1-8. MAJOR GROUPS
Before being used for a transfusion, blood must be typed and cross-matched to assure compatibility between the blood of the person who gets the transfusion and the type of blood being used. The most well known of the groupings is the A-B-O group.
1-9. A-B-O GROUP
Each person has either type A, B, AB, or O. The most common types in America are type 0 (45 percent) of the population and type A (41 percent). The blood type indicates the presence or absence of certain antigens. These antigens stimulate the body to produce antibodies. The antibodies react with their antigens to form agglutination or little clusters (clumps) in the blood. When a person has type A blood, his blood contains antibodies for type B, but none for type A. The opposite is true if he has type B blood. That is, the person would have antibodies for type A, but none for type B. If a person has type AB blood, he has neither type A nor type B antibodies and can receive type A, B or AB blood. Type O blood causes no antibodies to be formed and thus can be used to infuse any A-B-O group person. Figure 1-5 shows these relationships.
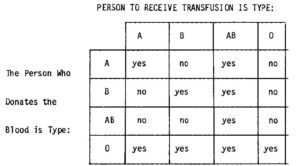
a. A type AB person is generally called “the universal recipient,” and a person with type O blood is generally called the “universal donor.”
b. A universal recipient is a person whose blood does not try to fight off the blood cells from any A-B-O source. Thus, it makes no difference which A-B-O type blood he receives. He can generally accept them all without adverse effect.
c. A universal donor is a person whose blood is well accepted by any A-B-O type person. This blood generally causes no adverse effects on the blood of any A-B-O type person who receives it. Because of this unique property, the universal donor is frequently asked to make blood donations.
1-10. Rh FACTOR
Many other flood factors have been isolated. The first one discovered (and the most important one) is the Rhesus (Rh) factor. The name “Rhesus” is taken from the name of the Indian rhesus monkey. This factor was first isolated from experiments with these monkeys. Each person is either Rhesus positive or Rhesus negative, depending on whether he has or does not have antigens for the Rh factor. Rh-positive people have these antigens while Rh-negative people do not (unless they have been transfused with Rh-positive blood). The amount of transfusion required to produce this reaction varies with the individual. A true “universal donor” would generally be type O and Rh-negative.
Serious problems because of the Rh factor can occur during pregnancy if the mother is Rh-negative and he fetus is Rh-positive. Small numbers of the child’s red cells escape from the placenta and enter the mother’s blood stream. This will cause no problem during the first pregnancy, but she will form antibodies. If she is also carrying a Rh-positive child during the second or subsequent pregnancies, the antibodies from her blood will attack the blood of the fetus and cause anemia in the fetus. Some possibilities are open for countering this problem. The baby can be transfused with Rh-negative blood at birth or anti-Rhesus immune globulin injections can be given to the mother. The stage of the pregnancy when the situation is discovered will usually determine which procedure should be used.
1-11. OTHER BLOOD GROUPS
Other factors (or groups) have varying effects on the blood, but none have the impact of the A-B-O or the Rh factors. These factors have names such as “Cartwright,” “MN,” “Lewis,” “He,” “Kell,” and “Wright.” Some factors may cause hemolytic disease in newborns. Some of these factors may present problems in organ transplants. The incidence of problems is normal use for blood transfusions is rare, but hemolytic reactions should be monitored during all blood transfusions. These other factors are sometimes used to establish or reject the possibility of familial relationships, such as in cases of disputed fatherhood.