a. Carry out the hospital policy for gowning and the three-minute scrub.
If you are already wearing scrubs, it is not necessary to gown. If the initial scrub has already been completed when coming on duty, a one-minute scrub is acceptable.
b. Receive the infant from the transporter.
Take the infant from the transporter or the transporter’s arms. Verify the ID bracelet on the infant’s arm and leg with the delivery room personnel. Make sure the information is accurate (i.e., mother’s name, sex of the infant, date and time of birth, and doctor’s name). Take the report from the delivery room person. The report concerns pertinent information of the mother’s labor and of the newborn’s birth.
c. Remove the delivery room blanket from the infant.
d. Weigh the infant.
Place a protective paper cover over the scale first and make sure the scale is balanced. Place the infant on the scale. Document the infant’s weight on the:
(1) SF 510, Nursing Notes.
(2) Delivery room record.
(3) Instant data card.
e. Place the infant in an open warmer for the remainder of the admission procedures to maintain adequate temperature.
(1) Measure the infant (see figure 8-5).
(a) Length (from top of head to the heel with the leg fully extended).
(b) Head circumference – repeat after molding and caput succedaneum are resolved.
(c) Chest circumference (at the nipple line).
(d) Abdominal circumference.
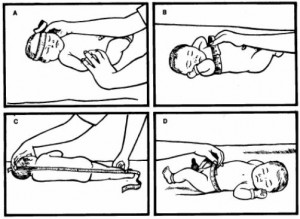
(2) Record measurements in inches and centimeters.
(3) Document the information in the appropriate areas on SF 510, Nursing Notes, the delivery room record, and the instant data card.
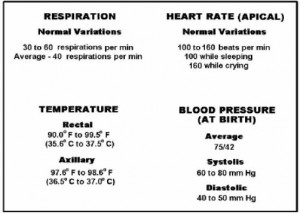
(4) Take infant’s vital signs and document on SF 510, Nursing Notes and the delivery room record.
(a) Temperature-only the first one is done rectally, the remainder are axillary.
(b) Heart rate and respirations-count a full minute because of the irregularities in rhythm.
NOTE: See figure 8-6 for taking the infant’s temperature and figure 8-7 for normal neonatal vital signs.

f. Aspirate fluids.
(1) Aspirate the infant’s mouth and nose gently with a bulb syringe.
(2) Insert a number 5 French catheter into the baby’s nares to check for patency.
(3) Insert a number 8 French catheter in the baby’s mouth down into the stomach and gently aspirate stomach contents.
(4) Record the color and amount of aspirate on SF 510, Nursing Notes and on the delivery record sheet.
g. Evaluate the infant’s physical condition.
(1) Note the infant’s cry, color, and activity for signs of respiratory distress throughout the assessment.
(2) Do a complete head-to-toe assessment, looking for any gross abnormalities on his hands, feet, palate, spine, and so forth.
(3) Document if the infant voids or passes meconium.
(4) Document presence of reflexes (dealt with more extensively in the typical newborn).
(a) Moro.
(b) Sucking.
(c) Grasping.
(5) Count the number of vessels in the cord and document.
(6) Assess head for molding, caput succedaneum, or cephalhematoma and document in appropriate records.
(7) Observe and record any birthmarks.
h. Place the infant on his side (see figure 8-8) to promote drainage of mucus.
Note that he is supported by a pillow to his backside.
i. Provide for infant’s safety while in open warmer.
j. Place the infant in an isolette if his temperature is below 98°F rectally.
If the infant’s temperature is above 98ºF rectally, place him in an open crib.
NOTE: Step “j” is done after the initial assessment and procedures are completed.

