This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
Lesson 6: Changes of the Postpartal Patient
Section I. CHANGES OF THE POSTPARTAL PATIENT
The first six weeks following the birth of a baby is known as the postpartum period. During this period the reproductive organs of the mother return to their prepregnant state. There are marked anatomic and physiologic changes as the physiologic processes that are designed to accommodate pregnancy are revised. In caring for a patient during the postpartal period, the nurse must have a good understanding of the physiologic and psychological adaptations that occur during this time. With this knowledge and understanding the nurse is able to recognize any abnormal findings and to intervene as necessary.
6-2. CHANGES IN THE REPRODUCTIVE SYSTEM FOLLOWING DELIVERY
a. The Uterus.
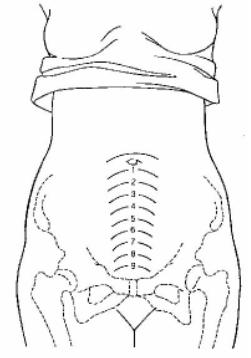
(1) Major changes in the uterus. Immediately after the placenta and membranes are delivered, the placenta site is elevated, irregular, and partially obliterated by vascular constriction and thrombosis. In other words, the placental attachment site is sealed in order to prevent bleeding. The uterus gradually returns to its approximate prepregnant size. This is accomplished by a decrease in the size of the individual myometrial cells and is usually accomplished by 4 to 6 weeks postpartum. The process is referred to as uterine involution. The uterine size usually increases slightly after each pregnancy. A soft and boggy uterus, due to relaxation, requires immediate massage until it is contracted again. This is done to stop bleeding. The height of the uterus after delivery can be used to measure the process of uterine involution while the mother is hospitalized. See figure 6-1 to view the following changes of the uterus:
(a) Immediately after delivery- midway between the umbilicus and symphysis pubis.
(b) Twelve hours after delivery-above the umbilicus.
(c) After that - the fundus descends about one fingerbreadth every 24 hours.
(d) After the tenth day of postpartum--the uterus should not be palpable abdominally.
(2) Afterpains. Afterpains are referred to as uterine contractions which continue following delivery, but occur less frequently than during labor and have an irregular pattern. Periodic relaxations add contractions. This is common and causes the afterpains for multiparas. They may last two to three days. Breast-feeding intensifies the afterpains. This is due to oxytocin being released by the posterior pituitary in response to stimulation of the nipple. Nursing measures used to relieve afterpains are as follows:
(a) Have the mother to assume a prone position.
(b) Have the mother to place a hot water bottle on her abdomen.
(c) Have the mother to void often to keep the bladder empty.
(d) Inform the mother to drink hot liquid, this will help to ease the pain.
(e) Give analgesics per physician's order.
|
b. Lochia Flow. One of the most unique capabilities of the uterus is its ability to rid itself of the debris remaining after delivery. This process is known as lochia flow. This is the vaginal discharge during the puerperium consisting of blood, tissue, and mucous. It may last up to six weeks after delivery. It is important for the nurse, as well as the patient, to be concerned with the following facts about lochia flow:
(1) Types of lochia (in order of occurrence).
(a) Lochia rubra-a red, distinctly blood-tinged vaginal flow that follows delivery. It lasts from two to four days after delivery.
(b) Lochia serosa-a serous, pinkish brown, watery vaginal discharge that follows lochia rubra. It lasts until about the 10th day after delivery.
(c) Lochia alba-a thin, yellowish to white, vaginal discharge that follows lochia serosa on about the 10th post delivery day. It may last from the end of the third to the sixth post delivery week.
(2) Lochia with a foul-smell or a green-tinge may indicate infection.
(3) Lochia clots whereas normal menstrual flow does not.
(4) Normal lochia flow should stop within three to four weeks postpartum.
(5) An increase in lochia flow may indicate a retained placenta or a patient who is not getting enough rest.
(6) Lochia flow is slightly heavier after breast-feeding, which is due to the release of oxytocin. Oxytocin causes the uterus to contract.
c. Changes in the Cervix. Initially, the cervix appears soft and edematous and has little tone. Multiple small lacerations may be seen. The cervix constricts rapidly and regains its shape by the end of the first week. Then, it is firm and thicker. The external os is contracted, only about one cm dilated. The cervix is healed by the fourth to sixth week after delivery. The extended os will assume a typical transverse slit of a parous woman.
d. Changes in the Vagina. Initially, the vagina is swollen and has poor tone following vaginal delivery. It remains distensible, regains its tone and returns to its original size by the fourth to sixth week of the postpartal period. The patient can help to improve tone and contractibility of the vaginal orifice by performing the Kegel's exercise (perineal tightening). Lacerations resulting from childbirth heal completely.
e. Changes in the Perineum. Initially, swelling and tenderness as a result of childbearing is present. Bruising and rupture of blood vessels are usually evident. By the fourth to sixth week postpartum, the episiotomy or laceration is usually evident. There is no more swelling and tenderness in the perineum area.
6-3. CHANGES IN THE CARDIOVASCULAR SYSTEM FOLLOWING DELIVERY
a. Blood Volume. Initially, there is a 15 to 30 percent increase in circulating blood volume the first 20 days of postpartum. This results from the elimination of placental circulation and an increase in venous return. The increase is responsible for profound diuresis in early postpartum and a fall in hematocrit. This is why early postpartum time is the greatest risk for heart failure in patients with cardiac disease or limited cardiac reserve.
b. Hematocrit. The hematocrit drops because of blood loss during actual delivery. It usually rises by the third to seventh postpartum day unless substantial blood loss has occurred. Normal blood loss is about 250cc for vaginal delivery. This varies considerably. Blood loss must be greater than 500cc to be considered hemorrhage.
6-4. FACTS ABOUT THE URINARY SYSTEM FOLLOWING DELIVERY
The bladder mucosa shows varying degrees of edema and hyperemia, with diminished bladder tone after delivery. This results in decreased sensation to increased pressure, increased capacity, overdistention with overflow incontinence, and incomplete emptying of the bladder. Nursing care must include careful monitoring of the condition of the bladder. Distention and urinary retention are common occurrences and can cause discomfort as well as predispose a patient to infection, uterine atony and heavy bleeding, and may cause the patient's blood pressure to increase. With adequate emptying of the bladder, tone is usually restored within five to seven days.
6-5. FACTS ABOUT OVULATION AND MENSTRUATION FOLLOWING DELIVERY
Amenorrhea (cessation of menstruation) helps the body to conserve body fluids. Reestablishment of ovulation and menstruation is influenced by whether the mother is breast-feeding or not. Ovulation is delayed in direct proportion to the amount and length of time the baby is breast-fed. The absence of menstruation in a breast-feeding mother does not necessarily indicate absence of ovulation. Breast-feeding is not a means of birth control; contraceptives should be used.
6-6. FACTS ABOUT BREASTS AND LACTATION FOLLOWING DELIVERY
The concentrations of hormones that stimulated breast development during pregnancy decreases promptly after delivery. The time it takes for the return of these hormones to prepregnancy levels is determined in part by whether the mother breast-feds her infant.
|
a. Milk. Does not appear until three or four days after delivery.
b. Colostrum. This is the watery prolactations secretion that is first evident during the second trimester. It is secreted for the first several days after delivery in increasing amounts. Characteristics of colostrum are as follows:
(1) Thick, yellow fluid during pregnancy which changes to thin before delivery.
(2) Higher in protein and inorganic salts than breast milk.
(3) Lower in fats and carbohydrates than breast milk.
(4) Contains high levels of antibodies, which protect the infant against enteric infections.
(5) Nutritive value is lower than that of breast milk.
(6) Acts as a laxative for the newborn.
c. Lactation.
(1) As previously mentioned, breast milk usually comes three or four days postpartum. The color is bluish white. The milk causes a fullness and tenderness to the breasts which is known as engorgement. This congestion usually subsides in one to two days. Ejection reflex can be adversely affected by extreme factors such as anxiety, tension, or severe cold or pain. The infant should be breast-fed in a comfortable, relaxed setting. Some medications may be excreted through the breast milk.
(2) Suppression of breast milk by non-nursing mothers is simple and most natural. The mother should:
(a) Not allow the infant to suck.
(b) Not stimulate the breast or nipples.
(c) Wear a tight bra.
(d) Avoid hot showers.
(e) Apply ice packs to the breast if engorgement occurs.
NOTE: Hormonal methods to suppress breast milk are administered during the postpartum period. This method suppresses the production of prolactin.
(3) The dietary requirements of the lactating mother should include increase amounts of protein, calcium, iron, and vitamins. An increase in fluid intake is also necessary. The amount of breast milk production is directly proportional to fluid intake. Additional fluids are required in hot, humid climates.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved