|
|
|||||
Treating a Sucking Chest WoundA sucking chest wound is identified by the sucking or
hissing sound made during breathing by the casualty.
With this type of wound, the chest cavity is no
longer sealed, allowing air to rush through the wound and into the chest
during inhalation. This causes the lung to collapse. This is a
life-threatening condition and requires immediate treatment.
Start by uncovering the wound. If the clothing is
stuck to the wound or in a chemical environment, then clothing should not
be removed. Don't attempt to clean the wound. That will be done later.
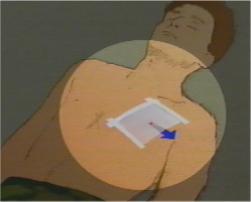
Use the casualty's hand to cover the wound while you quickly prepare an occlusive patch. The plastic wrapper of a battle dressing works very well, although any air-tight material can be substituted, such as:
The patch should be large enough to extend 2 inches beyond the edge of the wound. Smaller patches tend to get pulled back into the wound. Watch a video showing this technique. Secure the patch to the wound with adhesive tape. Three sides should be taped, while the 4th side is left untaped. Whenever the casualty breaths out (exhales), air is expelled from the chest cavity and escapes from underneath the open edge of the patch. Whenever the casualty breaths in (inhales), the patch sticks to the skin and keeps air from returning into the chest cavity. This helps to re-inflate the collapsed lung. Place a small battle dressing over the patch, but
don't make it so tight that the casualty can't breath.
Sometimes, you won't have any adhesive tape, or the
tape won't stick (blood, water, mud, or perspiration may keep it from
sticking). In that case, it is still very helpful to use the patch, held
in place by a battle dressing or triangular bandage.
Finally, roll the patient onto the injured side while
awaiting transportation.
Some medical bags include pre-packaged chest seals. These are easy to use and fast. · Use the enclosed gauze pad to wipe the skin dry around the wound. · Peel off the paper backing and place the sticky side of the seal over the wound and surrounding skin · The one-way flutter valve will allow air to be expelled from the chest, but will keep the outside air from returning. As a first aid measure, patching the chest can be life-saving. To more fully re-inflate the lung, you may need to place a chest tube. Read more about inserting a chest tube,
This section was developed from "Treat an Open (Sucking) Chest Wound," A1701-93-000086, Health Sciences Media Division, US Army Medical Department C&S, Fort Sam Houston, Texas.
Home · Military Medicine · Sick Call · Basic Exams · Medical Procedures · Lab and X-ray · The Pharmacy · The Library · Equipment · Patient Transport · Medical Force Protection · Operational Safety · Operational Settings · Special Operations · Humanitarian Missions · Instructions/Orders · Other Agencies · Video Gallery · Forms · Web Links · Acknowledgements · Help · Feedback Approved for public release; Distribution is unlimited.
*This web version is provided by The Brookside Associates, LLC. It contains original contents from the official US Navy NAVMED P-5139, but has been reformatted for web access and includes advertising and links that were not present in the original version. The medical information presented was reviewed and felt to be accurate in 2001. Medical knowledge and practice methods may have changed since that time. Some links may no longer be active. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the US Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense.
© 2015, Brookside Associates, LLC. All rights reserved |
|
||||