This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
Lesson 8: Care of the Normal Newborn Infant
The practical nurse has a unique opportunity of closely observing and providing care for the newborn infant after delivery (see figure 8-1). Because of the newborn infant's helplessness, his needs must be met initially by nursing personnel. Many nursing assessments and evaluations are conducted for the well-being of the infant. Nursing care does not stop with the newborn infant. Interaction with the parents is also important in the development of a family unit.
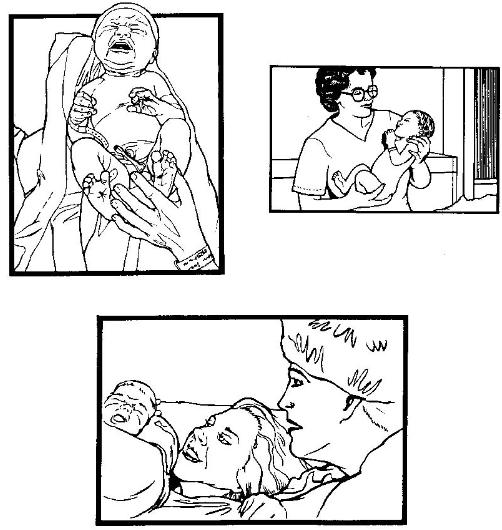
Figure 8-1. The newborn infant.
8-2. CARE OF THE NEWBORN IN THE DELIVERY ROOM
There are several needs of a newborn infant that require close attention. Establishing and maintaining respirations are the two needs that must be met immediately.
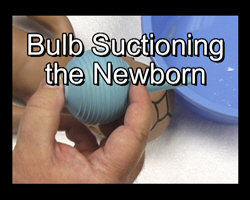
a. Establishing and Maintaining the Newborn's Airway. The physician suctions the infant before it is completely born with a bulb syringe or a DeLee trap. A DeLee trap is used if meconium was present in the amniotic fluid. The infant's mouth is suctioned first and then his nose. Once the infant is delivered, his head is held slightly downward to promote drainage of mucus and fluid. The infant's face is wiped thoroughly clean. If the infant doesn't breathe spontaneously, he should be stimulated to cry by slapping his heels, lightly tapping the buttocks, and/or rubbing his back gently. The infant is then positioned with his head slightly down when placed in the radiant warmer. The bulb syringe is used to remove mucus from his mouth and nose (see figure 8-2).
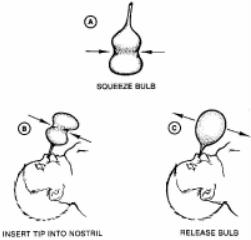 Figure 8-2. Removing mucus from infant's nose. |
|
(1) Common characteristics of newborn respirations.
(a) Nose breathers. Sleeps with mouth closed, does not have to interrupt feedings to breathe.
(b) Irregular rate.
(c) Usually abdominal or diaphragmatic in character.
(d) Ranges from 40 to 60 breathers per minute.
(e) Breathing is quiet and shallow.
(f) Easily altered by external stimuli.
(g) Periods of apnea less than 15 seconds is normal.
(h) Acrocyanosis may occur during periods of crying. Acrocyanosis refers to cyanotic look of the baby's hands and feet when he is crying. When the baby stops crying, his hands and feet get pink again.
(2) Signs and symptoms of newborn respiratory distress.
(a) Increased rate or difficulty breathing-growing and seesaw breathing. In normal respirations, the infant's chest and abdomen rise. With seesaw respirations, the infant's chest wall retracts and his abdomen rises with inspirations. See fig. 8-3.
(b) Sternal or subcostal retractions.
(c) Nasal flaring.
(d) Excessive mucus, drooling.
(e) Cyanosis.

Figure 8-3. See-saw respirations.
b. Maintaining Body Temperature.
(1) Dry the infant thoroughly immediately after delivery. The infant is extremely vulnerable to heat loss because his body surface area is great in relation to his weight and he has relatively little subcutaneous weight. Heat loss after delivery is increased by the cool delivery room and the infant's wet skin.
(2) Place the infant in a radiant heat warmer.
(3) Place a stockinette cap on the infant's head to prevent heat loss through the head.
(4) Wrap the infant snugly in a warm blanket.
(5) Place the infant closely to the mother's skin. Skin-to-skin contact with the mother will help prevent heat loss.
c. Identify the Infant After Delivery.
(1) The infant must be properly identified before leaving the delivery room. An identification (ID) band is placed on the infant's wrist and leg. An identical band matching the infant's band is placed on the mother's wrist.
(2) The infant's footprints or palm prints placed next to the mother's thumb print is rarely done in most facilities. Each facility has its own instant identification method.
d. Establish Parent-Infant Bonding Process.
(1) Parent-infant bonding is the initial step in the process of attraction and response between the newborn and the parents. This paves the way for development of love and affiliation that forms a strong family unit.
(2) This process should begin as soon after delivery as possible. In the delivery room as soon as the infant is dry and identified, he should be given to the parents. The infant is more alert during the first hours (approximately four) after birth than in the immediate subsequent hours.
8-3. VIRGINIA APGAR SCORING OF THE NEWBORN
The initial APGAR scoring is performed in the delivery room by the physician. APGAR scoring is a method of evaluating the condition of the newborn at one minute and at five minutes after delivery. See figure 8-4 for an APGAR scoring chart.
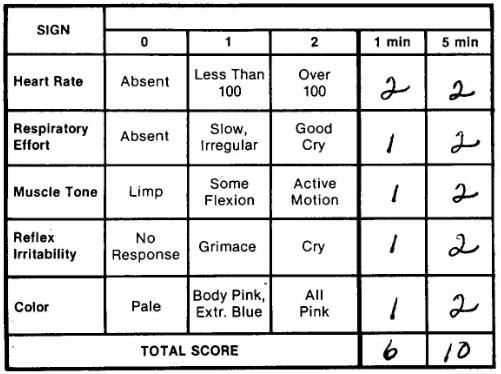
Figure 8-4. APGAR scoring chart.
a. Purpose. The APGAR scoring chart is used to evaluate the conditions of the baby at birth, determine the need for resuscitation, evaluate the effectiveness of resuscitative efforts, and to identify neonates at risk for morbidity and mortality.
b. Objective Signs Used for Evaluation.
(1) Heart rate.
(2) Respiratory effort.
(3) Muscle tone.
(4) Reflex irritability.
(5) Color.
c. Scoring.
(1) Evaluations at each of the five categories are initially done at one minute after birth.
(2) Each item has a maximum score of two and a minimum score of zero.
(3) The final APGAR score is the sum total of the five items, with a maximum score of ten. The higher the final APGAR score, the better condition of the infant.
(4) Evaluations at one minute quickly indicate the neonate's initial adaptation to extrauterine life and whether or not resuscitation is necessary.
(5) The five-minute score gives a more accurate picture of the neonate's overall status, including obvious neurologic impairment or impending death.
8-4. PROCEDURE FOR ADMISSION TO THE NURSERY
a. Carry out the hospital policy for gowning and the three-minute scrub. If you are already wearing scrubs, it is not necessary to gown. If the initial scrub has already been completed when coming on duty, a one-minute scrub is acceptable.
b. Receive the infant from the transporter. Take the infant from the transporter or the transporter's arms. Verify the ID bracelet on the infant's arm and leg with the delivery room personnel. Make sure the information is accurate (i.e., mother's name, sex of the infant, date and time of birth, and doctor's name). Take the report from the delivery room person. The report concerns pertinent information of the mother's labor and of the newborn's birth.
c. Remove the delivery room blanket from the infant.
d. Weigh the infant. Place a protective paper cover over the scale first and make sure the scale is balanced. Place the infant on the scale. Document the infant's weight on the:
(2) Delivery room record.
(3) Instant data card.
e. Place the infant in an open warmer for the remainder of the admission procedures to maintain adequate temperature.
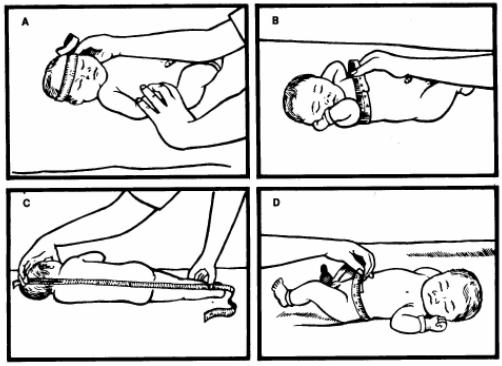
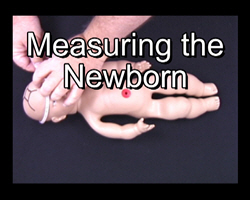
(1) Measure the infant (see figure 8-5).
(a) Length (from top of head to the heel with the leg fully extended).
(b) Head circumference - repeat after molding and caput succedaneum are resolved.
(c) Chest circumference (at the nipple line).
(d) Abdominal circumference.
(2) Record measurements in inches and centimeters.
(3) Document the information in the appropriate areas on SF 510, Nursing Notes, the delivery room record, and the instant data card.
(4) Take infant's vital signs and document on SF 510, Nursing Notes and the delivery room record.
(a) Temperature-only the first one is done rectally, the remainder are axillary.
(b) Heart rate and respirations-count a full minute because of the irregularities in rhythm.
NOTE: See figure 8-6 for taking the infant's temperature and figure 8-7 for normal neonatal vital signs.
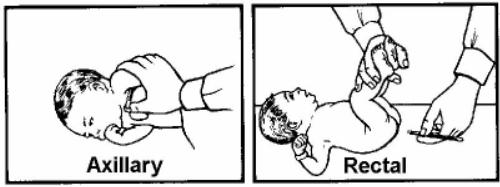
Figure 8-6. Taking infant's temperature.
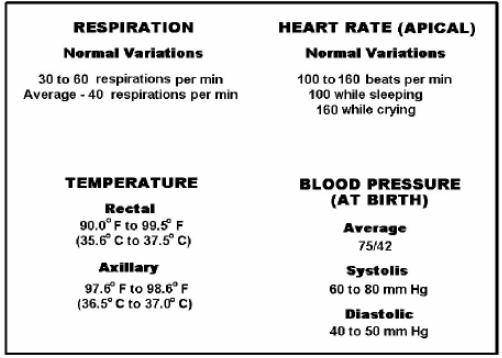
Figure 8-7. Normal neonatal vital signs.
f. Aspirate fluids.
(1) Aspirate the infant's mouth and nose gently with a bulb syringe.
(2) Insert a number 5 French catheter into the baby's nares to check for patency.
(3) Insert a number 8 French catheter in the baby's mouth down into the stomach and gently aspirate stomach contents.
(4) Record the color and amount of aspirate on SF 510, Nursing Notes and on the delivery record sheet.
g. Evaluate the infant's physical condition.
(1) Note the infant's cry, color, and activity for signs of respiratory distress throughout the assessment.
(2) Do a complete head-to-toe assessment, looking for any gross abnormalities on his hands, feet, palate, spine, and so forth.
(3) Document if the infant voids or passes meconium.
(4) Document presence of reflexes (dealt with more extensively in the typical newborn).
(a) Moro.
(b) Sucking.
(c) Grasping.
(5) Count the number of vessels in the cord and document.
(6) Assess head for molding, caput succedaneum, or cephalhematoma and document in appropriate records.
(7) Observe and record any birthmarks.
h. Place the infant on his side (see figure 8-8) to promote drainage of mucus. Note that he is supported by a pillow to his backside.

Figure 8-8. Infant placed on his side.
i. Provide for infant's safety while in open warmer.
j. Place the infant in an isolette if his temperature is below 98°F rectally. If the infant's temperature is above 98ºF rectally, place him in an open crib.
NOTE: Step "j" is done after the initial assessment and procedures are completed.
8-5. ADMINISTRATION OF VITAMIN K
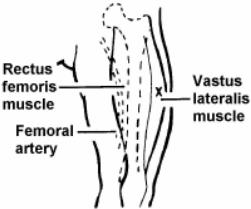
Vitamin K is given as a prophylaxis for hemorrhagic disease. It is administered intramuscular (IM) in the vastus lateralis muscle (see figure 8-9).
8-6. EYE PROPHYLAXIS FOR THE NEWBORN
This procedure is required by law in all states as prophylaxis against gonorrhea. The medications used are as follows:
a. Erythromycin Ophthalmic Ointment. This has become the drug of choice and is received in a sterile syringe from the pharmacy. It is injected into each eye from the inner to outer canthus immediately after birth (see figure 8-10). It does not appear to cause much eye irritation.
b. 1% Silver Nitrate Solution. Two drops are applied in each eye in the conjunctival sac, not the cornea. The infant eyes may or may not be irrigated after instillation, depending on local policy. The infant may get profuse discharge and chemical conjunctivitis for a few days with no residual damage. One percent silver nitrate solution is no longer recommended for use.
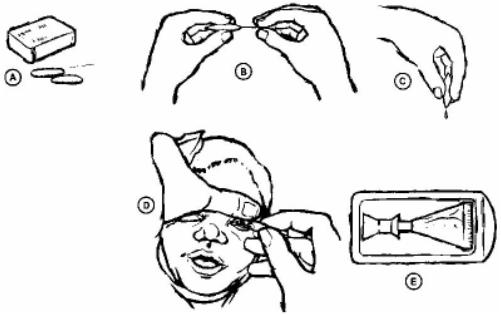
Figure 8-10. Administration of erythromycin ophthalmic ointment.
a. The amount of time required for the initial bath is determined by local policy. If the infant's temperature is greater than 98ºF rectally, the bath may be done after all admission procedures are done. Otherwise, wait until the infant's temperature has stabilized above 98ºF.
b. The procedure for actually completing the bath is also determined by local policy. Allow the parent to participate if possible. Remove as much of the vernix as possible. Some may not come off during the first bath because it is so "sticky."
8-8. CORD CARE FOR THE NEWBORN INFANT
a. Inspect the cord frequently for signs of bleeding immediately after it has been cut.
b. Apply triple dye (refer to local policy) to the cord after the infant has had his bath and has been determined to be stable. The dye prevents infection and helps the cord to dry.
c. Swab the cord with alcohol at least three times per day (refer to local policy). The alcohol aids in drying.
d. Observe for cord detachment. The cord detaches in ten to fourteen days. The cord dries faster when left uncovered. Have the parents roll the infant's diaper down some in front initially so the cord is not covered.
e. Observe for signs of infection and report findings immediately. The signs of infection are purulent drainage, redness, and possible swelling (more than usual).
a. Bonding should be initiated in the delivery room.
b. The significant other should be allowed to participate in as much of the care as possible during the admission process to develop the bond between him and the infant.
c. Transport the infant back to the mother as soon as local policy allows to take advantage of the alert state newborns have during those first few hours after birth.
(1) This is considered a critical time for both individuals to interact and get to know one another.
(2) It is an excellent time to establish breast-feeding while the infant is awake.
(3) Approximately the first four hours after delivery, the infant returns to a sleep state or less alert state.
a. Baptism is performed for infants who are in imminent danger of death and whose parents are Roman Catholic or certain other Christian denominations.
b. The nurse may perform the baptism by pouring a small amount of warmed water on the infant's head and saying, "I baptize thee in the name of the Father, and of the Son, and of the Holy Spirit." A record of the baptism is made in SF 510, Nursing Notes. The parents are notified about the baptism.
8-11. COMPLETE INSPECTION OF THE NEWBORN
A complete inspection of the newborn infant is performed within 24 hours after delivery. The goal is to compile a complete record of the newborn that will act as a database for subsequent assessment and care.
|
a. Assemble necessary equipment.
(1) Pediatric stethoscope.
(2) Penlight.
(3) Tape measure.
(4) Rectal thermometer.
(5) Infant scale.
b. Wash hands for a full three minutes.
c. Approach and identify the infant.
d. Provide for a warm, well-lighted, draft-free area, keeping the infant undressed for as short a time as possible.
e. Place the infant on a flat, protected surface.
f. Take the infant's temperature. The infant's temperature is taken rectally only on admission. Subsequent temperatures are to be taken by the axillary method.
g. Determine the infant's apical heart rate. Count for a full minute.
h. Determine the infant's respiratory rate. Count for a full minute. Note any signs of respiratory distress (retractions, grunting, nasal flaring) rate over 60 bpm, or periods of apnea. Auscultate the infant's lungs.
i. Balance the scale.
j. Weigh the naked infant. Most newborns weigh between six to nine pounds (2,700 and 4,000 grams). Record the weight in pounds and ounces, as well as in grams.
k. Measure the infant's length from top of the head to the heel with the leg fully extended and record measurements.
l. Measure the infant's head circumference and record measurements. The normal head circumference is 13 to 14 inches (33 to 35 cm). Cranial molding from a vaginal delivery may affect this measurement. The measurement should be repeated on the second and third day after delivery.
m. Measure the infant's chest circumference at the nipple line and record the measurement.
n. Observe the general contour of the infant's head. Gently palpate the sutures and fontanelles. The anterior fontanelle is approximately two inches long and is gem/diamond shaped. The posterior fontanelle is smaller than the anterior fontanelle. Normally, the fontanelle feels soft and is either flat or slightly indented. The anterior fontanelle usually bulges when the infant cries, coughs, or vomits.
o. Observe the general appearance of the infant's neck. The infant's neck is usually short, thick, and covered with folds of tissue. The infant should be able to move his neck from side to side, from flexion to extension, and can hold his head in the midline position.
p. Observe the infant's eyes for symmetry of size and shape. Note the infant's eye movements. Strabismus caused by poor neuromuscular control is normal. An infant older than ten days should look in the direction in which you turn. Note the color of the infant's eyes.
q. Inspect the infant's ears for structure, shape, and position. The ears should be firm with wee-formed cartilage. Tops of the auricles should be parallel to the outer canthus of the eye (refer to figure 7-5).
r. Inspect the infant's nose for patency.
s. Inspect the infant's mouth for cleft palate by gently depressing his tongue when he cries. Check the mucous membranes. Observe the soft and hard palate. Make sure they are in tact.
t. Inspect the infant's skin and nails. Observe for jaundice, birthmarks, milia, petechiae, and lanugo. Observe the infant's hands and feet for normal creases. Observe the color of the infant's nail beds; they should be pink. Acrocyanosis may be present up to 24 degrees, especially when the infant is crying.
u. Inspect the size, shape, and symmetry of the infant's chest. Normally, an infant's chest is circular or barrel-shaped. The breast tissue of both male and female infants may be slightly engorged during the first few days of life.
v. Palpate the infant's peripheral pulses (femoral, brachial, and radial).
w. Inspect the size and shape of the infant's abdomen. The abdomen should be cylindrical in shape. Sunken or distended abdomen should be reported. Check the umbilical cord for the number of vessels.
x. Auscultate the infant's abdomen for bowel sounds. Bowel sounds should be present within one to two hours after birth.
y. Observe for excessive drooling, coughing, gagging, or cyanosis during feeding.
z. Place the infant on his abdomen and observe his spine for curves, masses, or abnormal openings.
aa. Inspect the male infant's genitalia. The penis should be checked for location of the urinary meatus. The scrotum may appear edematous and proportionately large.
bb. Inspect the female infant's genitalia. The labia majora may appear edematous and cover the clitoris and the labia minora.
cc. Observe the infant's spontaneous or involuntary movements for symmetry, spasticity, or rigidity. Gently straighten his arm or leg. Release it and observe whether it returns to its normal position. If the extremity remains limp, the infant may be hypotonic. If the extremity is difficult to straighten and rapidly flexes when released, he may be hypertonic.
dd. Dress the infant carefully and return him to his bassinet.
ee. Record all significant nursing observations in the infants' health record. Report your observations to the Charge Nurse.
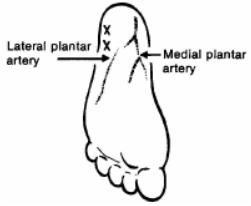
A phenylketonuria (PKU) test is done to check for rising levels of phenylalanine. Phenylalanine is a naturally occurring amino acid essential to growth. After milk or formula (both contain phenylalanine) feedings begin, levels rise due to a deficiency of the liver enzyme that converts phenylalanine to tyrosine. Due to this metabolic deficiency, poisons build up in the bloodstream and cause mental retardation. If the infant is found to have rising levels of phenylalanine, many protein foods can be withheld from the diet and synthetic foods substituted. The following steps are performed to collect a blood specimen for a PKU test on the newborn infant.
a. Ensure that the infant has been on milk or formula feeding for three full days. Four days are preferred.
b. Explain to the parents the purpose of the test
c. Perform a heel stick to obtain needed specimen (see figure 8-11).
d. Place one drop of blood on each of the three circles on the filter paper or in accordance with local policy.
e. Label and transport the specimen to the laboratory.
f. Notify the parents of follow-up care of the infant, if the infant is discharged prior to his third or fourth day of life. This test must be done.
8-13. GOALS OF NEWBORN NURSING CARE
a. To continue appraisal of the newborn throughout his hospital stay.
(1) Observe and record the infant's vital signs.
(2) Monitor weight loss or gain (daily by some local policy).
(3) Monitor bowel and bladder function.
(4) Monitor activity and sleep patterns.
(5) Monitor interactions and bonding with parents.
b. To provide safeguards against infection (that is, handwashing).
c. To initiate feedings.
d. To provide guidance and health instruction to parents.
8-14. DISCHARGE CONSIDERATION FOR THE NEWBORN AND FAMILY
a. Planning for discharge should begin at time of admission. An infant in normal health is discharged from the hospital at the same time as the mother.
b. Instructions for parents (teaching should be continuous).
(1) Feeding schedule.
(2) Bathing routine.
(3) Home care needs.
(4) Umbilical cord stump care.
(5) Infant safety in the car.
c. Prior to discharge, a follow-up appointment date should be arranged for the newborn (local policy determines the date-two, four, or six weeks).
d. A final identification check of the mother and the infant must be performed before the infant can be allowed to leave the hospital.
|
|||||||||
|
LESSON OBJECTIVES 8-1. Identify terms and definitions that are related to the normal newborn infant. 8-2. Identify procedures used to establish and maintain a newborn infant's airway. 8-3. Identify the common characteristics of a newborn infant's respirations. 8-4. Identify the signs and symptoms of respiratory distress in a newborn infant. 8-5. Identify the procedures for maintaining a newborn infant's body temperature. 8-6. Select the procedures for identifying the newborn infant before leaving the delivery room. 8-7. Identify the best time to begin the parent-infant bonding process. 8-8. Identify the purposes for APGAR scoring of the newborn infant. 8-9. Identify objective signs used for evaluation of the newborn infant. 8-10. Identify procedures for admission of the newborn infant to the nursery. 8-11. Identify procedures for weighing a newborn infant. 8-12. Identify procedures for aspirating fluids from a newborn infant. 8-13. Identify procedures used to evaluate the physical condition of a newborn infant. 8-14. Identify the purpose for administration of vitamin K to a newborn infant. 8-15. Identify the medications used in eye prophylaxis for a newborn infant. 8-16. Identify the two observations for cord care of the newborn infant. 8-17. Identify goals of nursing care for a newborn infant. |
|||||||||
|
|||||||||
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved