a. The initial prenatal visit should be scheduled at the first signs of pregnancy.
This is usually shortly after the second menstrual cycle is missed. Depending on where the care is to be given, the first prenatal visit may not be scheduled until after a positive urine pregnancy test is documented.
b. The initial prenatal visit may be particularly stressful to the patient. Some patients may be anxious about the nature of exams and tests to be done during the visit. The pregnancy may have been unplanned, there may be already existing financial or family problems, or some patients may have had unpleasant experiences with previous pregnancies. The presence of one or more of these problems may serve to heighten the emotional content of the visit.
c. Setting a comfortable climate is very important to the patient. The patient’s first impression and initial reception will influence how she may comply with the instructions given during pregnancy. If treated with a true concern as an individual, she will be more inclined to follow instructions. If the patient is rushed with little concern for her as an individual, she may decide not to return. A cordial, respectful environment in which the patient feels like a person is a necessity for every visit.
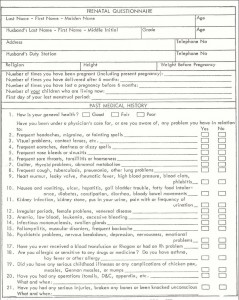
d. A thorough medical/obstetrical history is obtained. The history is essentially a screening tool that identifies the factors that may detrimentally affect the course of pregnancy. This process involves interviewing the patient and possibly having the patient to complete a questionnaire to obtain the following information:
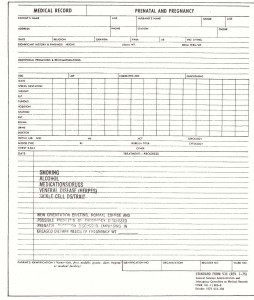
NOTE: See figures 6-1 and 6-2 for a typical prenatal questionnaire and a prenatal and pregnancy medical record.
(1) Past medical history of the patient’s mother and father (for example, hypertension, diabetes, and tuberculosis).
(2) Family illnesses (that is, diabetes, mental illness, and bleeding disorders).

(3) Obstetric/gynecologic record.
(a) Last menstrual period (LMP) and menstrual history (for example, last regular cycle and spotting).
(b) Contraceptive history (Were birth control pills used? Did the patient become pregnant immediately after cessation of pills? How long after cessation of pills?
(c) Reproductive history (for example, number of previous pregnancies and their outcomes, complications).
(d) Exposure or treatment for any sexually transmitted diseases (STDs).
(e) Problems with the current pregnancy (for example, bleeding, nausea, and headaches).
(4) Present medical condition of the patient (for example, hypertension, diabetes, medications presently taking, and any drug allergies).
e. Physical examination. After a complete history is obtained, the patient is prepared for a through physical examination.
(1) Vital signs are taken to include:
(a) Temperature, pulse, respiration, and blood pressure.
(b) Fetal heart tones. Document if obtained with a doppler or fetoscope.
(2) Evaluate height, normal weight, and present weight.
(3) Obtain urine specimen. This should be obtained before the patient undresses for the pelvic examination.
(a) On the initial visit, a complete urinalysis is done.
(b) On subsequent visits, a urine specimen will be dipsticked for albumin and glucose.
(c) Additional testing will be done only if there are indications of toxemia of pregnancy or diabetes mellitus.
(4) Prepare patient for a pelvic examination, if performed.
(a) A pelvic examination is performed to confirm the pregnancy and to determine gestation. An examiner will look for signs of pregnancy–Chadwick’s sign (color of cervix), Goodell’s sign (softening of tip of cervix), and Hegar’s sign (softening of the region between the body of the uterus and cervix). He will also evaluate the size of the uterine and the fundal height.
(b) Estimate of pelvic size. The examiner evaluates the position of the ischial spines and tuberosities. He evaluates diagonal conjugate to estimate pelvic canal size and whether it will allow passage of the fetus at the time of birth.
NOTE: One vaginal birth is not proof of adequate pelvic space for all subsequent deliveries.
(c) Palpation of pelvic contents is done to identify any abnormal masses or tumors.
(d) Nursing responsibilities.
1 Assemble necessary equipment (speculum, lubricant, spatula for cervical scraping, glass slide, culture tube with sterile cotton-tipped applicator, exam gloves, and exam light).
2 Have the patient empty her bladder so she is more comfortable. It is easier for the examiner to evaluate the size of the uterus on an empty bladder.
3 Have the patient to remove her clothing and to put on a patient gown. Allow for patient privacy while changing.
4 Position the patient on the exam table in the lithotomy position with a drape to cover her (see figure 6-3).
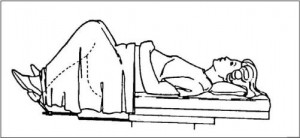
5 Reassure and encourage the patient to relax during the exam. The patient can relax by taking two to three breaths and letting them out slowly through her mouth.
6 Provide wipes so the patient may remove lubricant used during the exam.
7 Allow for patient’s privacy when redressing.
8 Clean up room and dispose of used materials properly.
(5) The physician will observe and palpate the patient’s breast for abnormalities.
(6) A rectal exam is usually done at the end of the pelvic exam.
(7) Laboratory studies performed are as follows:
(a) CBC, Hgb, or Hct-to detect anemia.
(b) Sickle cell on black women-to identify patients with sickle cell anemia.
(c) VDRL-to identify patients with untreated syphilis.
(d) Rh factor, blood type-to determine if the patient is Rh negative.
(e) Rubella antibody titer-to determine immunity to rubella.
(f) Hepatitis screen-is done if patient history indicated cause for suspicion.
Brookside Associates Note
Additional prenatal tests that are commonly performed at or following the initial visit include:
Atypical antibody screen – Maternal atypical antibodies may be capable of causing hemolytic disease of the newborn.
Chlamydia – Chlamydia is a commonly-found microorganism inhabiting the genital tract. A sexually transmitted disease, it can provoke such symptoms as a mucopurulent cervicitis or PID. It can also remain symptomless.
TSH – Used to detect maternal thyroid abnormalities that may effect the fetus.
(g) HTLVIII (AIDS)-screening for AIDS may begin as a common part of the initial visit.
(8) Cultures taken at the time of the pelvic exam are as follows:
(a) Papanicolaou (PAP) Smear is done to detect any abnormalities of cell growth.
(b) Gonorrhea culture is done to screen the patient for possible infection to protect herself, her partner, and the fetus.
(c) Herpes simplex culture is done if there is a history or any lesions noted to rule out active herpes.
