Hospital Corpsman Sickcall Screener's Handbook
Naval Hospital Great Lakes
Cardiovascular Disorder and Exam Techniques
Allotted time:
Instructional references:
-
Brady Emergency Care (7th Edition)
-
American Heart Association Basic Life Support for Health Care Providers
-
Lippincott Manual for Physical Exams
Instructional Aids:
-
Visual aid panel
-
Transparencies Student handout
Terminal learning objectives: Given a simulated patient with simulated symptoms, the
pupil will be able to recognize potential problems and properly perform the needed exam.
Enabling learning objective:
-
Be able to identify the different disorders of the cardiovascular system.
-
Be able to identify the signs and symptoms of different cardiovascular disorders.
-
Be able to identify the treatment of different cardiovascular conditions.
-
Be able to identify the cardiac cycle and the different heart sounds.
-
Be able to identify the different types of murmurs and where they may be heard.
-
Be able to identify the different components of a proper cardiac exam.
-
Be able to identify the different components of the heart and cardiac vascular system.
SIGNS AND SYMPTOMS OF SELECTED CARDIOVASCULAR DISEASES
-
Cardiovascular disease–General Principles
-
Chest pain: refer all chest pain to MO to rule out cardiac involvement. Chest pain has
many causes of which cardiac is only a portion. Chest pain should be evaluated as if the
patient has a potentially fatal illness.
-
Cardiac risk factors
-
smoking
-
diabetes
-
hypercholesterolemia: Excessive amount of cholesterol in the blood.
-
hypertension
-
obesity
-
family HX of MI prior to age 65
-
being male or a post-menopausal woman
-
Common disorders
-
Angina pectoris - lack of O2 to the heart
-
signs/symptoms
-
usually substernal pain
-
usually occurs in association to exertion (sometimes rest)
-
usually subsides with rest
-
Pain can be located in the neck, throat, back, lower jaw, or teeth, axilla, and
epigastrim.
-
Pain will be described as squeezing, crushing, almost vice like. Often a fist is used to
describe the pain (Levine’s sign).The intensity varies from mild to severe.
-
Duration can last anywhere from a few minutes to 5 minutes.
-
Patient may experience palpitations, faintness (but does not faint), diaphoresis,
dyspnea, and symptoms mimicking digestive complaints. May complain of indigestion.
-
Treatment
-
Refer to MO STAT
-
Give basic emergency care and O2 if available.
-
Sublingual nitroglycerin will relieve the pain-must be ordered by MO.
-
If you suspect angina, obtain an EKG, but do not let the EKG delay your notification of
the MO
-
Myocardial infarction (MI) - This is acute death of the heart muscle.
-
Signs/symptoms
-
May be similar to hx of angina
-
Severe to mild squeezing, crushing, substernal pain. Usually worse than angina, but not
always
-
location similar to angina
-
Pain persists, even with rest
-
dyspnea/cyanosis
-
distress secondary to anoxia or pain
-
hypoperfusion (shock)
-
pulmonary edema
-
diaphoretic
-
variable blood pressure
-
variable pulse
-
syncopal symptoms
-
nausea and/or vomiting
-
clammy skin
-
Treatment
-
BLS, o2, emergency
-
Refer to MO or ER STAT
-
Hypertension - involves the elevation of the systolic and/or diastolic blood
pressures.
-
Categories
-
Mild: Diastolic 90-99mm/hg
Systolic 140-159mm/hg
-
Moderate: Diastolic 100-109mm/hg
Systolic 160-179mm/hg
-
Severe: Diastolic 110-119mm/hg
Systolic 180-209mm/hg
-
Very Severe Diastolic > 120mm/hg
Systolic > 219mm/hg
-
Signs/symptoms
-
NONE–MOST COMMON ("the silent killer")
-
headache or fatigue
-
dizziness
-
epsistaxis (nosebleed)
-
shortness of breath
-
visual disturbances
-
chest pain–"ripping"
-
Treatment
-
refer to MO
-
stop smoking
-
stop alcohol
-
relief of stress
-
regular exercise
-
low sodium diet
-
decrease weight
-
medication but depends on severity of HTN (MO to decide)
-
Blood pressure evaluation (BPE’s)
-
Ordered by the MO, this is used only for patients who are found to have a mildly
elevated BP on routine screening. BPE’s are ordered to establish the diagnosis of
HTN.
-
Have patient return for a 5 day blood pressure evaluation which consist of A.M. and
afternoon readings. BP and pulse should be taken lying, sitting, and standing.
-
Each reading should be shown to MO daily.
THE CARDIAC CYCLE
|
 |
|
Operational Medicine CD
Text, images,
videos and manuals
The essential text for military healthcare providers
www.brooksidepress.org |
-
General
-
Ventricular systole is the period of ventricular contraction.
-
Ventricular diastole is the period of ventricular filling.
-
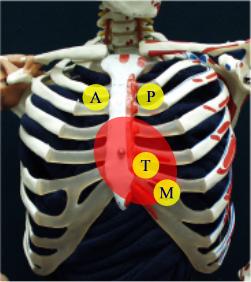
Relation of heart sounds to chest wall.
-
The base of the heart is at the left and right 2nd interspace, close to the sternum.
-
The aortic area is the right 2nd interspace just lateral to the sternal border.
-
The pulmonic area is the left 2nd and 3rd interspace just lateral to the sternal border.
-
The tricuspid area is just lateral to the lower left sternal border.
-
The mitral area is the left 5th interspace just medial to the midclavicular line (MCL).
This is the apex of the heart.
-
The various areas overlap to some extent.
-
Remember "Apartment M" as you march from the upper right chest to left lower
chest A - aortic
P - pulmonic
T - tricuspid
M - mitral
-
Heart sounds
-
S-1
-
closure of mitral and tricuspid valves
-
heard best in mitral area
-
initiation of systole
-
S-2
-
closure of aortic and pulmonic valve
-
heard best in aortic/pulmonic areas
-
initiation of diastole
-
S-3
-
heard in early diastole, after S-2
-
It is pathologic. Seen in conditions of volume overload or cardiac failure.
-
S-4
-
heard just before S-1
-
Is due to increased ventricular resistance with ventricular filling during atrial
contraction.
-
Is associated with hypertensive disease and aortic stenosis but may sometimes be normal
in young healthy people and pregnant women.
-
S-2 splitting
-
During inspiration S-2 splits into two heart sounds, A-2 and P-2 (S2=A2+P2).
-
The pulmonary component (P-2) is heard best in the 2nd and 3rd interspaces close to the
sternum. It comes before A-2.
-
Aortic component (A-2) is louder and is heard well over the entire pericardium.
-
The splitting of S2 into A2 and P2 is a normal finding.
-
Murmurs
-
Definition: Auditory vibrations resulting from turbulence of blood flow, through
narrowed valves (stenosis), backwards flow (regurgitation), or abnormal passages (shunts).
Typically a whooshing quality of sound.
-
Parameters in assessment of murmurs.
-
intensity (loudness)
-
Pitch
-
configuration (shape) (i.e., creshendo, diamond-shaped)
-
quality
-
duration
-
radiation
-
timing in cycle
-
Categories of murmurs
-
systolic: best classified by time of onset and termination. May be functional or
innocent.
-
pan systolic - starts with S-1 and ends with S-2 without a gap between murmur and heart
sounds.
-
mid-systolic - begins after S-1 and ends at or before S-2.
-
late systolic - begin in mid to late systolic and ends with S-2.
-
diastolic: classified by time of onset and termination. ALWAYS PATHOLOGIC.
-
early - begins with S-2
-
mid - begins at clear intervals after S-2
-
late diastolic - begin in mid to late diastole and ends with S-1
Cardiac Cycle:
-
Other types
-
Some specific murmurs are identified by area of auscultation, parameters, and time of
cycle.
-
Aortic stenosis
-
2nd right interspace
-
radiation to neck and down left sternal border
-
often loud and with a thrill
-
medium pitch
-
harsh quality
-
heard best with pt sitting and leaning forward
-
Pulmonic stenosis
-
2nd and 3rd left interspace
-
radiation to left shoulder and neck
-
soft to loud, may have a thrill
-
medium pitch
-
harsh quality
-
Pansystolic murmurs
-
Mitral regurgitation
-
located in apex
-
radiation to left axilla
-
soft to loud with possible apical thrill
-
medium to high pitch
-
blowing quality
-
doesn’t get louder with inspiration
-
Tricuspid regurgitation
-
lower left sternal border
-
radiation to right sternum to xiphoid area or midclavicular line. Never to axilla.
-
variable intensity
-
medium pitch
-
blowing quality
-
gets louder with inspiration
-
Diastolic murmurs
-
Aortic regurgitation
-
2nd and 4th left interspaces
-
grade 1 to 3
-
high pitch - use diaphragm of stethoscope
-
blowing quality
-
Heard best with patient sitting and leaning forward and with breath held in expiration.
-
Mitral stenosis
-
limited to apex
-
no radiation
-
grade 1 to 4
-
low pitch - use bell of stethoscope
-
listen at apical impulses with patient in left lateral position
-
SBE (subacute bacterial endocarditis): often develops on abnormal valves after
asymptomatic bacteremias from infected gums, or GU or GI tract.
-
It is recommended that antimicrobial prophylaxis be performed for patients with valvular
or other predispositions to infectious endocarditis when undergoing procedures associated
with bacteremias and subsquent infectious endocarditis. Examples of these procedures are:
-
oral-dental procedures, to include cleanings, tonsillectomy, or adenoidectomy (viradans
streptococci)
-
GI/GU tract infections (enterococci)
-
cardiac valvular surgery (Staphylococcus aureus & epidermidis)
-
Prophylaxis regimen
-
Amoxicillin 3.0 gm PO 1 hr before procedure, then 1.5 gm PO 6 hrs later
-
PCN allergic: E-mycin 1.0 gm PO 2 hrs before procedure, then 1/2 dose (0.5 gm) 6 hrs
later
-
Techniques of examination
-
Position
-
Have patient lying with upper body elevated at 30 degrees.
-
Stand on patients right side.
-
Use a quiet room for examination.
-
Inspection and palpation
-
Observe for abnormal pulsation.
-
Palpate with the ball of your hand for thrills/pulsations.
-
aortic area - pulsation of aortic aneurysm or thrill of aortic stenosis, accented on
closure.
-
2nd left interspace pulsation of increased pulmonary artery pressure. Felt during held
expiration.
-
right ventricular area - left sternal border in 3rd, 4th, and 5th interspaces for right
ventricular impulse.
-
apical or left ventricular area - feel for apical impulse, usually at 5th interspace
just medial to left MCL.
-
note position, duration, intensity and amplitude.
-
may be laterally displaced in left ventricular enlargement
-
normally light tapping 1-2 cm diameter area
-
Auscultation
-
To listen for the heart sounds, start in the right 2nd interspace, left 2nd interspace
then the 3rd, 4th, and 5th interspaces and finally to the apex. (APT-M)
-
Identify S-1, S-2 (begin in aortic/pulmonic area)
-
S-1 is the first paired heart sounds
-
S-2 normally louder in aortic area
-
S-1 immediately precedes carotid impulse
-
Identify heart rate
-
Determine number of beats per minute
-
bradycardia (slow heart rate) below 60 bts/min
-
tachycardia (fast heart rate) above 100 bts/min
-
Identify rhythm
-
regular or irregular [regularly irregular (PVC’s)] or [ irregularly irregular
(atrial fibrillation)]
-
additional or premature beats on regular pattern (regularly irregular) vs no
identifiable rhythm (complete irregularity or irregularly irregular)
-
rhythm varies normally with respirations
-
Listen for extra heart sounds (S-3, S-4 murmurs or rubs)
-
Grade intensity of murmurs if present
-
grade 1 - very faint, hard to hear
-
grade 2 - quiet but heard easily with stethoscope
-
grade 3 - moderately loud
-
grade 4 - loud murmurstill need stethoscope to hear, associated with thrill
-
grade 5 - very loud, heard with stethoscope partially placed on the chest, associated
with thrill
-
grade 6 - heard with stethoscope entirely off of the chest
-
Carotid arteries/Jugular venous pressure and pulses
-
Carotid arteries
-
Palpate carotid pulsation just lateral to thyroid cartilage of trachea.
-
Palpate amplitude and contour of pulsation of aortic regurgitation, lifts or bounding
pulse.
-
Auscultate with the bell of the stethoscope while patient holds breath. This is done to
access for carotid bruits which may suggest carotid artery narrowing.
-
Jugular venous pressure
-
Observe neck for venous distention
-
Position patient with head elevated to 30 degrees
-
Identify external jugular vein.
-
Identify highest point which pulsation may be seen.
-
Estimated venous pressure from horizontal from top of pulsation to a plumb line dropped
perpendicular to the top of the sternal angle. More than 3-4cm venous pressure is
abnormal.
Hospital Corpsman Sickcall Screeners Handbook
Naval Hospital, Great Lakes
Introduction
April, 1999
|