Indications for assessing fetal maturity includes: determining the appropriate time for inducing labor, avoiding prematurity, and guarding the high-risk mother.
Varieties of tests of the fetus status are of value in monitoring the well being of the fetus.
Evaluation of fetal maturity and well-being is essential in the management of the highrisk pregnancy. The following test may be used:
a. Amniocentesis. A method for assessing fetal maturity and well being.
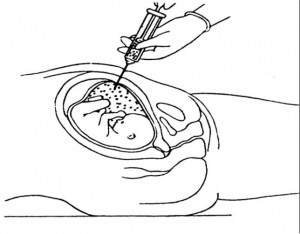
(1) Definition. Amniocentesis is withdrawal of amniotic fluid by insertion of a needle through the abdominal and uterine walls (see figure 2-8).
(2) When done. This procedure is possible after the 14th week of pregnancy when the uterus becomes an abdominal organ and when there is sufficient fluid for the procedure.
(3) Information obtained by amniocentesis.
(a) Color of fluid. The fluid is usually colorless. If it is meconium (stool) stained, it will be greenish brown and this indicates fetal hypoxia.
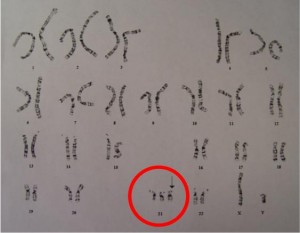
(b) Detects fetal chromosomal anomalies such as Down’s Syndrome.
(c) Helps to evaluate the probability of sex-linked genetic disorders.
(d) Indicates fetal maturity, in-born errors, or metabolism, (indicates disorders like PKU).
(4) Risks of the procedure. Overall complications are less than 1 percent for the mother and the fetus. Possible risks are:
(a) Maternal.
1 Hemorrhage.
2 Infection.
3 Labor.
4 Inadvertent damage to the intestines or bladder.
(b) Fetal.
1 Death.
2 Hemorrhage.
3 Direct injury from the needle.
4 Abortion.
5 Premature labor.
b. Non-Stress Test. It evaluates the ability of the placenta to supply fetal needs in a normal (or unstressed) daily uterine environment.
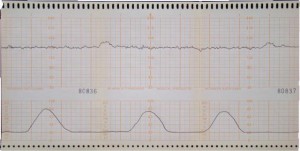
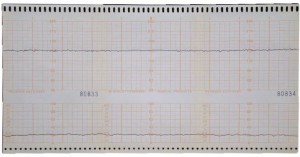
(1) The non-stress test (NST) involves application of the fetal monitor to record the fetal heart rate. The mother is instructed to push a marker button when she feels the fetus move. The marker button indicates movement as it occurred in relationship to the fetal heart rate. With sufficient placental functioning, the fetus should demonstrate an acceleration in heart rate with movement, in the same way that the adult experiences increased heart rate with exercises. A lack of fetal heart rate acceleration indicates the need for further testing.
(2) Non-stress test is used to screen the high-risk pregnancy where the placental compromise is anticipated to include post-term pregnancy, pregnancy induced hypertension, gestational diabetes, intrauterine growth retardation, and maternal complaints of decreased fetal movement.
(3) Patients identified as NST candidates will generally be required to complete an NST on a regular basis (that is, weekly, bi-weekly).
c. Methods of Contraction Production.
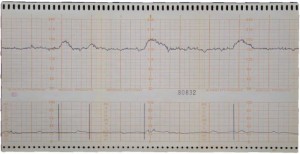
(1) Oxytocin challenge test (OCT). A dilute of IV solution of oxytocin is administered to the mother until a contraction pattern is developed. When sufficient information is obtained to evaluate the test, the medication is turned off.
(a) The Oxytocin challenge test evaluates the ability of the placenta to supply fetal needs in a stressed environment. Contractions, such as those of labor, are a stress on the pregnancy. During a contraction, the flow of oxygen from the uterus to the placenta is diminished. The healthy placenta stores an oxygen reserve so that the fetus does not suffer a diminished supply of oxygen during the contraction.
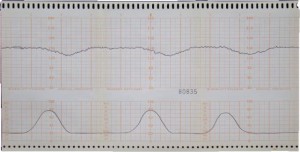
(b) The OCT involves application of the fetal monitor to record fetal heart rate and contraction activity. Acceptable results include acceleration of fetal heart rate or no change in fetal heart rate baseline during a contraction. Unacceptable results include deceleration of fetal heart rate during a contraction.
Illustration of a Negative OCT
(c) The OCT is used to evaluate the high-risk pregnancy where the placental compromise is suspected. It is often applied to the same high-risk patients listed under NST. In addition, it is used to evaluate the patient when a suspicious result is obtained on an NST. The OCT is more invasive than the NST; it provides more conclusive results than the NST.
(2) Breast stimulation test (BST). This test involves stimulation of the nipples (by rubbing), which causes the posterior pituitary to release the hormone oxytocin, which in turn, causes contractions.
(3) Contraction stress test (CST). Evaluation is done in the presence of naturally occurring contractions. It is a means of evaluating the respiratory function (oxygen and carbon dioxide exchange) in the placenta.