3) is the preferred method of establishing an airway if you suspect that the casualty has a fractured neck. The jaw-thrust method moves the casualty’s tongue forward (away from the airway) without extending his neck.

(1) Kneel behind the casualty’s head.
(2) Rest your elbows on the surface on which the casualty is lying.
(3) Place one hand on each side of the casualty’s head.
(4) Place the tips of your index and middle fingers under the angles of the casualty’s jaw. (This is done on both sides of the casualty’s jaw.)
(5) Place your thumbs on the casualty’s jaw just below the level of the teeth. The thumbs will keep the casualty’s head from turning or tilting during the lift.
(6) Lift the jaw upward with your fingertips. The mouth should not be closed as this could prevent air from entering the casualty’s airway. Use your thumb to retract the casualty’s lower lip if needed.
(7) If the lift does not open his airway (tongue is still blocking the airway), lift the jaw up a little further. If this is unsuccessful, tilt the casualty’s head backward very slightly. In accordance with (IAW) American Heart Association (AHA) guidelines 2005, if you are unable to obtain an airway with the jaw-thrust method, the head-tilt/chin-lift method should be used. The importance of maintaining a patent airway outweighs the risk of spinal damage.
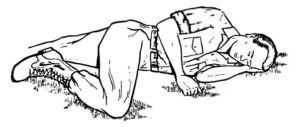
3-7. CHECK FOR BREATHING
Check to see if the casualty is breathing adequately (figure 3-4). Many times, opening the airway is all that is necessary to restore breathing in an unconscious casualty. This check usually takes 3 to 5 seconds to perform. Keep maintaining the casualty’s airway (head-tilt/chin-lift or jaw-thrust) while you perform the check.
NOTE: This is the first time that you actually check to see if the casualty is breathing adequately. Even if an unconscious casualty is breathing when you find him, his breathing could deteriorate or stop altogether while you are performing other measures if you do not take the precaution of positioning him so that his airway stays open.
a. Place your ear over the casualty’s mouth and nose and look towards the casualty’s chest. For the best results, your ear should be almost touching the casualty.
b. Look at the casualty’s chest. If the casualty is breathing, you should be able to see the chest rise and fall.
c. Listen for the sound of breathing (air being inhaled and exhaled).
d. Feel for the flow of air on the side of your face caused by the casualty exhaling

3-8. EVALUATE YOUR FINDINGS
a. If your check shows that the casualty is not breathing, try to open his airway again and check for breathing a second time. If he is still not breathing, begin administering ventilations immediately (paragraph 3-9).
b. If your check shows that the casualty is breathing, asses the rate and quality of breathing. Just because a casualty is breathing does not ensure that the depth of breathing or the rate are adequate to support life. (If the casualty is breathing 4 times per minute, he is technically breathing; but this rate is not adequate to sustain the casualty’s life). If the casualty has adequate breathing, consider inserting an airway adjunct to help control and protect the casualty’s airway. If available, oxygen should be administered at this time. Continue to examine the casualty for injuries while maintaining his airway. Check on his breathing periodically. Reopen the airway and perform rescue breathing should the casualty stop breathing.
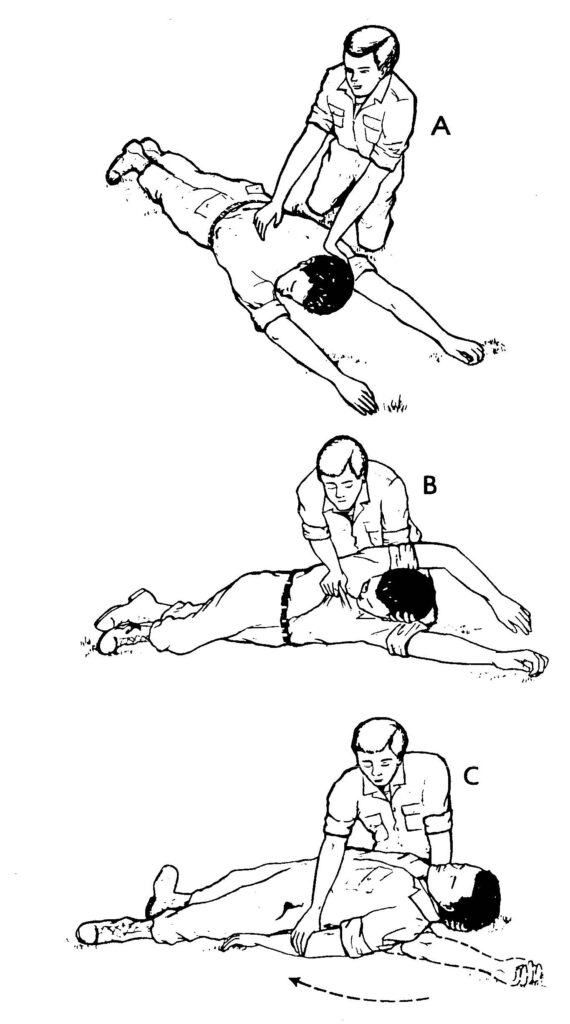
(1) If the casualty regains consciousness, place him in the left lateral recumbent position (figure 3-5) if no other injuries are present.
(2) If the casualty is unconscious and you have an oropharyngeal airway (OPA or J-tube) available, you can insert the airway to prevent the casualty’s airway from being blocked by his tongue. Remove the airway when the casualty begins to regain consciousness.
(a) Make sure that you insert the correct size of airway. Place the oropharyngeal airway along the outside of the casualty’s jaw. The airway should reach from the bottom tip of his ear to the corner of his mouth.
(b) Open the casualty’s mouth. If you have difficulty in opening his mouth, place your crossed thumb and index finger on the casualty’s upper and lower teeth near a corner of his mouth and push until his teeth separate and his mouth opens.
(c) Place the tip end (not the flanged end) of the oropharyngeal airway into the casualty’s mouth so that the tip points toward the roof of the casualty’s mouth.
(d) Slide the airway along the natural curvature of the tongue.
(e) When the tip of the airway reaches the back of the tongue past the soft palate, rotate the airway 180 degrees so the tip of the airway points down toward his throat.
(f) Advance the airway until the flange rests on the casualty’s lips.
(3) If the casualty has an intact gag reflex but can still not protect his airway, insert a nasopharyngeal airway.
(a) Ensure the airway is the correct size by measuring the diameter of the airway with the patient’s fifth finger (pinky) and the correct length by measuring the airway from the corner of the patient’s nostril to the tip of the ear.
(b) Lubricate the airway.
(c) Insert the airway in to the patient’s right nostril with the bevel towards the septum. This is anatomically the larger nostril in most people, and the curve of the airway is designed to be inserted in this side. Insert the airway by pushing it towards the back of the patient’s head until the flange rests on the casualty’s nare.
3-9. ADMINISTER TWO BREATHS
If the unconscious casualty is not breathing, you will need to perform rescue breathing. Rescue breathing procedures are also called “ventilating the casualty.” Ventilation simply means that you are supplying the casualty’s lungs with fresh air.
Even though the air comes from your lungs, it still contains plenty of oxygen. Room air contains about 20 percent oxygen; we use about 4 percent of this leaving 16 percent oxygen available to the patient when mouth-to-mouth rescue breathing is conducted. The mouth-to-mouth technique of rescue breathing is normally used.
An alternate technique, the mouth-to-nose method, is used when the casualty has a serious mouth or jaw injury, when the casualty’s mouth cannot be opened, or when you are unable to achieve a tight seal around the casualty’s mouth. Check for the presence of a stoma (an artificially-created opening in the neck and trachea). A stoma allows air exchange when the casualty’s upper airway is blocked due to surgery or a medical condition such as cancer. If a stoma is present, perform mouth-to-stoma rescue breathing. Cover the patient’s mouth and nose when conducting mouth-to-stoma breathing to make sure the air does not escape through this route instead of entering the lungs.
As you administer the two ventilations, observe the casualty’s chest out of the corner of your eye to see if the chest rises and falls. It should take about one second to blow a breath into the casualty’s lungs. Allow time between breaths for the chest to fall and the casualty to exhale. Avoid over inflation of the lungs, which can cause complications, including gastric distention, and can also increase the intra-thoracic pressure, making it difficult for blood to return to the fill the heart.
a. Mouth-to-Mouth. Mouth-to-mouth rescue breathing (figure 3-6) is also called mouth-to-mouth resuscitation. The following steps assume that you are maintaining the airway using the head-tilt/chin-lift method.
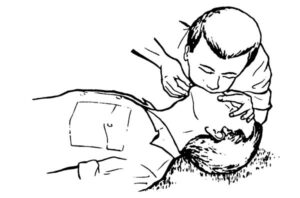
(1) Maintain airway. Keep the casualty’s airway open (patent) by maintaining the head-tilt/chin-lift.
(2) Inhale. Take a deep breath.
(3) Pinch the nose. Use the thumb and index finger of your hand that is on the casualty’s forehead to pinch his nostrils closed so that air will not escape when you blow air into his mouth. Keep the heel of your hand on the casualty’s forehead and continue to apply enough pressure to maintain the head tilt. The fingertips of your other hand remain under the casualty’s chin and continue to keep the chin lifted.
(4) Seal the mouth. Place your mouth over the casualty’s mouth. Cover his mouth completely and make sure that your mouth forms an airtight seal so that air will not escape when you blow air into his mouth.
(5) Deliver the first breath. Blow a breath at a slow rate into the casualty’s mouth. (Maintaining the open airway will keep the casualty’s mouth slightly open.) If the airway is truly open, the chest should rise as his lungs fill with air.
(6) Take another deep breath. After blowing into the casualty’s mouth, quickly break the seal over his mouth, take a breath of air, exhale, and then take another deep breath. The casualty’s chest should fall as air escapes from his mouth after you break the seal. You may be able to hear or feel the exhaled breath also.
(7) Seal the mouth. Seal your mouth over the casualty’s mouth again so that air will not escape.
(8) Deliver the second breath. Blow another breath into the casualty’s mouth at a slow rate. Observe the casualty’s chest.
(9) Break the seal and release nose. After delivering the second breath, break the seal over the casualty’s mouth and release the nose. The casualty’s body will exhale without further effort on your part.
b. Mouth-to-Nose. The mouth-to-nose rescue breathing (figure 3-7) is also called mouth-to-nose resuscitation.

(1) Maintain airway. Keep the casualty’s airway open by keeping the chin lifted.
(2) Inhale. Take a deep breath.
(3) Close the mouth. Use the hand that is lifting the casualty’s jaw to close the casualty’s mouth. No air should escape through the casualty’s mouth when you perform your ventilations. Continue to keep the jaw in a “lifted” position. (If the head-tilt/chin-lift is being used, maintain the pressure on the forehead with your other hand to keep the casualty’s airway open.)
(4) Seal the nose. Place your mouth over the casualty’s nose. Make sure that your mouth forms a seal so that air will not escape when you blow air into his nose.
(5) Deliver the first breath. Blow a breath into the casualty’s nose at a slow rate. If the airway is open, the chest will rise as his lungs fill with air.
(6) Take another breath. After blowing into the casualty’s nose, quickly break the seal over his nose, take a breath of air, exhale, and take another deep breath. His chest should fall somewhat as air escapes from the casualty’s nose after you break the seal. You may be able to hear or feel the exhaled breath also.
(7) Seal the nose. Seal your mouth over the casualty’s nose again so that air will not escape.
(8) Deliver the second breath. Blow another breath into the casualty’s nose at a slow rate and observe the casualty’s chest.
(9) Break the seal and open mouth. After delivering the second breath, break the seal over the casualty’s nose and allow his mouth to open slightly while continuing to maintain the open airway. (The mouth is opened in case there is an obstruction in the casualty’s nasal passages.) The casualty’s body will exhale naturally without effort on your part. If the mouth does not open readily, use your thumb to depress the lower lips slightly to separate the lips.
c. Mouth-to-Stoma. The mouth to stoma rescue breathing is used if a permanent or temporary opening has been made at the front base of the neck in order to open the airway to the atmosphere.
(1) Inhale. Take a breath.
(2) Close the mouth and nose, if needed. Use a hand to close the casualty’s mouth and nostrils in order to prevent air escaping.
(a) This step is not needed if the casualty’s upper airway has been closed surgically, as shown in figure 3-8.

(b) If the casualty has a temporary tracheostomy tube in the trachea, the tube may have a cuff that can be inflated to seal off the airway above the stoma and thus prevent air from escaping through the mouth or nose.
(3) Seal the stoma. Place your mouth over the casualty’s stoma. Make sure that your mouth forms an airtight seal so that air will not escape when you blow air into the stoma.
(4) Deliver the first breath. Blow a breath into the stoma. His chest should rise as his lungs fill with air.
(5) Take another breath. After delivering the first breath, quickly break the seal over the stoma, take a breath of air, exhale, and then take another breath. His chest should fall somewhat as air escapes from the stoma after you break the seal. You may be able to hear or feel the exhaled air also.
(6) Seal the stoma. Seal your mouth over the stoma again so that air will not escape.
(7) Deliver the second breath. Blow another breath at a slow rate into the stoma and observe the casualty’s chest.
(8) Break seal. After delivering the second breath, break the seal over the stoma. If you are holding the casualty’s mouth and nose closed, you can release them. The casualty’s body will exhale naturally.
3-10. EVALUATE THE EFFECTIVENESS OF THE TWO VENTILATIONS
a. Spontaneous Breathing Resumes. If the casualty begins breathing again on his own, check his circulation and continue your assessment. Do not leave the casualty since his breathing may stop again. The casualty may still require help to keep his airway open.
b. Airway Blocked. If the casualty’s chest did not rise and fall, then fresh air is not getting into his lungs. Reposition the casualty’s airway in an attempt to open the airway. Then administer two breaths again using the same procedures. If the casualty’s chest still does not rise, he probably has an object blocking his airway. Remove the obstruction using finger sweeps and manual thrusts as described in paragraph 5-6. Once the obstruction has been removed, administer two full breaths and proceed to check the casualty’s pulse (paragraph 3-11).
c. Airway Open with No Spontaneous Breathing. If air goes in and out of the casualty’s lungs (airway open) but he does not start breathing on his own, check his pulse (paragraph 3-11) and determine if chest compressions are required.
3-11. CHECK CAROTID PULSE
Check the casualty’s pulse after you have successfully administered the two initial ventilations. Getting fresh air into the casualty’s lungs will not help if his heart is not beating and the blood is not circulating.
There are two major arteries, called the carotid arteries, in the neck. One artery lies in a grove on the left side of the trachea (windpipe); the other lies in a groove on the right side of the trachea. Either artery may be used to check the casualty’s carotid pulse, but you will normally use the artery on the side of the neck closest to you.
The carotid pulse is used because you are already near the neck, it is easily accessible, and a pulse can sometimes be felt at the carotid artery when the pulse may be too weak to be detected at arteries farther from the heart. It is also typical to check the radial pulse at the same time as the carotid pulse.
a. Locate Pulse Site. Place the index and middle fingers of your hand on the casualty’s trachea or larynx. Then slide your fingers toward you while gently pressing on the neck until you find the groove running parallel to the airway (figure 3-9).
(1) If you are using the chin-lift/head-tilt, remove your hand from the casualty’s chin and use that hand to locate the pulse site. Keep your other hand on his forehead and maintain the head-tilt.
(2) If you are using the jaw-thrust, use your dominant hand to check for a pulse while maintaining the casualty’s airway with the other hand.
(3) Three fingers (index, middle, and ring fingers) can be used instead of only two fingers.
CAUTION: Do not use your thumb. The thumb has a detectable pulse and you may mistake the pulse in your thumb for the casualty’s pulse.
b. Feel for Pulse. Press gently on the carotid artery with your fingertips. Allow enough time to detect a pulse that is weak, slow, and/or irregular. The check should take between 5 and 10 seconds.

c. Evaluate the Pulse Check.
(1) If no pulse can be felt, cardiopulmonary resuscitation is required immediately. The procedures for administering cardiopulmonary resuscitation are given in Lesson 4.
(2) If a pulse can be felt, determine the rate and quality of the pulse. Ensure that the pulse is adequate to sustain life. (A pulse of less than 40 beats per minute [BPM] is not adequate to sustain life in most adults and CPR should be started.) Administer the rescue breathing procedures given in paragraph 3-12.
3-12. CONTINUE RESCUE BREATHING
If the casualty’s heart is beating adequately and he is not breathing on his own, continue to administer rescue breathing. Administer ventilations (breaths) at the rate of 1 ventilation about every 5 seconds (10 to 12 ventilations per minute). Keep the casualty’s airway open, while performing the ventilations and continue to monitor the casualty’s pulse.
a. Perform Ventilations. Administer ventilations using the mouth-to-mouth, the mouth-to-nose, or the mouth-to-stoma method, as appropriate. Ventilations can also be provided with the bag-valve-mask or other equipment that is discussed in other subcourses. The steps given below assume that the mouth-to-mouth method is being used with the head-tilt/chin-lift. Adjust the procedures as needed if another combination is being used.
(1) Take a breath.
(2) Pinch the casualty’s nostrils closed using the thumb and index finger of the hand on his forehead.
(3) Place your mouth over the casualty’s mouth, making sure that a tight seal is formed.
(4) Blow into the casualty’s mouth at a slow rate. As you blow, observe his chest. If his chest does not rise, a sufficient amount of air is not getting into his lungs. This may be caused by an inadequate positioning of his airway, by air leaking from the casualty’s nose, by air leaking from around your mouth, or by the breath not being delivered with sufficient force. If a problem exists, correct the problem and continue administering ventilations.
(5) Remove your mouth from around the casualty’s mouth and release his nose. This allows him to exhale. Remember, the casualty’s airway must be kept open so he can exhale.
(6) Inhale and exhale a small breath for yourself if you need to do so.
(7) Repeat the above procedures at a rate of one ventilation every 5 seconds until you have completed 10 to 12 ventilations.
b. Recheck Pulse. Recheck the casualty’s carotid pulse after every 10 to 12 breaths (about every minute). As you check his pulse, also look, listen, and feel for signs that the casualty has begun to breathe on his own.
(1) If the pulse is absent, begin administering chest compressions (Lesson 4).
(2) If the casualty begins breathing on his own, maintain his airway and check for other injuries. If the casualty remains unconscious, an oropharyngeal airway may be inserted. Monitor the casualty’s respirations in case he stops breathing again. The casualty will need to be evacuated for further evaluation and treatment by a physician.
(3) If the casualty still has a pulse but is not breathing on his own, continue to administer rescue breathing and recheck the pulse, after every 12 ventilations. Continue until the casualty begins breathing on his own, you are relieved by another qualified person, you are ordered to stop, or until you are too exhausted to continue.
NOTE: In a hospital, only a physician can order that resuscitation efforts be stopped.