Operational Obstetrics & Gynecology
Labor and Delivery
|
Labor consists of regular, frequent, uterine contractions which lead to progressive dilatation of the cervix.
The diagnosis of labor may not be obvious for several reasons:
-
Braxton-Hicks contractions are uterine contractions occurring prior to the onset of labor. They are normal and can be demonstrated with fetal monitoring techniques early in the middle trimester of pregnancy. These innocent contractions can be painful, regular, and frequent, although they usually are not.
-
While the uterine contractions of labor are usually painful, they are sometimes only mildly painful, particularly in the early stages of labor. Occasionally, they are painless.
-
Cervical dilatation alone does not confirm labor, since many women will demonstrate some dilatation (1-3 cm) for weeks or months prior to the onset of true labor.
Thus, in other than obvious circumstances, labor will usually be determined by 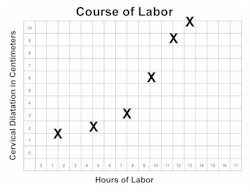 observing the patient over time and demonstrating progressive cervical changes, in the
presence of regular, frequent, painful uterine contractions.
observing the patient over time and demonstrating progressive cervical changes, in the
presence of regular, frequent, painful uterine contractions.
The cause of labor is not known but may include both maternal and fetal factors.
Latent Phase Labor
The first stage of labor is that portion leading up to complete dilatation. The first stage can be divided functionally into two phases: the latent phase and the active phase.
Latent phase labor (also known as prodromal labor) precedes the active phase of labor. Women in latent phase labor:
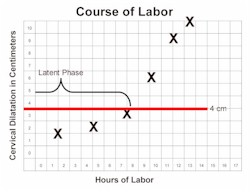
Are less than 4 cm dilated.
-
Have regular, frequent contractions that may or may not be painful.
-
May find their contractions wax and wane
-
Dilate only very slowly
-
Can usually talk or laugh during during their contractions
-
May find this phase of labor lasting days or longer.
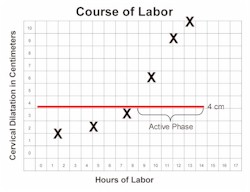 Active Phase Labor
Active Phase Labor
Active phase labor is a time of rapid change in cervical dilatation, effacement, and station.
Active phase labor lasts until the cervix is completely dilated. Women in active phase labor:
-
Are at least 4 cm dilated.
-
Have regular, frequent contractions that are usually moderately painful.
-
Demonstrate progressive cervical dilatation of at least 1.2-1.5 cm per hour.
-
Usually are not comfortable with talking or laughing during their contractions.
For a woman experiencing her first baby, labor usually lasts about 12-14 hours. If she has delivered a baby in the past, labor is generally quicker, lasting about 6-8 hours. These averages are only approximate, and there is considerable variation from one woman to the next, and from one labor to the next.
During labor, the cervix dilates (opens) and effaces (thins). This process has been likened to the process of pulling a turtleneck sweater over your head. The collar opens (dilates) to allow your head to pass through, and also thins (effaces) as your head passes through.
The process of dilatation and effacement occurs for both mechanical reasons and biochemical reasons.
The force of the contracting uterus naturally seeks to dilate and thin the cervix. However, for the cervix to be able to respond to these forces requires it to be "ready." The process of readying the cervix on a cellular level usually takes place over days to weeks preceding the onset of labor.
Descent means that the fetal head descends through the birth canal. The "station" of the fetal head describes how far it has descended through the birth canal.
This station is determined relative to the maternal ischial spines, bony prominences on each side of the maternal pelvic sidewalls.
"0 Station" ("Zero Station") means that the top of the fetal head has descended through the birth canal just to the level of the maternal ischial spines.
This usually means that the fetal head is "fully" engaged (or "completely engaged"), because the widest portion of the fetal head has entered the opening of the birth canal (the pelvic inlet).
If the fetal head has not reached the ischial spines, this is indicated by negative numbers, such as -2 (meaning the top of the fetal head is still 2 cm above the ischial spines).
If the fetal head has descended further than the ischial spines, this is indicated by positive numbers, such as +2 (meaning the top of the head is now 2 cm below the ischial spines).
Negative numbers above -3 indicate the fetal head is unengaged (floating). Positive numbers beyond +3 (such as +4 or +5) indicate that the fetal head is crowning and about to deliver.
Women having their first baby often demonstrate deep engagement (0 or +1) for days to weeks prior to the onset of labor.
Women having their second or third baby may not engage below -2 or -3 until they are in labor, and nearly completely dilated.
Delivery is also known as the second stage of labor. It begins with complete dilatation and ends when the baby is completely out of the mother. The exact time of delivery is normally taken at the moment the baby's anterior shoulder (the shoulder delivering closest to the mother's pubic bone) is out.
As the fetal head passes through the birth canal, it normally demonstrates, in sequence, the "cardinal movements of labor." These include:
-
Engagement (fetal head reaches 0 station.)
-
Descent (fetal head descends past 0 station.)
-
Flexion (head is flexed with the chin to its' chest.)
-
Internal Rotation (head rotates from occiput transverse to occiput anterior.)
-
Extension (head extends with crowning, passing through the vulva.)
-
External Rotation (head returns to its' occiput transverse orientation)
-
Expulsion (shoulders and torso of the baby are delivered.)
As the fetal head descends below 0 station, the mother will perceive a sensation of pressure in the rectal area, similar to the sensation of an imminent bowel movement. At this time she will feel the urge to bear down, holding her breath and performing a Valsalva, to try to expel the baby. This is called "pushing." The maternal pushing efforts assist in speeding the delivery.
For women having their first baby, the second stage will typically take an hour or two.
 Immediately after delivery of the baby, the placenta is still attached inside the
uterus. Some time after delivery, the placenta will detach from the uterus and then be
expelled. This process is called the "3rd stage of labor" and may take just a
few minutes or as long as an hour.
Immediately after delivery of the baby, the placenta is still attached inside the
uterus. Some time after delivery, the placenta will detach from the uterus and then be
expelled. This process is called the "3rd stage of labor" and may take just a
few minutes or as long as an hour.
Signs that the placenta is beginning to separate include:
-
A sudden gush of blood
-
Lengthening of the visible portion of the umbilical cord.
-
The uterus, which is usually soft and flat immediately after delivery, becomes round and firm.
-
The uterus, the top of which is usually about half-way between the pubic bone and the umbilicus, seems to enlarge and approach the umbilicus.
Immediately after the delivery of the baby, uterine contractions stop and labor pains go away. As the placenta separates, the woman will again feel painful uterine cramps. As the placenta descends through the birth canal, she will again feel the urge to bear down and will push out the placenta.
Most labors and deliveries are safe, spontaneous processes, requiring little or no intervention, and result in a healthy mother and healthy baby. Some are not so safe and may not have the same good outcome. The two purposes of L&D management are:
-
Monitoring the mother and baby for abnormalities which, through detection and treatment, will lead to a happy outcome for both.
-
Applying knowledge and skills to improve on the quality of the experience or outcome which nature would otherwise provide. This would include such areas as pain relief, prevention or repair of lacerations, reducing fatigue, anemia, risk of infection, and injury to the mother and baby.
Initial Evaluation of a Woman in Labor
An initial evaluation is performed to:
-
Evaluate the current health status of the mother and baby,
-
Identify risk factors which could influence the course or management of labor, and
-
Determine the labor status of the mother.
Interview the patient as soon as she arrives.
Certain key questions will provide considerable insight into the patient's pregnancy and current status:
-
What brought you in to see me?
-
Are you contracting? When did they start?
-
Are you having any pain?
-
Are you leaking any fluid or blood? When did that begin?
-
Have there been any problems with your pregnancy?
-
Has the baby been moving normally?
-
When did you last eat? What did you have?
-
Are you allergic to any medication?
-
Do you normally take any medication?
-
Have you ever been hospitalized for any reason?
Use a form that covers the prenatal history and risk assessment
For some women, there is a greater chance of problems during labor than for other women. Various factors have been identified to try to predict those women who will experience problems and those who will not. These are called risk factors. Some are more significant than others. While most women with any of these factors will experience good outcomes, they may benefit from increased surveillance or additional resources.
The following are associated with a moderate increase in risk:
|
|
Obtain a set of vital signs from the mother, including BP, pulse and temperature.
-
Elevated BP suggests the presence of pre-eclampsia.
-
Elevated temperature suggests the possible presence of infection.
-
While a pregnant pulse of up to 100 BPM or greater may be normal, rapid pulse may also indicate hypovolemia.
Check the frequency and duration of any uterine contractions.
In some cases, the patient will have been timing the contractions. Placing your hand on the maternal abdomen, you will be able to feel each contraction as the normally soft uterus becomes firm and rises out of the abdomen. Time the contractions from the beginning of one to the beginning of the next one. Also note the duration of the contractions and their relative intensity (mild, mild-to-moderate, moderate, severe)
Record the fetal heart rate.
This can be done with a fetal Doppler device, and electronic fetal monitor, ultrasound visualization of the fetal heart, or a DeLee type stethoscope.
Normal rates are between 120 and 160 BPM at full term. Post term babies may sometimes normally have rates as low as 110 BPM.
Check the urine for protein and glucose.
-
The presence of protein (1+ or greater) can suggest the presence of pre-eclampsia.
-
The presence of glucosuria (1+ to 2+ or greater) can suggest the presence of diabetes.
Estimate the fetal weight. An average baby at full term weighs 7 to 7 1/2 pounds.
By feeling the maternal abdomen, an experienced examiner can often predict within a pound the actual birthweight. A woman who has delivered a baby in the past can often do about as well in predicting her current baby's weight if you ask her, "Is this baby bigger or smaller than your last?"
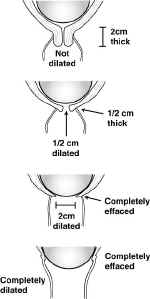
Cervical Dilatation and Effacement
 Using sterile gloves and lubricant, perform a vaginal exam and determine the dilatation
and effacement of the cervix. A small amount of bleeding during the days or hours leading
up to the onset of labor is common and called "bloody show."
Using sterile gloves and lubricant, perform a vaginal exam and determine the dilatation
and effacement of the cervix. A small amount of bleeding during the days or hours leading
up to the onset of labor is common and called "bloody show."
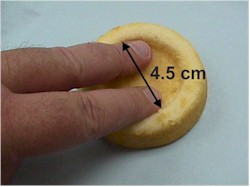
Dilatation is expressed in centimeters. I have relatively large fingers, and for my hands, I make the following generalizations:
-
1.5 cm: One finger fits tightly through the cervix and touches the fetal head.
-
2.0 cm: One finger fits loosely inside the cervix, but I can't fit two fingers in.
-
3.0 cm: Two fingers fit tightly inside the cervix.
-
4.0 cm: Two fingers fit loosely inside the cervix.
-
6.0 cm: There is still 2 cm of cervix still palpable on both sides of the cervix.
-
8.0 cm: There is only 1 cm of cervix still palpable on both sides of the cervix.
-
9.0 cm: Not even 1 cm of cervix is left laterally, or there is only an anterior lip of cervix.
-
10.0 cm: I can't feel any cervix anywhere around the fetal head.
Effacement is easiest to measure in terms of centimeters of thickness, ie., 1 cm thick, 1.5 cm thick, etc. Alternatively, you may express the thickness in percent of an uneffaced cervix...ie, 50%, 90%, etc. This expression presumes a good knowledge of what an uneffaced cervix should feel like.
By abdominal and pelvic examination, determine the orientation of the fetus.
 There are basically 3 alternatives:
There are basically 3 alternatives:
-
Cephalic (head first, or vertex)
-
Breech (butt or feet coming first)
-
Transverse lie (side-to-side orientation, with the fetal head on one side and the butt on the other)
Most of the time, the fetus will be head first (vertex).
 The easiest way for a relatively inexperienced examiner to determine this presentation
is by pelvic exam. The fetal head is hard and bony, while the fetal butt is soft
everywhere except right over the fetal pelvic bones.
The easiest way for a relatively inexperienced examiner to determine this presentation
is by pelvic exam. The fetal head is hard and bony, while the fetal butt is soft
everywhere except right over the fetal pelvic bones.
When the baby is presenting butt first, the presenting part is very soft, but with hard areas within it (sacrum and ischial tuberosities).
If one or both feet are presenting first, you will feel them.
If you don't feel any presenting part (head or butt) on pelvic exam, there is a good chance the baby is in transverse lie (or oblique lie). Then things get a little more complicated.
 Transverse lie or oblique lie can be suspected if the fundal height measurement is less
than expected and if on abdominal exam, the basic orientation of the fetus is
side-to-side.
Transverse lie or oblique lie can be suspected if the fundal height measurement is less
than expected and if on abdominal exam, the basic orientation of the fetus is
side-to-side.
More experienced examiners can tell much from an abdominal exam.
Making a "V" with their thumb and index finger and pressing down just above the pubic bone, they can usually feel the hard fetal head at the pelvic inlet.
Leopolds' maneuvers are used to determine the orientation of the fetus through abdominal palpation.
-
Using two hands and compressing the maternal abdomen, a sense of fetal direction is obtained (vertical or transverse).
-
 The sides of the uterus are palpated to determine the position of the fetal back and
small parts.
The sides of the uterus are palpated to determine the position of the fetal back and
small parts.
-
The presenting part (head or butt) is palpated above the symphysis and degree of engagement determined
-
The fetal occipital prominence is determined.
With a pelvic examination, determine the status of the fetal membranes (intact or ruptured).
A history of a sudden gush of fluid is suggestive, but not convincing evidence of ruptured membranes. Sudden, involuntary loss of urine is a common event in late pregnancy.
 Usually, ruptured membranes are confirmed by a continuing, steady leakage of amniotic
fluid, pooling of clear, Nitrazine positive fluid in the vagina on speculum exam. Vaginal
secretions are normally slightly acid, turning Nitrazine paper yellow. Amniotic fluid, in
contrast, is a weak base, and will turn the Nitrazine paper a dark blue.
Usually, ruptured membranes are confirmed by a continuing, steady leakage of amniotic
fluid, pooling of clear, Nitrazine positive fluid in the vagina on speculum exam. Vaginal
secretions are normally slightly acid, turning Nitrazine paper yellow. Amniotic fluid, in
contrast, is a weak base, and will turn the Nitrazine paper a dark blue.
Dried amniotic fluid forms crystals (ferning) on a microscope slide. Vaginal secretions do not.
Following admission, the hemoglobin or hematocrit may be useful.
Women with significant anemia are more likely to have problems sustaining adequate uterine perfusion during labor. They also have less tolerance for hemorrhage than those with normal blood counts.
Women with no prenatal care should, in addition, have a blood type, Rh factor, and atypical antibody screen performed.
Other tests may be indicated, based on individual histories.
Management of Early Labor
If the patient is in early labor, with a normal pregnancy, and intact membranes, she may feel like ambulating and this is very acceptable.
Not all women in early labor feel like walking and she need not be forced out of bed. Some patients, particularly those with ruptured membranes and those with certain risk factors are probably better off staying in bed, even during early labor.
While in bed, it is preferable, in women without continuous electronic fetal monitoring, to have them lie on one side or the other, but to avoid being on their back. Such lateral positioning maximizes uterine blood flow and provides a greater margin of safety for the baby.
Women with continuous electronic fetal monitoring may choose whatever position is most comfortable. If there is a problem with uterine blood flow, it will be demonstrated on the fetal monitoring strip and appropriate position changes can be undertaken.
Recheck the maternal vital signs every 4 hours. Elevation of blood pressure may indicate the onset of pre-eclampsia. Elevation of temperature >100.4 may indicate the development of infection.
Because of the risk of vomiting and aspirating later in labor, it is best to avoid oral intake other than small sips of clear liquids or ice chips. If labor is lengthy or dehydration becomes an issue, IV fluids are administered. Lactated Ringer's or Lactated Ringer's with 5% Dextrose at 125 cc/hour (6-hours for 1 L) are good choices.
Periodic pelvic exams are performed using sterile gloves and a water-soluble lubricant. The frequency of such exams is determined by individual circumstances, but for a normal patient in active labor, an exam every 2-4 hours is common. In active labor, progress of at least 1 cm per hour is the expected pattern. If the patient feels rectal pressure, an exam is appropriate to see if she is completely dilated.
Some women experience difficulty emptying their bladder during labor. Avoiding overdistension of the bladder during labor will help prevent postpartum urinary retention. If the patient is uncomfortable with bladder pressure and unable to void spontaneously, catheterization will be welcomed.
Prior to active labor, the fetal heart rate for low risk patients is usually evaluated every hour or two.
Once active labor begins for these women (4 cm dilated, with regular, frequent contractions), the fetal heart rate is evaluated every 30 minutes. This can be done by looking at the electronic fetal monitor (if used), or by measuring the fetal heart rate following a contraction. Fetal jeopardy is likely if the auscultated fetal heart rate is less than 100 BPM, even if it later rises back to the normal range of 120-160. Persistent fetal tachycardia (greater than 160 BPM) is also of concern.
For women with significantly increased risks, it is better to evaluate the fetal heart rate every 15 minutes during the active phase of labor.
Women in the second stage of labor (completely dilated but not yet delivered) usually have their fetal heart rate evaluated every 5 minutes until delivery.
Electronic fetal monitors continuously record the instantaneous fetal heart rate on the upper channel and uterine contractions on the lower channel. They do this by attaching, either externally (and non-invasively) or internally, to detect the fetal heart and each uterine contraction.
A normal contraction pattern in active labor shows contractions occurring about every 2-3 minutes and lasting about 60 seconds.
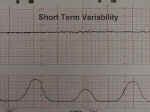 Short Term Variability |
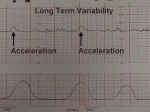 Long Term Variability |
The normal fetal heart rate baseline is 120-160 BPM and has both short and long-term "variability." Short term variability means that from one moment to the next, the fetal heart speeds up slightly and then slows down slightly, usually with a range of 3-5 BPM from the baseline.
Reduced variability occurs normally during fetal sleep and usually returns after 20 to 40 minutes. It also may be present with fetal anomalies or injury. Persistent or progressively reduced variability is not, by itself, a sign of fetal jeopardy. But in combination with other abnormalities (see below), it may indicate fetal intolerance of labor.
Long-term variability represents broad-based swings in fetal heart rate, or "waviness," occurring up to several times a minute. One form of long-term variability of particular significance is a fetal heart "acceleration." These usually occur in response to fetal movement, and are 15 BPM above the baseline or more, lasting 10-20 seconds or longer. They can often be provoked by stimulating the fetal scalp during a pelvic examination, or by acoustically stimulating the fetus with a loud, obnoxious noise. The presence of fetal accelerations is reassuring that the fetus is healthy and tolerating the intrauterine environment well.
During labor, no significance is attached to the absence of fetal accelerations.
Tachycardia is the sustained elevation of fetal heart rate baseline above a 160 BPM. Most tachycardias are not indicative of fetal jeopardy. Causes include:
|
|
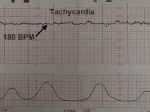 Tachycardia |
 Bradycardia |
 Early Deceleration |
 Variable Deceleration |
 Mild and Severe Variable Decelerations |
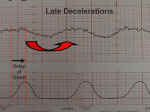 Late Deceleration |
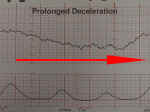 Prolonged Deceleration |
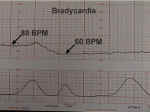
Bradycardia is the sustained depression of fetal heart rate baseline below 120 BPM. Most of these are caused by increased vagal tone, although congenital cardiac abnormalities can also be responsible.
Mild bradycardia (to 80 or 90 BPM) with retention of beat-to-beat variability is common during the second stage of labor and not of great concern so long as delivery occurs relatively soon. Moderate to severe bradycardia (below 80 BPM) with loss of beat-to-beat variability, particularly in association with late decelerations, is more troubling and may indicate fetal distress, requiring prompt resolution.
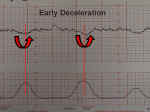
Early decelerations are periodic slowing of the fetal heartbeat, synchronized exactly with the contractions. These dips are rarely more than 20 or 30 BPM below the baseline.
These innocent changes are thought to be due, in many cases, to fetal head compression within the birth canal.
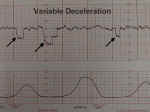
Variable decelerations are variable in onset, duration and depth. They may occur with contractions or between contractions.
Typically, they have an abrupt onset and rapid recovery (in contrast to other types of decelerations which gradually slow and gradually recover.
Variable decelerations are thought to represent a vagal response to some degree of umbilical cord compression. They are not caused by hypoxia, although if severe enough, frequent enough and persistent enough, can ultimately lead to some degree of fetal acidosis.
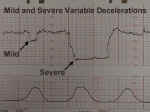
Mild or moderate variable decelerations are common and not considered threatening.
Mild variable decelerations do not dip below 70 BPM and last less than 30 seconds.
Severe variable decelerations dip below 60 BPM for at least 60 seconds ("60 x 60"). If persistent and not correctable by simple means, they can be threatening to fetal well-being.
Late decelerations are repetitive, gradual slowings of the fetal heartbeat toward the end of the contraction cycle. They are felt to represent some degree of utero-placental insufficiency.
If persistent and not correctable, they represent a threat to fetal well-being.
Prolonged decelerations last more than 60 seconds and occur in isolation. Causes include maternal supine hypotension, epidural anesthesia, paracervical block, tetanic contractions, and umbilical cord prolapse.
Some of these are largely self-correcting, such as the deceleration following paracervical block, while others (maternal supine hypotension) respond to simple measures such as repositioning.
Other causes (such as umbilical cord prolapse) require prompt intervention to avoid or reduce the risk of fetal injury.
Various cultures approach the pain of labor differently and individuals vary in their responses to labor pains. Some women will need little or no help with pain relief, while others will benefit from it. While no analgesic is 100% safe 100% of the time, pain relief is generally very safe and provides for a much happier experience for the woman and her family.
The following principles may be helpful:
-
A small number of women in labor will have virtually no pain and they do not need any analgesia.
-
The majority of women will have moderate discomfort, particularly toward the end of labor and they will generally appreciate some analgesia.
-
Some women will experience severe pain during labor and they will benefit from your most intensive efforts.
-
Giving analgesics prior to the onset of active labor (before 4 cm dilatation) will usually slow the labor process, although for some (those with a prolonged latent phase), it may actually speed up labor.
Focused breathing (Lamaze techniques) during contractions can be very helpful in reducing or eliminating the need for pharmacologic analgesia. Hypnotherapy can provide similar relief, as can massage therapy.
Narcotic analgesics can be highly effective at treating the pain of labor. They are generally safe for the baby, although it is better to avoid large doses toward the end of labor in order to avoid respiratory depression in the newborn. The greatest safety with narcotics is achieved when an antagonist (naloxone or Narcan) is available to treat the baby should depression appear. Good dosages for this purpose include:
-
Dilaudid (butorphanol) 1-2 mg IM Q 3-4 hours
-
Dilaudid (butorphanol) 1 mg IM and 1 mg IV every 3-4 hours
-
Demerol (meperidine) 12-25 mg IV every 60-90 minutes
-
Demerol (meperidine) 50-100 mg IM every 3-4 hours
-
Demerol (meperidine) 50 mg plus Vistaril (promethazine) 50 mg IM every 3-4 hours
-
Morphine 2.5-5 mg IV every 60-90 minutes
-
Morphine 7.5 - 15 mg IM every 3-4 hours
More frequent, smaller doses are better than larger, less-frequent doses. Smaller doses given IV are immediately effective, but wear off quickly. Whether that is an advantage or disadvantage depends on how close the woman is to delivery and her need for immediate pain relief.
Paracervical blocks (up to 20 cc of 1% Lidocaine in divided doses) can stop the pain of contractions for up to an hour and a half. Care must be taken to prevent excessive fetal uptake of the Lidocaine, which can lead to fetal bradycardia.
Continuous lumbar epidural anesthetic is effective and versatile, but requires skilled providers. In some settings, this can be very appropriate, but in other operational settings, these resources may not be available.
Inhalation of 50% nitrous oxide with 50% oxygen, can give very effective pain relief during labor and is safe for the mother and baby. It is safest when self-administered by the mother, under the guidance of her birth attendant. If she feels dizzy or starts to achieve anesthetic levels of the nitrous, she will naturally release the mask, reversing the effects of the nitrous oxide.
Less commonly used is a self-administered volatilized gas of methoxyflurane. It is capable of achieving anesthetic levels and so must be very closely monitored.
Second Stage Labor
On reaching complete cervical dilatation, the woman has entered the second stage of labor. The second stage lasts until the delivery of the baby. During the second stage, try to measure the fetal heart rate every 5 minutes.
During the second stage of labor, the woman will feel the uncontrollable urge to bear down. This Valsalva has the effect of increasing the expulsive forces and speeding the delivery process.
For most women, the most effective way to push is in the semi-recumbent position. With the onset of a contraction, she takes several, rapid, deep breaths. Then she holds her breath and tightens her stomach muscles, as though she were trying to move her bowels. She pushes for 10 seconds, relaxes, takes another breath, and pushes for another 10 seconds. Most women can get three or four pushes into a single contraction. She will usually push more effectively if her knees are pulled back towards her shoulders.
-
Some women find they are not comfortable in the semi-reclining position and they may push while tilted toward one side or the other.
-
Some women prefer to deliver on their side, with one knee drawn up and the other leg straightened (the Sims position).
-
Some women prefer to deliver in the sitting or squatting position.
Duration of the second stage is typically an hour or two for a woman having her first baby. For a woman having a subsequent baby, the second stage is usually shorter, less than an hour.
Ideally, you will have a sterile field (sterile towels, drapes, and equipment), but a clean field is nearly as good. Preparation of the vulva with antiseptic solution, shaving of pubic hairs and evacuating the bowels with an enema is not generally necessary, but might be a good idea in selected operational settings where contamination may be significant. For an uncomplicated delivery, you will need:
-
Latex gloves
-
Two baby blankets (one to initially receive and dry the baby and the other for after the baby is dried).
-
Something to clamp the umbilical cord (2 hemostats, 2 shoestrings, 2 ligatures, 2 parachute cords, etc.).
-
Something to cut the umbilical cord (scissors, scalpel, K-Bar, pocket knife, etc.)
-
Something to suction the baby's nose and mouth (bulb syringe, suction tubing, DeLee Trap, etc.)
-
Something in which to place the placenta (basin, bowel, mess kit, etc.)
-
Something to wipe up and absorb blood from the field (4x4 gauze sponges, sanitary pads, towels, small or medium battle dressings, etc.)
-
Injectable Lidocaine (for the delivery or repair of lacerations)
-
Suture (2-0 or 3-0 chromic, plain, or synthetic absorbable) for repair of any lacerations
During the delivery, the fetal head emerges through the vaginal opening, usually facing toward the woman's rectum.
As the fetal head delivers, support the perineum to reduce the risk of perineal laceration from uncontrolled, rapid delivery.
After the fetal head delivers, allow time for the fetal shoulders to rotate and descend through the birth canal. This pause also allows the birth canal to squeeze the fetal chest, forcing amniotic fluid out of the baby's nose and mouth.
After a reasonable pause (15-30 seconds), have the woman bear down again, delivering the shoulders and torso of the baby.
Sometimes, a small incision is made in the perineum to widen the vaginal opening, reduce the risk of laceration, and speed the delivery.
There are two forms, midline and mediolateral.
A midline episiotomy is safe, and avoids major blood vessels and nerves. It heals well and quickly and is reasonably comfortable after delivery.
If the fetal head is still too big to allow for delivery without tearing, the lacerations will likely extend along the line of the episiotomy. Lacerations through the rectal sphincter and into the rectum are relatively common with this type of episiotomy.
A mediolateral episiotomy avoids the problems of tearing into the rectum by directing the forces laterally. However, these episiotomies bleed more, take longer to heal, and are generally more uncomfortable after delivery.
In an operational setting, the major question is not so much where to put the episiotomy, but whether to perform this procedure at all.
-
If you don't perform an episiotomy, you are increasing the risk of vulvar lacerations, but these are usually (not always) small, non-threatening lacerations that will heal well without further complications.
-
If you perform a midline episiotomy, you will have fewer vulvar lacerations, but the few you have are more likely to be the trickier 3rd and 4th degree lacerations involving the anal sphincter and rectum.
-
If you perform a mediolateral episiotomy, you will avoid the 3rd and 4th degree lacerations, but you may open the ischio-rectal fossa to contamination and infection and increase the intrapartum blood loss.
The best approach is an individualized one, that takes into account your own training and expertise, the clinical circumstances, and the operational circumstances.
Although the perineum of a full-term patient is stretchy and compliant, the passage of a baby through the birth canal and vulva is usually uncomfortable. In a hospital setting, anesthesia for the delivery might consist of:
-
Local infiltration
-
Pudendal block
-
Epidural
-
Spinal (saddle block)
-
General anesthetic
In many operational settings, the only available anesthesia for delivery will be local infiltration.
Use 1% Lidocaine and inject just beneath the skin. Don't inject into the deeper tissues because there are no significant numbers of nerves there.
Use 10-20 cc total. The maximum dose of Lidocaine you can give at any one time to avoid Lidocaine toxicity is 50 cc of 1% Lidocaine. Try not to use the whole 50 cc for the delivery as you may need more for the repair of any lacerations.
 Clamp and Cut the Umbilical Cord
Clamp and Cut the Umbilical Cord
After the baby is born, leave the umbilical cord alone until the baby is dried, breathing well and starts to pink up. During this time, keep the baby more or less level with the placenta still inside the mother.
Once the baby is breathing, put two clamps on the umbilical cord, about an inch (3 cm) from the baby's abdomen. Use scissors to cut between the clamps.
 If you don't have clamps and scissors, use anything available to accomplish the same
purpose.
If you don't have clamps and scissors, use anything available to accomplish the same
purpose.
In this example, the radio-opaque threads from a 4 x 4 gauze pad have been removed and used to tie the cord before cutting it with a pocket knife.
Anywhere from a few minutes after delivery to an hour later, the placenta will separate and deliver.
While you are awaiting delivery of the placenta, don't pull on the cord or massage the uterus to try and make it deliver more quickly. Pulling to vigorously on the cord, in the right clinical setting, may lead uterine inversion (the uterus turns inside out), a very serious and dangerous complication.
Massaging the uterus often only causes dis-coordinated contractions which slow a clean shearing of the placenta.
 As the placenta detaches and descends through the birth canal, the woman will again
feel contractions and the urge to bear down. As she does this, the placenta will be
expelled. Make sure all the fetal membranes come out with the placenta.
As the placenta detaches and descends through the birth canal, the woman will again
feel contractions and the urge to bear down. As she does this, the placenta will be
expelled. Make sure all the fetal membranes come out with the placenta.
Inspect the placenta for completeness. If a portion is missing, she will need to have her uterus explored and the missing piece removed.
Also inspect the cord to make sure there are 3 blood vessels present (2 arteries and 1 vein). Two-vessel cords are associated with certain congenital anomalies.
After delivery of the placenta, the uterus normally contracts firmly, closing off the open blood vessels which previously supplied the placenta. Without this contraction, rapid blood loss would likely prove very problematic or worse.
To encourage the uterus to firmly contract, oxytocin 10 mIU IM can be given after delivery. Alternatively, oxytocin 10 or 20 units in a liter of IV fluids can be run briskly (150 cc/hour) into a vein. Breast feeding the baby or providing nipple stimulation (rolling the nipple between thumb and forefinger) will cause the mother's pituitary gland to release oxytocin internally, causing similar, but usually milder effects.
A simple way to encourage firm uterine contraction is with uterine massage. The fundus of the uterus (top portion) is vigorously massaged to keep it the consistency of a tightened thigh muscle. If it is flabby, the patient will likely continue to bleed.
Lochia is the name for vaginal discharge following delivery. For several days, vaginal bleeding will persist, similar to a heavy menstrual period (lochia rubra). Then, it will thin and become more pale in color (lochia serosa). By the 10th day, it will take on a white or yellow appearance due to the admixture of white blood cells (lochia alba). If it has a foul smell at any time, the odor suggests the presence of infection.
Maternal temperature should be periodically assessed. Any persistent fever (>100.4 twice over at least 6 hours) indicates the possibility of infection and should be investigated.
Blood pressure should also be checked several times during the first day and periodically thereafter. Abnormally high blood pressure can indicate late-onset pre-eclampsia. Low blood pressure may indicate hypovolemia.
For the first several days after delivery, the breasts produce a clear, yellow liquid known as colostrum. For nursing mothers, colostrum provides some nutrition and significant antibodies to their babies. Then, the breasts will swell (engorge) with milk, white in color, and containing more calories (fat) and volume. The initial engorgement can be uncomfortable. Nursing relieves this discomfort. For women not breast-feeding, firm support of the breasts and ice packs will help relieve the discomfort, which will disappear within a few days in any event. Nipples should be kept clean and dry.
It is important to establish bladder function early in the post partum phase. Because bladder distention due to post partum bladder atony or urethral obstruction is common, encourage the woman to void early and often. Any evidence of significant urinary retention should be treated with catheterization and prompt resolution is expected. When cleansing the vulva, avoid rectal contamination of the vagina or urethra.
Aftercramps are common, crampy pains originating in the uterus. They are less common among first-time mothers, and more common when nursing. They are annoying but not dangerous and will usually disappear within a few days.
Oral analgesics, such as acetaminophen with codeine, or ibuprofen are appropriate and will ease the pain of vulvar lacerations, aftercramps, and the various muscle aches related to a physically demanding labor and delivery. Rarely will these medications need to be continued beyond the first few days.
Swelling of the hands, ankles and face in the first few days following delivery is common, particularly if IV fluid have been given. In the absence of other indicators of pre-eclampsia (elevated blood pressure and proteinuria), it is of no clinical significance, but may be distressing to the patient. Reassure the patient that this is a normal, expected event and will resolve spontaneously.
Rh negative women who deliver Rh positive babies should receive an injection of Rh immune globulin (Rhogam) to prevent Rh sensitization in later pregnancies. This is best done within 3 days of delivery. In operational settings where the Rh type of the infant is not known, it is safe to give Rhogam to all Rh negative women following delivery. Those with Rh positive babies will benefit and those with Rh negative babies will not be harmed.
After delivery, the mother needs time to rest, sleep, and regain her strength. She may eat whatever appeals to her and can get up and move around whenever she would like. Prolonged bedrest is neither necessary nor desirable. There are a few cautionary notes:
-
While she may be up walking, strenuous physical activity will increase her bleeding and is not a good idea.
-
The first time she gets up, someone should be with her to assist in getting her back down if she feels light-headed.
-
She may shower or bathe freely, but prolonged standing in a hot shower may lead to dizziness, in this setting of borderline hypovolemia and vasodilatation.
After 3 weeks, the uterine lining is normally completely healed and a new endometrium regenerated. At this point, most normal activities can be resumed, although strenuous physical activity is usually restricted until after 6 weeks.
In normal circumstances, women can resume sexual activities whenever they feel like it. Most women won't feel like it for a while, and perineal lacerations generally take 4-6 weeks to completely heal. Even then, intercourse may be uncomfortable, due to residual irritation around any laceration sites, vaginal dryness due to the natural estrogen suppression after delivery, or psychological factors surrounding resumption of intercourse. Patients can be reassured that this is common, temporary, and very much improved with the use of water-soluble lubricants, such as KY Jelly or Surgilube.
Oral contraceptive pills, if desired, can be started any time during the first few days post partum and are compatible with breast feeding. Alternatively, their use may be postponed until the 6-week examination, a common time for follow-up care.
*These videos are an added feature, provided by the Brookside Associates Medical Education Division. They were not present in the original edition.
Contents - Introduction - Medical Support of Women in Field Environments - The Prisoner of War Experience - Routine Care - Pap Smears - Human Papilloma Virus - Contraception - Birth Control Pills - Vulvar Disease - Vaginal Discharge - Abnormal Bleeding - Menstrual Problems - Abdominal Pain - Urination Problems - Menopause - Breast Problems - Sexual Assault - Normal Pregnancy - Abnormal Pregnancy - Normal Labor and Delivery - Problems During Labor and Delivery - Care of the Newborn
|
Bureau of Medicine
and Surgery |
Operational
Obstetrics & Gynecology - 2nd Edition |
This web version of Operational Obstetrics & Gynecology is provided by The Brookside Associates. It contains original contents from the official US Navy NAVMEDPUB 6300-2C, but has been reformatted for web access and includes advertising and links that were not present in the original version. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense. All material in this version is unclassified.
This formatting C. 2006
Brookside Associates, LLC.
All rights reserved