a. Transfer the patient from the delivery table.
Remove the drapes and soiled linen. Remove both legs from the stirrups at the same time and then lower both legs down at the same time to prevent cramping. Assist the patient to move from the table to the bed.
b. Provide care of the perineum.
An ice pack may be applied to the perineum to reduce swelling from episiotomy especially if a fourth degree tear has occurred and to reduce swelling from manual manipulation of the perineum during labor from all the exams. Apply a clean perineal pad between the legs.
c. Transfer the patient to the recovery room.
This will be done after you place a clean gown on the patient, obtained a complete set of vital signs, evaluated the fundal height and firmness, and evaluated the lochia.
d. Ensure emergency equipment is available in the recovery room for possible complications.
(1) Suction and oxygen in case patient becomes eclamptic.
(2) Pitocin® is available in the event of hemorrhage.
(3) IV remains patent for possible use if complications develop.
e. Check the fundus.
(1) Ensure the fundus remains firm.
(2) Massage the fundus until it is firm if the uterus should relax (see figure 2-10).
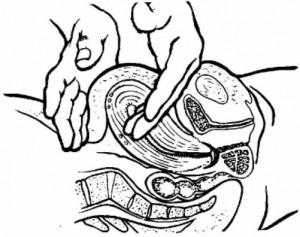
(3) Massage the fundus every 15 minutes during the first hour, every 30 minutes during the next hour, and then, every hour until the patient is ready for transfer.
(4) Chart fundal height. Evaluate from the umbilicus using fingerbreadths. This is recorded as two fingers below the umbilicus (U/2), one finger above the umbilicus (1/U), and so forth. The fundus should remain in the midline. If it deviates from the middle, identify this and evaluate for distended bladder.
(5) Inform the Charge Nurse or physician if the fundus remains boggy after being massaged.
NOTE: A boggy uterus many indicate uterine atony or retained placental fragments. Boggy refers to being inadequately contracted and having a spongy rather than firm feeling. This is descriptive of the postdelivery of the uterus.
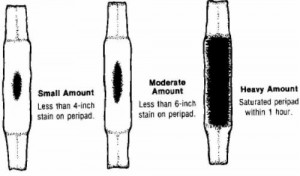
f. Monitor lochia flow. Lochia is the maternal discharge of blood, mucus, and tissue from the uterus.
This may last for several weeks after birth.
(1) Keep a pad count. Record the number of pads soaked with lochia during recovery.
(2) Identify presence of bright red bleeding or blood clots.
(3) Document thick, foul-smelling lochia.
(4) Observe for constant trickle of bright red lochia. This may indicate lacerations.
(5) Identify lochia amounts as small, moderate, or heavy (large) (see figure 2-11).
(6) Document lochia flow when the fundus is massaged.
(a) Every fifteen (15) minutes times one hour.
(b) Every thirty (30) minutes times one hour.
(c) Every hour until ready for transfer.
g. Observe the mother for chills.
The cause of the mother being chilled following birth is unknown. However, it refers primarily to the result of circulatory changes after delivery. The best means of relief is to cover the mother with a warm blanket.
h. Monitor the patient’s vital signs and general condition.
(1) Take BP, P, and R every 15 minutes for an hour, then every 30 minutes for an hour, and then every hour as long as the patient is stable. Take the patient’s temperature every hour.
(2) Observe for uterine atony or hemorrhage.
(3) Observe for any untoward effects from anesthesia.
(4) Orient the patient to the surroundings (bathroom, call bell, lights, etc.).
(5) Allow the patient time to rest.
(6) Encourage the patient to drink fluids.
i. Observe patient’s urinary bladder for distention.
Be able to recognize the difference between a full bladder and a fundus.
(1) Characteristics of a full bladder.
(a) Bulging of the lower abdomen (see figure 2-12).
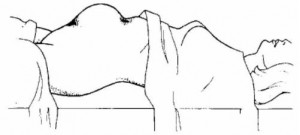
(b) Spongy feeling mass between the fundus and the pubis.
(c) Displaced uterus from the midline, usually to the right.
(d) Increased lochia flow.
(2) Full bladders may actually cause postpartum hemorrhage because it prevents the uterus from contracting appropriately.
(3) Nerve blocks may alter the sensation of a full bladder to the patient and prevent her from urinating.
(4) If at all possible, ambulate the patient to the bathroom.
(5) Urine output less than 300cc on initial void after delivery may suggest urinary retention.
(a) Document the fundal height and bladder status before the patient urinates.
(b) Reevaluate and document the fundal height and bladder status after the patient urinates to accurately document an empty bladder.
j. Evaluate the perineal area for signs of developing edema and/or hematoma.
(1) Predisposing conditions includes prolonged second stage, delivery of a large infant, rapid delivery, forceps delivery, and fourth degree lacerations.
(2) Nursing considerations for perineal edema.
(a) Apply an ice pack to the perineum as soon as possible to decrease the amount of developing edema.
(b) Stress the importance of peri-care and use of “sitz-baths” on the postpartum ward.
(c) Assess for urinary distention which is due to edema of the urethra.
(3) Assessment for perineal hematoma.
(a) Look for discoloration of the perineum.
(b) Listen for the patient’s complaints or expression of severe perineal pain.
(c) Observe for edema of the area.
(d) Observe/listen for patient’s feeling the need to defecate if forming hematoma is creating rectal pressure.
(e) Observe for patient’s sensitivity of the area by touch (by sterile glove).
k. Observe for signs of hemorrhage.
(1) Uterine atony.
(2) Vaginal or cervical lacerations.
(3) Retained placental fragments.
(4) Bladder distention.
(5) Severe hematoma in vagina or surrounding perineum.
l. Assess for ambulatory stability.
(1) The patient is at risk of fainting on initial ambulation after delivery due to hypovolemia from blood loss at delivery and hypoglycemia from prolonged nothing by mouth (NPO) status.
(2) The patient should be accompanied on the first ambulation and observed for stability.
(3) Ammonia ampuls should be readily available.
(4) The patient should be closely monitored while in the bathroom to prevent injury if fainting does occur.
(5) The patient who received regional anesthesia at deliver (that is, pudendal block) should be assessed for possible loss of sensation in the lower extremities.
m. Observe C-section patients.
Most C-section patients are still initially recovered in the recovery room. If not, monitor the patient as you would any patient in a recovery room immediately during post delivery. Include monitoring of the fundus and lochia flow. Times are consistent with the normal vaginal delivery patient.
n. Instruct the patient in the proper perineal care.
The patient should use the peribottle after each void and bowel movement, wipe from front to back to avoid contamination, and apply the perineal pad from front to back.
o. Discontinue IV on a normal patient once she is stable and the physician has ordered removal.
p. Complete notes and transfer the stable patient to the ward (on normal vaginal delivery–others require physician clearance).
