Goals of modified activity during pregnancy are to promote health of the patient and the fetus, to provide relaxation and diversion, to promote or continue good muscle tone, and to prevent muscle atrophy.
a. Employment.
(1) Many patients continue to work throughout pregnancy. Whether she can or should continue to work depends on the physical activity involved, the industrial hazards, toxic environment (chemical dust particles, gases, such as inhalation anesthesia), medical or obstetrical complications, or employment regulations of the company.
(2) Activities that are dependent on a good sense of balance should be discouraged, especially during the last half of pregnancy.
(3) Excessive fatigue is usually the reason for employment termination. This may be prevented by modification of the job requirements temporarily and adequate rest periods during the day.
(4) Patients who have sedentary jobs need to walk around at intervals and should never sit or stand in one position for long periods. Chairs should provide adequate back support. A footstool can help prevent pressure on veins, relieve strain on varices, and minimize swelling of the feet.
b. Travel. This is perhaps a detail of prenatal care, which most patients think very little about, unless they have a tendency to become nauseated or have had a previous miscarriage, which precludes any extensive strain. Traveling should be discussed with the physician, even though there is little restriction on travel from a medical point of view. Extensive trips should be approved by the physician.
(1) Traveling is not a cause of abortion or premature labor.
(2) Lowered oxygen levels may cause fetal hypoxia in high-altitude regions.
(3) Fatigue or tension are primary problems due to change in personal habits and diets. The patient should take frequent rest periods; stop and walk around every two hours if traveling by auto. Drink plenty of fluids to prevent dehydration. These steps will help prevent fatigue, relieve tension, and increase circulation.
(4) Consider traveling by air for long trips to reduce travel time.
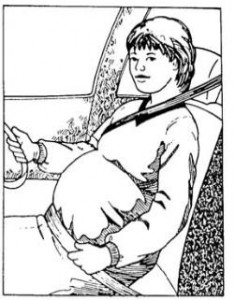
(5) Wear seat belts at all times (see figure 7-1).
c. Sexual Relations.
(1) It has been suggested, but not proven, that premature delivery may be induced by the effect of oxytocin released during maternal response of organs, orgasmic contractions, and prostaglandin in the male ejaculate.
(2) There are no restrictions on sexual intercourse during pregnancy except for those patients who have a history of ruptured membranes, vaginal spotting, or have been treated for preterm labor during this pregnancy.
(3) Patients with a history of repeated abortions may be advised to avoid intercourse during the period of gestation when previous abortions occurred.
(4) Modifications in regard to sexual positions may be required as the pregnancy progresses.
(5) Patients or couples should also be cautioned against masturbatory activities when orgasmic contractions are contraindicated. Studies have shown that orgasm is often more intense when induced by masturbation. The fetal heart rate decreases during orgasm. Fetal distress has not yet been noted.
d. Alcohol Consumption. Studies now support that alcohol should be avoided during pregnancy to prevent the possibility of fetal alcohol syndrome, which includes growth retardation, mental deficiency, and craniofacial or musculoskeletal abnormalities. It is now believed that as little as one to three ounces of alcohol per day may be dangerous.
e. Smoking.
(1) Smoking, or frequent exposure to a smoke-filled environment is harmful to the fetus. Smoking causes vasoconstriction of the blood vessels to include those of the placenta. It also decreases oxygen and nutrients to the infant.
(2) There is direct correlation between smoking and low infant birth weight. There is a tendency toward depressed growth and low weight gain to continue even after birth.
(3) There is an increased number of upper respiratory infections in the infant during the first year of life.
f. Exercise. During pregnancy, exercise is vital for good maternal health, healthy birth, and recovery. Exercise has been proven to be safe and healthful as long as the patient feels comfortable doing them. Physical exercise helps a patient adjust to the hormonal and physical change of pregnancy as well as the emotional and psychological changes. Exercise provides extra support for the growing baby by strengthening abdominal muscles as well as muscles supporting the backbone and the pelvic floor (areas under great stress in pregnancy).
(1) Moderate exercise is recommended. Activities continued to a point of exhaustion or fatigue compromises uterine profusion and fetoplacental oxygenation. These activities are discouraged.
(2) As pregnancy continues, the center of gravity changes so the patient may become clumsy and increase the risk of injury. The amount of exercise is dependent on the health, previous exercise habits, and obstetric history of the individual.
(a) Curtailing an exercise pattern of a previously active patient may be a negative factor in her physical, emotional, and mental health.
(b) Most patients may continue their pre-pregnancy exercise program as long as the pregnancy remains normal.
(3) Once the pregnancy has been confirmed is, however, not the time to start a new exercise program.
Brookside Associates Notes
1. Exercise requiring a fine sense of balance for personal safety are not advised during pregnancy. Balance may not be maintained even in early pregnancy and there is a significant risk of injury from falling.
2. Extreme joint stress (such as might be experienced during intensive weight training) may injure the joints because of the softening of the protective cartilage and tendons that occurs in the second half of pregnancy.
