Hospital Corpsman Sickcall Screener's Handbook
BUMEDINST 6550:9A
Naval Hospital Great Lakes
1999
Ear, Nose, and Throat
-
Examination of the Ear:
-
External ear (auricle or pinna) — Inspect each ear and surrounding tissue for deformity, lumps or skin lesions. If ear pain, discharge or inflammation is present, move the auricle up and down and press the tragus. Movement of these structures is painful in acute otitis externa, but not in otitis media.
-
Ear Canal and Drum (Tympanic Membrane or TM) — When using the otoscope, grip the auricle firmly while pulling upward, back and slightly out. Using the largest speculum that fits, insert it into the ear, holding the otoscope braced against the patient’s head.
Identify any discharge or foreign bodies, redness or swelling. Cerumen may obscure your view and need removal prior to evaluation of the eardrum. In acute otitis externa, the canal is often swollen, narrowed, moist, pale, tender, and filled with debris.
Inspect the ear drum for color and contour. In acute otitis media, the eardrum is red and bulging. Is the eardrum mobile with valsalva or pneumatic attachment?
Locate Landmarks: Remember — landmarks are obscured with otitis media and acute perforation !
-
Umbo — central bulge where the malleus attaches to the drum.
-
Light reflex — a line of light from the umbo pointing forward and down. Inspect for perforations; the normal drum is translucent, pearly gray color.
-
Handle and short process of the malleus — superior to umbo.
-
Hearing: Whisper a word (like baseball) about one foot away from the ear. If the patient can’t hear the word, he has at least a 30% hearing loss.
-
Examination of the Nose and Sinuses:
-
External Nose:
Inspect for deviations in shape. Observe for discharge from the nares, (watery, mucoid, purulent) From one or both sides. A bilateral watery discharge associated with sneezing and nasal congestion indicate an allergy. Mucus discharge is typical of rhinitis while bilateral purulent (pus) discharge is typical of an upper respiratory infection (URL). One sided purulent, thick greenish and extremely malodorous discharge may indicate a foreign body.
-
Nasal Cavity:
To examine the nasal cavity spread the nares by pushing up on the tip of the nose. Using an otoscope with a wide nasal speculum or a hand held nasal speculum inspect:
-
The nasal mucosa, note color, swelling or discharge (clear, mucus, purulent)
-
Inspect the inferior and middle turnbinates
-
Nasal septum noting any deviation, inflammation or perforation.
-
Inspect for polyps (pale masses that usually hang down from the middle turbinate) or other abnormalities.
-
Examination of the Sinuses:
To palpate the frontal sinus for tenderness use your thumbs and press up from under the bony brow (right under eyebrows). Avoid pressure on the eyes. Then press up on each maxillary sinus by pressing under the zygomatic processes.
Next percuss the sinus areas to detect tenderness. Lightly tap directly of each sinus area with your finger. Another method is to transilluminate the sinuses in a dark room. Place a light under each brow close to the nose. Shield the light with your hand. Normally you will see a dim red glow as light is transmitted through the air filled sinus. Repeat the process with light shinning downward just below the inner aspect of each eye. Look through the open mouth for the reddish glow. Absence of the red glow suggest thickened secretions in the sinus.
-
Examination of the Mouth and Throat (Pharynx):
-
The patient must open mouth widely. With a good light and tongue blade inspect the inner cheeks (Buccal mucosa) for color, ulcers, white patches.
-
Teeth — check for caries or broken teeth.
-
Gums — check for infection, inflammation, swelling or bleeding.
-
Tongue — look at the top, bottom and sides.
-
Throat (Pharynx) — With mouth open ask patient to say "ah" if you can not see the pharynx use a tongue blade. Ask for an "ah" and note the rise of the soft palate ( a test for the 10th, Vagus cranial nerve). Inspect the soft palate, anterior and posterior pillars, uvula, tonsils and posterior pharynx. Note any evidence of exudate, swelling, ulceration or tonsillar enlargement. White patches of exudate associated with redness and swelling suggest acute exudative pharyngitis (strep).
-
|
 |
|
Operational Medicine CD
Text, images,
videos and manuals
The essential text for military healthcare providers
www.brooksidepress.org |
Examination of the Neck:
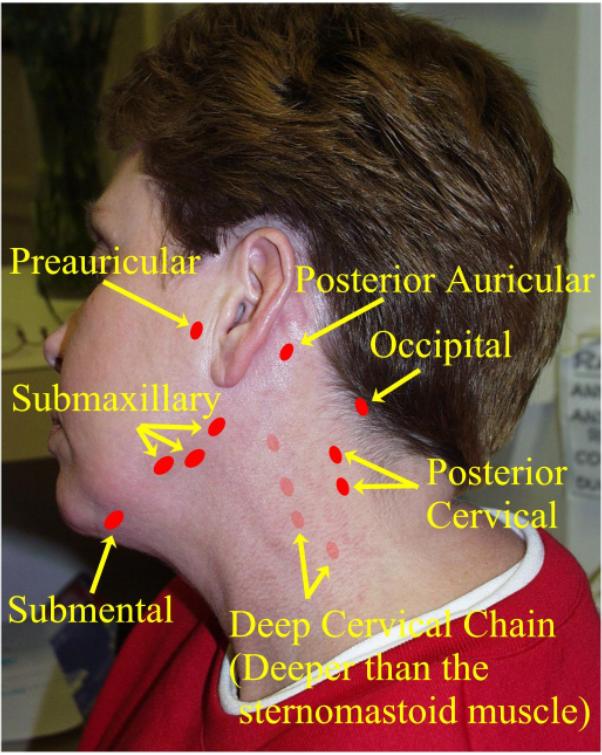
Inspect for masses or asymmetry. Evaluate range of motion and palpate for midline position of the trachea. Inspect and palpate for lymph notes. If a node is enlarged or tender look for a source in the area that it drains. Tender nodes suggest inflammation; hard or fixed nodes suggest malignancy. Is it a node, muscle or artery: Remember you should be able to roll a node in two directions —up and down, and side to side — a muscle or artery will not pass this test.
Check for nuchal rigidity — touch chin to sternum. Pain is a sign of meningeal irritation (see NEUROLOGY LESSON)
Diseases of the Ear, Nose, and Throat
-
External Otitis: (Swimmer’s Ear):
Is there a history of recent water exposure or mechanical trauma (cotton applicator Q-Tip)? External otitis is caused by bacteria that grow in the presence of moisture, but not in an acidic environment. This problem can be prevented with drops made of 2/3 alcohol and 1/3 vinegar that are used after swimming. External otitis is defined as inflammation of the external auditory canal.
S: Pain to the ear may be intense, occasionally a decrease in hearing or a sensation of obstruction in the ear is present.
O: Examination reveals erythema and edema of the ear canal often with purulent exudate. Pain is aggravated by pulling on the auricle or pushing on the tragus. If the canal is very swollen the ear drum may not be visible. The Tragus is usually normal.
A: Otitis Externa
P: Gently remove any debris from the canal so medication may gain entry into it.
Cortisporin Otic Suspension 4-5 gtts qid for 7 days. Tylenol for pain. Occasionally, due to excessive swelling, an otowick must be placed in the canal to get the medication inside. Replace every 24 hours.
-
Sinusitis:
Sinusitis usually follows an URI and occurs when an undrained collection of pus accumulates in a sinus due to viral, allergic or bacterial causes. The maxillary sinus is the most commonly affected with pain and pressure over the cheek. Pain and pressure of the forehead indicate a frontal sinusitis.
S: Bacterial — Mucopurulent nasal discharge, ache behind eyes, toothache like pain, usually worse at night and early morning, and with bending over.
Non-Bacterial (viral) — Clear nasal discharge, post nasal drip with resulting cough, headache, and pressure sensation in sinuses
O: Yellow to green discharge (bacterial) or clear mucuoid discharge (non-bacterial) tenderness over sinuses, may have fever, poor transillumination of sinuses. X-rays may show clouding or air/fluid levels.
A: Sinusitis
P: Antibiotics: Septra DS one BID for 10 days or
Amoxicillin 500 mg TID for 10 days
Ampicillin 500 mg QID for 10 days.
Decongestants: Sudafed 60 mg QID or Entex LA (Duravent) one BID
Nasal decongestant Spray: Afrin
N.S. BID for 3 days.
Tylenol for pain and fever.
-
Acute Pharyngitis / Tonsillitis:
Inflammation of the throat, may or may not have fever, swelling or tender lymph nodes, or purulent exudate. Usually of bacterial or viral etiology.
S: Sore throat, painful swallowing, fever, URI
O: Throat appears red, may have pustular exudate or enlarged tonsils.
Tender lymph nodes may be present.
A: Acute Pharyngitis or Tonsillitis
P: Throat Culture to rule out group A beta-hemolytic strep infection.
Tylenol for pain or fever.
Cepacol Lozenges as needed.
If culture is positive for strep infection treat with:
Bicillin 1.2 million units, IM and /or
Penicillin VK 250 mg QID for 10 days (must take for full 10 days)
Erythromycin 250 mg QID for 10 days.
NOTE: If the examination is highly suspicious for strep infection, i.e. fever, swollen tender nodes, beefy red throat with pustular exudate, then treatment may be started prior to obtaining culture results, just do not skip obtaining the throat culture.
-
Auscutation of lung fields: Abnormal breath sounds of the lungs are of two types:
-
Crackles (old nave was rales) — are intermittent, non-musical, very brief sounds. They sound like rubbing hair between your fingers. Notice if they are heard on inspiration or expiration. These sounds are produced when previously closed airways open suddenly in the smaller airways.
-
Continuous or of longer duration then crackles with a musical sound. There are two types:
-
Wheezes: high pitched musical sound caused by a relatively high velocity air flow through a narrowed airway.
-
Rhonchi: deeper, have a snoring quality, caused by the passage of air through an airway obstructed by secretions. Tend to disappear after coughing.
Now repeat the examination on the anterior chest:
-
Inspect chest
-
Palpation of chest
-
Palpation for tactile fremitus
-
Percussion of anterior thorax
-
Auscultation of anterior chest
|
|
Approved for public release;
Distribution is unlimited.
The listing of any non-Federal product in this CD is not an endorsement of the
product itself, but simply an acknowledgement of the source.
Bureau of Medicine and Surgery
Department of the Navy
2300 E Street NW
Washington, D.C
20372-5300 |
Operational Medicine
Health Care in Military Settings
CAPT Michael John Hughey, MC, USNR
NAVMED P-5139
January 1, 2001 |
United States Special Operations
Command
7701 Tampa Point Blvd.
MacDill AFB, Florida
33621-5323 |
*This web version is provided by
The Brookside Associates Medical Education Division. It contains
original contents from the official US Navy NAVMED P-5139, but has been
reformatted for web access and includes advertising and links that were not
present in the original version. This web version has not been approved by the
Department of the Navy or the Department of Defense. The presence of any
advertising on these pages does not constitute an endorsement of that product or
service by either the US Department of Defense or the Brookside Associates. The
Brookside Associates is a private organization, not affiliated with the United
States Department of Defense.
Contact Us · · Other
Brookside Products
|
|
Operational Medicine 2001
Contents
|

|
 |
|
FMST Student Manual Multimedia CD
30 Operational Medicine Textbooks/Manuals
30 Operational Medicine Videos
"Just in Time" Initial and Refresher Training
Durable Field-Deployable Storage Case |
|