|
|
|||||
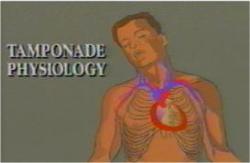
Drain a Cardiac TamponadeCardiac tamponade occurs when the pericardial sac surrounding the heart fills with blood following an injury. Because the sac is relatively rigid and not elastic, even small amounts of blood in the pericardial sac can have important effects on the heart. With increasing amounts of blood in the sac, the heart is compressed and its' ability to fill and pump adequate amounts of blood is impaired. This is called cardiac tamponade and is characterized by:
Pericardiocentesis (withdrawal of fluid or blood from the pericardial sac) can be undertaken in these patients for both diagnosis and treatment. The goals of pericardiocentesis are to:
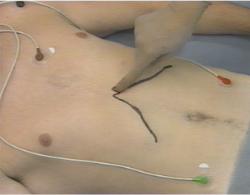
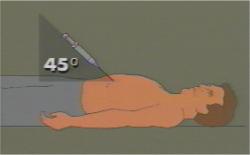
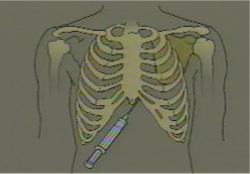
The essential equipment for the procedure is a long needle with an attached catheter, attached to a syringe. A good choice for this is a 14 gauge, 6-inch Angiocath needle. Some IV tubing and a 3-way stopcock are used for continuing drainage once the catheter is placed inside the sac. Continuous EKG monitoring should be employed, if available. In the event of arrythmia provoked by the pericardiocentesis, you would ordinarily want to discontinue the procedure. It is best to perform this technique using the sterile techniques of sterile gloves, antiseptic prep, and surgical draping. If these are unavailable but there is an urgent (life and death) need for pericardiocentesis, proceed, doing the best you can with what you've got. Insert the needle just to the left of the xyphoid process (in the notch between the lower edge of the ribs and the bottom of the breast bone. Aim the needle for the lower tip of the left shoulder blade. Once the needle is through the skin, apply continuous suction with the syringe so that when you enter the pericardial sac, you will know immediately because of the return of blood. As soon as you get significant blood return:
The physical status of the patient will usually improve immediately. Remember that although you have temporarily helped the patient, the injury that lead to the cardiac tamponade is still present, will need repair, and may lead to reaccumulation of blood in the pericardial sac. For these reasons, it is a good idea to leave the soft catheter in place, attached to IV tubing and a 3-way stopcock, so you can easily withdraw more blood if the patient's clinical condition deteriorates. There are numerous potential complications from this procedure, including traumatic injury to the heart, blood vessels or lung, as well as infection. However, in the right patient at the right time, pericardiocentesis can save a life long enough for definitive surgical care to occur. Watch a video demonstrating this technique.
This section was developed from "Emergency Surgical Procedure: Pericardiocentesis" A1701-96-000138, Health Sciences Media Division, US Army Medical Department C&S, Fort Sam Houston, Texas
Home · Military Medicine · Sick Call · Basic Exams · Medical Procedures · Lab and X-ray · The Pharmacy · The Library · Equipment · Patient Transport · Medical Force Protection · Operational Safety · Operational Settings · Special Operations · Humanitarian Missions · Instructions/Orders · Other Agencies · Video Gallery · Forms · Web Links · Acknowledgements · Help · Feedback Approved for public release; Distribution is unlimited.
*This web version is provided by The Brookside Associates, LLC. It contains original contents from the official US Navy NAVMED P-5139, but has been reformatted for web access and includes advertising and links that were not present in the original version. The medical information presented was reviewed and felt to be accurate in 2001. Medical knowledge and practice methods may have changed since that time. Some links may no longer be active. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the US Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense.
© 2015, Brookside Associates, LLC. All rights reserved |
|
||||