This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
|
Lesson 1: Complications of Pregnancy
Being aware of conditions that can cause complications in pregnant women will be an asset to you, as a practical nurse, in your knowledge and skills in providing care to the patient. Complications of pregnancy can be an emotional crisis to a patient and her support person. Prenatal care allows for early identification and management of a patient with complications.
a. One of the first discomforts experienced in pregnancy, which generally occurs in the morning is nausea and vomiting. It is attributed to the great hormonal changes during the early stages of pregnancy.
b. Nursing interventions consist of advising the patient:
(1) To eat small, frequent meals instead of three large meals.
(2) To drink liquids (such as 7-Up™ or ginger ale) between meals instead of with meals.
(3) To eat a few crackers or toast before getting out of bed in the morning.
(4) That the nausea and vomiting should subside in the second trimester of pregnancy, but if not, she MUST report this condition to her health care provider.
a. Hyperemesis gravidarum refers to persistent severe nausea and vomiting which results in dehydration, ketouria, and possible weight loss. The exact cause is unknown. If left untreated, it can cause fetal death.
b. Nursing implications include the following:
(1) Record accurate intake and output to include emesis.
(2) Monitor intravenously (IV) solutions ordered by the physician.
(3) Record the patient's weight daily.
(4) Assess the patient for skin damage if dehydration is obvious.
(5) Implement prophylactic measures (lotions, massages, op-site) to prevent skin breakdown.
(6) Be alert to the psychological needs of the patient. She may be concerned about this crisis and of the results on herself and the fetus.
a. Heartburn is a burning sensation in the epigastric and sternal region. It results from relaxation of the cardiac sphincter and the decreased tone and mobility of smooth muscles due to increased progesterone, thereby allowing for esophageal regurgitation, decreased emptying time of the stomach, and reverse peristalsis. Heartburn has nothing to do with the heart. It occurs more frequently as pregnancy advances as a result of decreased peristalsis and pressure of the growing fetus on the stomach.
b. Nursing interventions consist of advising the patient to:
(1) Not to lie flat after eating. Sitting or walking helps gravity move the food through the gastrointestinal tract.
(2) Drink a glass of milk about 1/2 hour before eating. This will inhibit the secretion of stomach acid.
(3) Avoid eating or drinking gas-forming foods or fluids (cabbage, beans, cokes, etc.).
(4) Not take any antacid unless ordered by her obstetric (OB) practitioner or physician. Sodium bicarbonate and Alka-Seltzer™ contain high amounts of sodium.
(5) Eat small, frequent, non-spicy, non-fried meals and drink adequate fluids.
a. There are many types of infection which the patient can contact during pregnancy. However, the most prevalent infections are urinary track infections, venereal diseases, and human immunodeficiency virus (HIV).
(1) Urinary track infections. Infections of the urinary track are common during pregnancy. The infections are caused by the narrowing of the lower urethra and dilation of the upper urethra. This action results in a slowing of urination, which increases the risk of infection.
(2) Venereal diseases. Venereal disease (VD) or sexually-transmitted disease (STD) refers to one of a number of infectious diseases that are transmitted through sexual contact and may be localized or systemic. Common types of VD are gonorrhea, syphilis, venereal warts, and herpes simplex type II. Microorganisms from these diseases can cross the placenta barrier, placing the fetus at risk.
(3) Human immunodeficiency virus. The transmission of human immunodeficiency virus occurs primarily through the exchange of body fluids (blood, semen, and perinatal events). Severe depression of the cellular immune system characterizes acquired immune deficiency syndrome (AIDS). Exposure to the virus has a significant impact on the woman's pregnancy, the newborn's feeding method, and the newborn's health status. The HIV from infected pregnant women is transmitted in three ways:
(a) To the fetus-as early as the first trimester through maternal circulation.
(b) To the infant-during labor and delivery by inoculation or ingestion of maternal blood and other infected fluids.
(c) To the infant-through breast milk.
b. Nursing implications include the following.
(1) Teach the patient to attend scheduled prenatal appointments.
(2) Inform the patient of specific lab tests that will be obtained for early detection of diseases (VDRL, gonorrheal culture, and HIV blood tests).
1-6. VARICOSITIES (VARICOSE VEINS)
a. Varicosities refer to dilated, tortuous veins that result from incompetent values within those veins. The valves close incompetently or not at all. Blood is thus permitted to seep backward rather than being propelled always toward the heart. This seepage causes further congestion of the part with venous blood and further distention of the veins.
|
b. Factors associated with varicosities include the following.
(1) The saphenous veins of the legs are commonly affected with varicosities. It can also occur in the external genitalia (vulva or labia), the pelvis, and the perianal area (hemorrhoids).
(2) Some people have familial tendency toward varicosities.
(3) Weight gain associated with the enlarging uterus impairs venous return.
(4) Prolonged sitting (to include with legs crossed at knees) and standing can contribute to development of varicosities.
(5) Wearing of constrictive clothing may also cause varicosities.
(6) Relaxation of smooth muscles, which is due to hormonal changes during pregnancy, is also thought to contribute to the development of varicosities.
(7) Varicosities are seen as dark blue or purplish swellings.
(8) The patient may complain of heavy and tired feelings in the legs or a burning, cramping sensation.
c. Nursing implications include the following.
(1) Encourage the patient to lie down with her hips/legs elevated periodically throughout the day.
(2) Inform the patient that elastic stockings applied before rising may lessen discomfort.
(3) Inform the patient of proper nutritional habits to avoid constipation.
(4) Inform the patient not to bear down with bowel movements.
(5) Inform the patient to avoid prolonged sitting or standing greater than 15 minutes without a change of position.
(6) Inform the patient not to massage her legs.
(7) Inform the patient to discuss possible surgical treatment of varicosities if persistent after pregnancy.
a. Maternal acidosis refers to a complex disorder of carbohydrates, fat, and protein metabolism caused primarily by a relative or complete lack of insulin secretion by the beta cells of the pancreas. Although there is an overall improvement in the perinatal outcome of the well-managed diabetic pregnancy, there is still a significant risk for neonatal morbidity. The most common cause of fetal death associated with diabetes is maternal acidosis. Possibilities of diabetes being present are:
(1) Birth of a large baby over nine pounds.
(2) Repetitive, spontaneous abortions.
(3) Unexplained stillbirth.
(4) Excessive amniotic fluid (Polyhydramnios).
b. Diabetic patients are at risk for developing preeclampsia. They also have a risk of a difficult delivery as a result of the large size of the baby.
c. Nursing implications are as follow.
(1) Test patient's urine for glucose with clinitest tabs as ordered by OB practitioner or physician.
(2) Administer oral hypoglycemic medications or insulin as ordered by the OB practitioner or physician.
(3) Teach the patient the left lateral-recumbent position to rest. This position improves intrauterine blood flow and may decrease the occurrence of preeclampsia.
(4) Apply all nursing implications learned for the care of an adult with diabetes.
1-8. HYPERTENSION-PREGNANCY-INDUCED
Hypertension-Pregnancy-Induced (PIH) is another name for preeclampsia or eclampsia. It is a serious, statistically important disorder characterized by the development after the twentieth week of gestation of hypertension, with albuminuria or edema or both. The exact cause of PIH is unknown.
a. Preeclampsia. The signs of preeclampsia are referred as being classic (see figure 1-1).
(1) Hypertension. Hypertension is blood pressure, which is greater than 140/90, but less that 160/110.
(2) Albuminuria. Albumin (a protein) is not normally found in the urine.
(3) Edema. There is a swelling of the upper body (hands and face) in addition to swelling of the ankles, which is normally seen in pregnancy.
b. Eclampsia. This refers to the progression of the above classic signs with the addition of convulsions or a coma.
| * Hypertension * Albuminuria * Edema * Convulsion or Coma in True Eclampsia |
Figure 1-1. Classic signs of preeclampsia and eclampsia.
c. Nursing Implications.
(1) Inform the patient to record her weight weekly and to notify the clinic if there is an excessively amount of weight gained.
(2) Inform the patient to avoid foods high in sodium content. This will reduce water retention/edema.
(3) Inform the patient that prevention of preeclampsia is essential to a healthy pregnancy and keeping scheduled OB appointments is a must.
a. The adverse effects of exposure of the fetus to drugs are variable. They include transient behavioral changes (such as fetal breathing movements) or irreversible effects (such as fetal death, intrauterine growth retardation, structure malformations, or mental retardation). Maternal use of drugs may be for the pharmacologic control of disease process (for example, insulin) or for symptomatic relief of benign problems (for example, aspirin). In addition to the therapeutic use of drugs, the nontherapeutic use of drugs such as alcohol, nicotine, or narcotics poses threats to the fetal's well-being. Substance abuse results in fetal alcohol syndrome (FAS), a syndrome characterized by physical and mental abnormalities of the newborn.
b. Nursing implications are listed below.
(1) Apply all general nursing implications related to the substance abuse patient.
(2) Participate in health team discharge planning for the substance dependent mother and newborn with social services.
|
a. The battered, pregnant woman often has medical, social, and psychological needs that require special attention. An assault on a pregnant patient jeopardizes her body as well as the fetus. The patient suffers extensive psychological trauma.
b. Nursing implications are listed below.
(1) Assess the emotional needs of the patient and the significant support person.
(2) Promote a trust relationship which will foster self-esteem and a positive pregnancy experience.
(3) Inform the patient and the spouse about counseling.
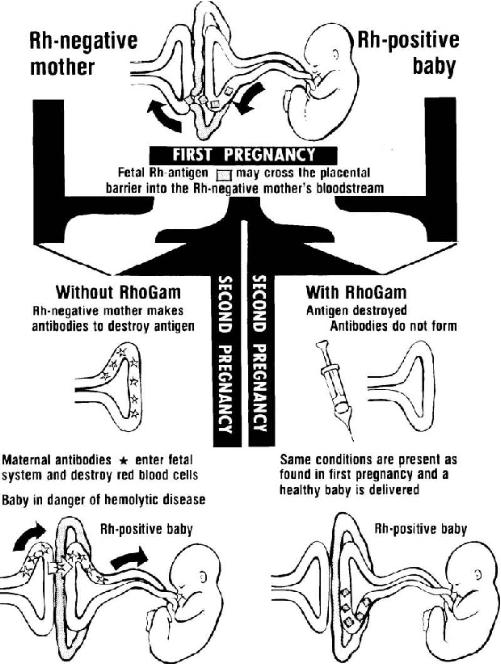
a. RhoGAM® incompatibility occurs when the Rh-negative pregnant patient carries an Rh-positive fetus. The patient's body reacts to the "foreign" fetus blood type. The mother produces antibodies that in-turn causes destruction of the fetus red blood cells (hemolysis). Hemolysis of the fetus red blood cells deprives the fetus of oxygen (erythroblastosis fetalis).
b. The treatment for Rh incompatability is given below.
(1) RhoGAM® (immune globulin) administered 72 hours following the birth of an Rh-positive child will eliminate maternal isoimmunization. Refer to figure 1-2.
(2) An Rh-negative patient whose sex partner is Rh-positive, who aborts or has an ectopic pregnancy, should receive RhoGAM®. This is essential to prevent the patient from developing Rh-positive antibodies.
c. Nursing implications are listed below.
(1) Follow the obstetrics (OB) practitioner's or physician's orders for drawing of Rh antibody titer.
(2) Follow delivery room standing operating procedure (SOP) to obtain cord blood sample to determine baby's blood type.
Figure 1-2. Rh factors.
|
|||||||||
|
LESSON OBJECTIVES After completing this lesson, you should be able to: 1-1. Identify facts concerning complications and nursing implications of a pregnant woman, including are: |
|||||||||
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007 Medical Education Division, Brookside Associates, Ltd. All rights reserved