There are several needs of a newborn infant that require close attention.
Establishing and maintaining respirations are the two needs that must be met immediately.
a. Establishing and Maintaining the Newborn’s Airway.
The physician suctions the infant before it is completely born with a bulb syringe or a DeLee trap. A DeLee trap is used if meconium was present in the amniotic fluid. The infant’s mouth is suctioned first and then his nose. Once the infant is delivered, his head is held slightly downward to promote drainage of mucus and fluid. The infant’s face is wiped thoroughly clean.
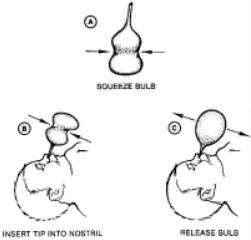
If the infant doesn’t breathe spontaneously, he should be stimulated to cry by slapping his heels, lightly tapping the buttocks, and/or rubbing his back gently. The infant is then positioned with his head slightly down when placed in the radiant warmer. The bulb syringe is used to remove mucus from his mouth and nose (see figure 8-2).
(1) Common characteristics of newborn respirations.
(a) Nose breathers. Sleeps with mouth closed, does not have to interrupt feedings to breathe.
(b) Irregular rate.
(c) Usually abdominal or diaphragmatic in character.
(d) Ranges from 40 to 60 breathers per minute.
(e) Breathing is quiet and shallow.
(f) Easily altered by external stimuli.
(g) Periods of apnea less than 15 seconds is normal.
(h) Acrocyanosis may occur during periods of crying. Acrocyanosis refers to cyanotic look of the baby’s hands and feet when he is crying. When the baby stops crying, his hands and feet get pink again.
(2) Signs and symptoms of newborn respiratory distress.
(a) Increased rate or difficulty breathing-growing and seesaw breathing. In normal respirations, the infant’s chest and abdomen rise. With seesaw respirations, the infant’s chest wall retracts and his abdomen rises with inspirations. See fig. 8-3.
(b) Sternal or subcostal retractions.
(c) Nasal flaring.
(d) Excessive mucus, drooling.
(e) Cyanosis.

b. Maintaining Body Temperature.
(1) Dry the infant thoroughly immediately after delivery. The infant is extremely vulnerable to heat loss because his body surface area is great in relation to his weight and he has relatively little subcutaneous weight. Heat loss after delivery is increased by the cool delivery room and the infant’s wet skin.
(2) Place the infant in a radiant heat warmer.
(3) Place a stockinette cap on the infant’s head to prevent heat loss through the head.
(4) Wrap the infant snugly in a warm blanket.
(5) Place the infant closely to the mother’s skin. Skin-to-skin contact with the mother will help prevent heat loss.
c. Identify the Infant After Delivery.
(1) The infant must be properly identified before leaving the delivery room. An identification (ID) band is placed on the infant’s wrist and leg. An identical band matching the infant’s band is placed on the mother’s wrist.
(2) The infant’s footprints or palm prints placed next to the mother’s thumb print is rarely done in most facilities. Each facility has its own instant identification method.
d. Establish Parent-Infant Bonding Process.
(1) Parent-infant bonding is the initial step in the process of attraction and response between the newborn and the parents. This paves the way for development of love and affiliation that forms a strong family unit.
(2) This process should begin as soon after delivery as possible. In the delivery room as soon as the infant is dry and identified, he should be given to the parents. The infant is more alert during the first hours (approximately four) after birth than in the immediate subsequent hours.
