Dry the Baby
Immediately after delivery, the baby should be dried. Ideally, this is with a warm, soft towel, but don’t delay in drying the baby while searching for a warm, soft towel.
In an emergency, any dry, absorbing material will work well for this purpose. This would include:
-
Shirts
-
T-shirts
-
Gloves
-
Jackets
-
Socks
Replace the Wet Towels
Babies can lose a tremendous amount of heat very quickly, particularly if they are wet. By removing the wet towels and replacing them with dry towels, you will reduce this heat loss.
Babies, during the first few hours of life, have some difficulty maintaining their body heat and may develop hypothermia if not attended to carefully. This is particularly true of premature infants.
Position the Baby
Babies should be kept on their backs or tilted to the side, but not on their stomachs.
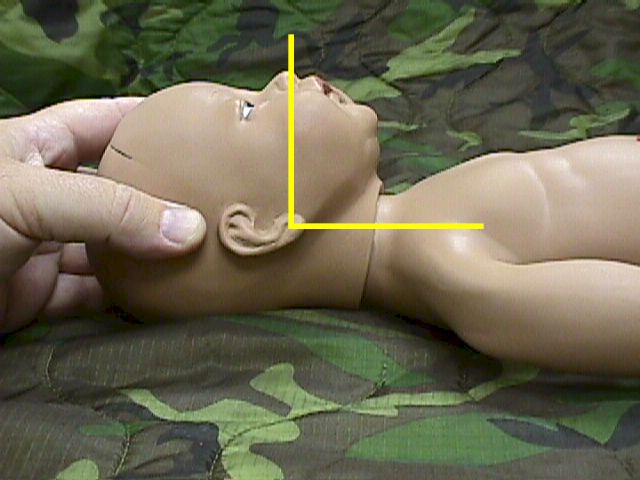
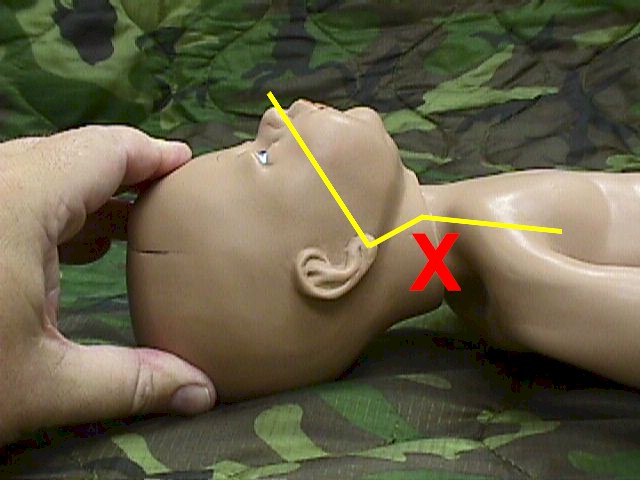
The orientation of the head relative to the body is important for breathing. In adults, this orientation is not usually crucial; adults tolerate a relatively wide range of head positioning without compromising their airway. Not so with newborns who have a relatively narrow range of head positioning that will permit air to move unimpeded through the trachea.
The optimal position for the baby is with the head neither markedly flexed against the chest, nor extended with the chin up in the air. Instead, the head should be in a “military” attitude, looking straight up.
|
OK |
Not OK |
Not OK |
Position the baby on its’ back with the head looking straight up. This will usually provide for good airflow.
If there is any airway obstruction, make small adjustments to the head position to try to straighten the trachea and eliminate the obstruction.
|
|
Suction the Airway
When babies are born, they need to clear the mucous and amniotic fluid from their lungs. Several natural mechanisms help with this:
-
As the fetal chest passes through the birth canal it is compressed, squeezing excess fluid out of the lungs prior to the baby taking its’ first breath. This is noticed most often after the fetal head is delivered but prior to delivery of the shoulders. After several seconds in this “partly delivered” position, fluid can be seen streaming out of the baby’s nose and mouth.
-
After birth, babies cough, sputter and sneeze, mobilizing additional fluid that may be in their lungs.
-
After birth, babies cry loudly and repeatedly, clearing fluid and opening air sacs in the process. Crying is a reassuring event and does not indicate distress.
-
Newborn grunting actions may further mobilize fluid, in addition to opening the air sacs in the lungs.
While babies will, for the most part, bring the amniotic fluid out of the lungs on their own, they may need some assistance in clearing their airway of the mobilized fluid. This will require suctioning.
Bulb syringes are commonly used for this purpose, suctioning both the nose and mouth of the baby. If a bulb syringe is not available, any suction type device may be used, including a hypodermic syringe without the needle.
If no suction device is available, keep the baby in a slight Trendelenburg position (head slightly lower than the feet) and turn the baby to its’ side to allow the fluids to drain out by gravity.
Evaluate the Baby
Evaluate the baby for breathing, color and heart rate. If the baby is not breathing well or is depressed, additional drying with a towel may provide enough tactile stimulation to cause the baby to gasp and recover.
Babies are not slapped on their buttocks for this purpose, although flicking the soles of the feet with a thumb and forefinger can provide enough noxious stimulation.
|
|
Color
Asses the pinkness of the fetal skin.
Although some newborn infants are uniformly pink in color, many have some degree of “acrocyanosis.” This means that the central portion (chest) is pink, but the extremities, particularly the hands and feet, are blue or purple.
Acrocyanosis is normal for a newborn during the first few hours, disappearing over the next day. It is due to relatively sluggish circulation of blood through the peripheral structures, related to immaturity or inexperience of the newborn blood flow regulatory systems.
Central cyanosis is not normal and indicates the need for treatment. It is due to the accumulation of desaturated (oxygen-depleted) hemoglobin.
Cyanosis due to airway obstruction is treated by opening the airway.
Cyanosis due to inadequate ventilations is treated by ventilating the baby.
In mild cases, cyanosis may be resolved by providing 100% oxygen to the baby.
Ventilate if Necessary
If, after a brief period of tactile stimulation, the baby is not making significant respiratory efforts, you should begin artificial ventilation, using whatever materials you have available to you.
In ideal circumstances, this equipment would include a newborn mask, bag, 100% oxygen, pressure gauge, flowmeter and flow control valve.
In other than ideal circumstances, mouth-to-mouth ventilation may be the only available resource.
Position one hand behind the newborn head and neck. This hand will make the small adjustments necessary to keep the airway open.
Cover the newborn’s nose and mouth with your own mouth. Use puffs of air to expand the baby’s lungs. If you blow too forcefully or use too large a volume of air, you risk overexpanding the lungs, causing a pneumothorax.
The normal newborn heart rate is over 100 BPM.
Pediatric stethoscopes can be used to listen to the heartbeat, but palpating the newborn pulse is easy to do and requires no special equipment.
Even if the umbilical cord has been clamped and cut, the umbilical arteries can still be palpated. You will feel a strong tapping sensation if you feel the cord next to the baby with your thumb and forefinger.
Alternatively, you can feel the brachial artery pulse, which courses down the medial aspect of the upper arm.
If the pulse is less than 100 BPM, you should begin ventilating the baby artificially, using whatever equipment and skills that are available.
Keep the Baby Warm
Newborn hypothermia can occur quickly and depress breathing. It is very important to keep the newborn warm. This can be accomplished by covering the baby with clothing as soon as it is dried.
Pay particular attention to keeping the head covered (but the airway open) as heat loss from the newborn head can be substantial.
Typically, the baby is wrapped in warm, soft blankets and a head covering put in place.
In sub-optimal circumstances, nearly any cloth material can be used keep the baby warm.
Non-cloth material can also be effective in keeping the baby warm. Aluminum foil or Mylar reflective blankets provide satisfactory heat retention, particularly if used in air-trapping layers.
If the mother is available, dry the baby, place the baby on the mother’s chest, and cover both of them with blankets or clothing. The mother’s body heat will help keep the baby warm.
Check the baby’s temperature several times during the first few hours of life. The normal range of newborn axillary temperature is about 36.5-37.4C (97.7-99.3F).
|
Apgar Score
|
||||||||||||||||||||||||||||
Assign Apgar Score
The Apgar score is a commonly-used method to assess the newborn status and need for continuing treatment. Points are assigned according to each of five categories. The total score is the sum of the points from each category.
The Apgar score is usually assigned at 1-minute after birth and again at 5-minutes after birth. Scores of 7 or more are considered normal. Those with normal scores may need some assistance and those with very low scores (0, 1 or 2) may need considerable assistance. Most newborn infants with low Apgar scores will be fine, once they are supported and resuscitated.
Breast-feeding
Babies can be breast-fed as soon as the airway is cleared and they are breathing normally. Some babies nurse vigorously while others are not particularly interested in feeding until several hours after birth. It is unwise to try to breast-fed babies with respiratory difficulties until the breathing problems are resolved.
Breast-feeding babies generally make their needs known by crying when they are hungry. They also cry when they are uncomfortable from a wet or soiled diaper. Sometimes, they cry because they need to be picked up and held.
Vernix
Babies are usually born with a white, cheesy coating on their skin called “vernix.” This is a combination of skin secretions and skin cells. While excess vernix can be cleaned from the baby, it is not necessary to remove all of it as it has a protective effect on the baby’s skin.
Meconium
Meconium is the dark green fecal material that babies pass after delivery and sometimes before delivery.
If the amniotic fluid is green colored, this is due to the presence of meconium and is found in as many as one in five deliveries. Babies subjected to intrauterine stress often pass meconium before delivery, but so do many non-stressed fetuses.
The presence of meconium is significant because is indicates the need to thoroughly clear the airway of meconium. In a hospital setting, this is often accomplished with endotracheal visualization or intubation. In operational settings, endotracheal intubation of the newborn may not be an option and careful suctioning with any available device will be performed.
Eye Prophylaxis
Within an hour of birth, treat the newborn’s eyes to prevent gonococcal infection. Alternative medications include:
-
1% silver nitrate solution
-
1% tetracycline opthalmic ointment
- 0.5% erythromycin opthalmic ointment (This also prevents chlamydial infections)
Vitamin K
During the first few hours following delivery, a single injection of 0.5 to 1.0 mg of natural vitamin K can help prevent hemorrhagic disease.
Umbilical Cord Care
Keep the cord stump clean and dry. Daily wiping of the cord with alcohol and leaving it open to the air facilitates drying and discourages bacterial growth. Topical application of antiseptics is usually not necessary unless the baby is living in a highly contaminated area.