This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
|
Lesson 4: Management of Obstetric Discomfort During Labor
The management of obstetric discomfort during labor is the responsibility of all nursing personnel. The relief or reduction of pain during labor can be achieved by several different methods (that is, psychoprophylactic methods, systemic drugs, local and regional nerve blocks, and general anesthesia). It will be important to you to have an understanding of where the discomfort originates, the nursing interventions to be provided, and measures used by the physician to help relieve discomforts experienced during labor.
4-2. SOURCES OF DISCOMFORT DURING CHILDBIRTH
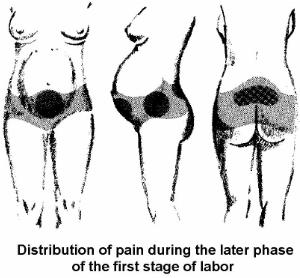
a. Visceral Discomfort (Abdominal or Internal Organs). This occurs most often during the first stage of labor. It results from uterine contractions. Discomfort is felt in the lower abdomen, lumbar region, and thighs. The mother will be free of pain between contractions.
b. Perineal Discomfort. The greatest discomfort is felt during the second stage of labor. This is when the cervix is dilating from 8 to 10 cm. Discomfort is due to the stretching of the vagina and the perineum as the presenting part moves through the birth canal.
4-3. FACTORS THAT MAY INFLUENCE THE AMOUNT OF PAINFUL STIMULI
|
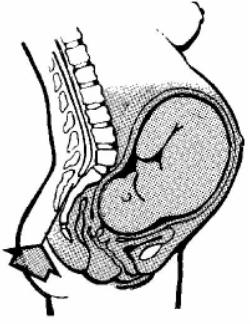
Figure 4-1. Areas of pain |
a. Patient's Pelvic Anatomy Itself. If the patient's pelvic anatomy is large, it may be easily expandable and if it is small, more stretching and increased intraabdominal pressure may be required.
b. Fetal Head Size. A large head would require more room and more time to descend and deliver. A small head may pass through the pelvis with a minimal amount of stretching.
c. Strength, Frequency, and Duration of Uterine Contractions.
(1) Extremely strong contractions may cause significant discomfort to the patient.
(2) Contractions occurring every two to three minutes may cause the patient to be fatigued and less tolerable of the discomfort.
(3) Contractions continually lasting sixty to ninety seconds require a great deal of tolerance and concentration by the patient.
d. Presence or Absence of Certain Obstetrical Deviations or Complications. The need for induction may result in longer, harder labor than if labor was spontaneous. Problems with the fetus in utero may preclude the patient from receiving any type of sedation.
e. Patient's Pain Threshold. It is believed that the pain felt may be altered by the level of available morphine-like hormonal substances in the body called endorphins. Endorphins are a special protein. They appear to interfere with transmission of pain producing impulses to the brain or may interfere with the brain's sensitivity to these impulses. Endorphin levels decrease in the presence of anxiety, tension, fatigue, and extended negative stimuli.
NOTE: See figure 4-1 for areas of pain.
4-4. EVALUATION OF THE DEGREE OF PAIN BEING EXPERIENCED
a. What The Mother Says. Is she requesting pain medication? Is she talking during the actual contraction?
b. Patient's Response. Comparison of the patient's response to a given specific phase of labor to the expected response for that phase is considered. The patient is usually talkative and able to walk about during the latent phase. Whereas, the patient may be nauseated, irritable, and uncooperative in the transition phase.
c. Facial Expression. This usually gives the truest impression. Grimacing indicates increased pain.
d. Color of Skin. If the patient's skin is pale, she may be weak or tired. If she is perspiring, she may be working hard with each contraction.
e. Blood Pressure, Pulse, and Respirations. The patient's blood pressure is expected to elevate during the actual contraction, which is due to vasoconstriction. Her blood pressure should be taken at least fifteen seconds after contractions subsides. As anxiety and pain increase, the patient's blood pressure, pulse, and respiration increase.
f. Posture. The patient may become stiff and tense up. This is an indication that the patient is not tolerating well. Her legs and arms may be loose and relaxed. This indicates that the patient is effectively dilating with contractions.
4-5. GOALS OF NURSING MEASURES TO MINIMIZE DISCOMFORT DURING CHILDBIRTH
Nursing measures to minimize discomfort during childbirth involves two areas. They are to decrease the intensity of pain and to minimize the degree to which the patient is bothered by pain. In decreasing the intensity of pain, the patient is given the opportunity to rest and is allowed more involved participation in the childbirth process. In addition, minimizing the degree to which the patient is bothered by pain will allow her to progress faster and keep her from becoming so fatigued.
4-6. NURSING MEASURES UTILIZED TO MINIMIZE DISCOMFORT DURING CHILDBIRTH
a. Give Frequent Explanations to the Patient.
(1) Explain to the patient what she is to expect, especially if she did not attend childbirth classes.
(2) Give simple and straightforward answers.
(3) Inform the patient of all progress. Do not give specific times for progress.
(4) Emphasize that pain diminishes between contractions. Encourage the patient to relax. Have her close her eyes and sleep.
(5) Ease panic associated with pain. Remind the patient of safety measures required for the baby and encourage concentration during the contractions.
b. Provide Comfort Measures.
(1) Ensure that there is clean and dry bedding and a clean gown.
(2) Inform the patient of frequent oral hygiene, especially after vomiting. This includes brushing the teeth and using mouthwash.
(3) Provide ice chips.
(4) Provide a cool cloth for the patient's face, if necessary.
(5) Give back rubs or pressure, especially over the lower sacrum area.
(6) Position the patient as needed. The side lying position is recommended. Lying on the left side is preferred because it increases placental flow. Place pillows behind the patient's back and between her legs, as necessary.
(7) Provide for a quiet room. Dim the lights if possible to encourage relaxation.
(8) Have the patient void every 2 hours; assist as needed.
c. Encourage the Use of Psychoprophylaxis.
Psychoprophylaxis refers to the mental and physical education of the parents in preparation for childbirth, with the goal of minimizing the fear and pain and promoting positive family relationships. This includes relaxation techniques and exercises learned during prepared childbirth classes.
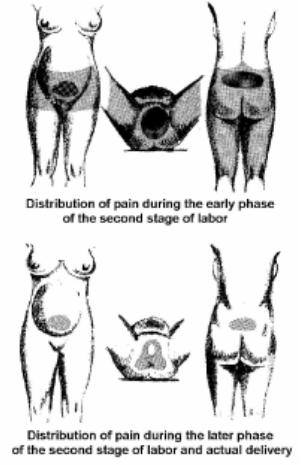
(1) Relaxation techniques include breathing during contractions, concentration on the focal point, and effleurage (see figure4-2). Effleurage is a light, rhythmic stroking techniques used during childbirth.
(2) The pelvic tilt and abdominal exercises are the exercises to be used.
d. Explain the Effects of Analgesic Medications During Labor.
(1) Fetus. What the patient in labor receives crosses the placenta and goes to the fetus. The fetus becomes sedated as a result of the medication. It may cause respiratory distress in the fetus if it is not worn off by the time of delivery. Medication is not usually given if the fetus is premature due to problems they have detoxifying the drug due to the immature system. It is, also, not usually given if the fetus is already showing signs of compromise or distress.
(2) Mother. The medication will make the patient sleepy or drowsy. It will not totally eliminate the discomfort. When given during the active phase, it may cause appropriate maternal relaxation that results in more rapid dilatation. It is not generally given during the latent phase (less than 4 cm dilatation) because it may interrupt a regular contraction pattern. It is not generally given in the transitional phase (greater than 8 cm dilatation) as delivery time cannot be predicted exactly and the infant may be born under the full impact of the medication.
(3) Labor and delivery process. Medications may slow labor down and space contractions further apart. In addition, it may speed the labor due to the relaxed state of the patient.
4-7. CLASSIFICATION OF DRUGS USED FOR CHILDBIRTH
a. Analgesics (Narcotics and Nonnarcotics). Analgesics refer to a technique or medication that reduces or eliminates pain. A narcotic analgesic produces the same amount of CNS depression in the fetus as that produced in the mother. Analgesics are the most common form used in obstetrics today. They include:
|
(1) Demerol®--narcotic.
(2) Morphine®--narcotic.
(3) Stadol®--nonnarcotic.
(4) Nubain®--narcotic.
(5) Nisentil®--narcotic.
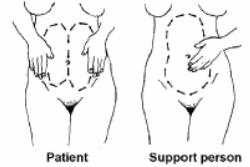
b. Anesthetic. Anesthetic refers to a technique or medication that partially or completely eliminates sensation or feeling. There are two types of nerve-blocking anesthetics, local and regional. Local anesthetics block sensory nerve pathways at the organ level. Regional anesthetics block sensory nerve pathways along the course of tissues. Refer to figure 4-3 for the level of anesthesia necessary for cesarean and vaginal delivery.
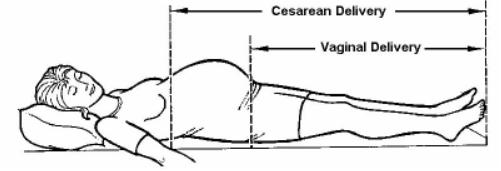
Figure 4-3. Level of anesthesia for cesarean and vaginal delivery.
c. Sedative or Tranquilizer. This refers to a medication that relieves anxiety and quiets the patient. It may combine with analgesics to enhance the effects of analgesics (although that effect is now being questioned). The primary ones for obstetrics are:
(1) Phenergan®--given more for its antiemetic effect.
NOTE: Antiemetic refers to preventing or alleviating nausea and vomiting.
(2) Vistaril®.
(3) Largon®.
4-8. NERVE-BLOCKING ANESTHETICS USED IN OBSTETRICS
a. Local. Local anesthetics produces anesthesia only in the area where injected. It is used in the superficial nerves of the perineum to make or repair episiotomy. Lidocaine® 1percent drug normally used and is short acting. Local anesthetics are used frequently for delivery.
b. Regional. Regional anesthetics include paracervical block, pudendal block, saddle block (low spinal), and caudal or lumbar epidural. (See figure 4-4.)
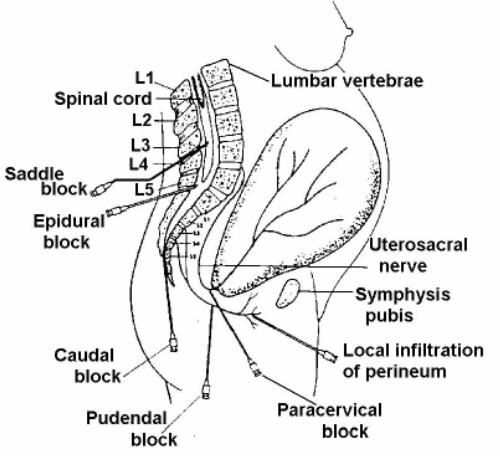
Figure 4-4. Injection sites for regional anesthetics.
(1) Paracervical block. Paracervical block (see figures. 4-4 and 4-5) is an injection of a dilute local anesthetic into the paracervical nerve endings through the vagina. There is relief within five minutes after administration and is good for about 45 to 60 minutes. The patient doesn't feel the cervical pain related to the uterine contractions.
When the anesthetic is injected into the tissues lateral to the cervix, it is picked up by the circulation, which quickly involves the uterus and placenta. When overdosage occurs, the fetus may exhibit bradycardia because of the quinidine-like effect of the anesthetic on the myocardium or quinidine due to a reduction in uterine blood flow. In addition, CNS medullary depression may develop and the neonate may show vascular collapse and apnea at delivery. These are potential complications and continuous fetal monitoring is required.
(2) Pudendal block. Pudendal block (see figures. 4-4 and 4-6) is an injection of local anesthetic on both sides of the vagina. It is administered just prior to delivery. It numbs the perineal area, vulva, and the vagina. It is used frequently in labor and delivery in combination with local anesthesia.
 Figure 4-6. Pudendal block. |
|
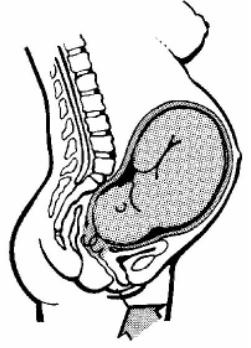
(3) Saddle block (low spinal). Saddle block (low spinal) (see figure 4-7) is an injection of anesthetic agent directly into the spinal canal below the spinal column to cause loss of sensation below the injection site. The patient has to sit up on the table with legs crossed or hanging over the side. The doctor should numb just the areas that would be touched. The saddle block numbs the abdominal and pelvic areas below the umbilicus to include the perineum, legs, and feet. It blocks the urge to push although the ability is still there. The patient will usually feel contractions. The side effects are severe maternal hypotension due to vasodilation and decreased oxygen to the fetus as a result of hypotension.
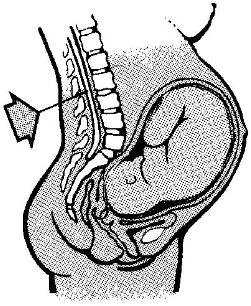 Figure 4-7. Saddle block. |
(4) Caudal or lumbal epidural.
(a) Caudal is an injection of anesthetic agent in the peridural space through the sacral hiatus (see figure 4-8). Lumbar epidural is an injection of anesthetic agent on top of the dura space through the 3rd and 4th or 5th lumbar space. These anesthetics numb the abdominal and pelvic areas below the umbilicus to the midthigh. The patient doesn't feel contractions or perineal stretching. The urge to push may be blocked, although the ability is still present.
(b) The advantages of caudal or lumbar epidural are that they are a good pain relief, the patient is alert and cooperative, and there is decreased danger of neonatal depression.
(c) The side effects include:
1 Hypotension secondary to peripheral vasodilation.
2 If dura infusion -- lower extremity sensory changes and loss of the ability to move lower extremities.
3 If blood stream infusion -- ringing in the ears, lightheadedness, circumoral (around mouth) tingling, numbness, metallic taste, and seizures.
4 Burning at the site of injection.
(d) The patient should be informed about the pressure she may feel. She may have a "crazy bone" feeling in her legs, hip, or back at the time the catheter is inserted if it touches a nerve.
(e) Both the caudal and the lumbar epidural require frequent observation and a physician's administration, which limits their use.
|
|
a. General anesthesia produces loss of sensation and loss of consciousness. It is seldom indicated for uncomplicated vaginal delivery. It is used in cases of fetal distress requiring immediate delivery and used for C-section when spinal anesthesia is contraindicated.
b. The disadvantages are as follows:
(1) The patient is unable to participate.
(2) It rapidly crosses the placenta causing fetal anesthesia, respiratory depression, and possible anoxia (loss of oxygen).
(3) There is increased risk of maternal aspiration -- evaluate how recently the patient has eaten.
(4) There is possible hemorrhage since nitrous oxide yields uterine relaxation.
4-10. NURSING CARE GIVEN TO THE OBSTETRIC PATIENT RECEIVING ANESTHESIA
a. Continue monitoring the labor patterns, fetal heart rate, blood pressure, and pulse.
b. Observe closely for side effects, most frequently maternal hypotension and fetal bradycardia.
c. Provide emotional support for the patient and her partner.
d. Maintain appropriate emergency equipment for maternal hypotension or fetal bradycardia. The equipment includes oxygen with facemask, suction, airways, and I.V. fluids.
e. Monitor bladder status at least every 2 hours. The sensation to urinate is lost with some anesthetics. If the bladder is distended, a physician's order may be required for in and out catherization.
4-11. NURSING CARE FOR MATERNAL HYPOTENSION IN THE OBSTETRIC PATIENT
a. Position the patient on her left side. This relieves uterine pressure on the inferior vena cava and iliac veins and it increases oxygen supply to the fetus.
b. Administer oxygen per facemask, usually at 5 to 8 liters/minutes, as ordered.
c. Elevate the patient's legs.
d. Stay with the patient, do not leave her unattended.
e. Notify the Charge Nurse or physician immediately.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved