|
OBGYN Skills Lab
|
|||||||||
|
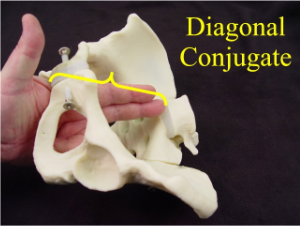
Pelvic Exam During Labor Video Pelvic exams are used during labor for initial assessment, measurement of progress, evaluation of fetal presentation and position, and determining the status of fetal membranes. During labor, several measurable changes occur to the cervix, including cervical dilatation, effacement and descent of the presenting part. To watch the video, click here Dilatation refers to the opening of the cervix and is expressed in centimeters. The opening of this water bottle is about 2 centimeters. If it were a cervix, you would say it is 2 centimeters dilated. To gain experience in accurately evaluating dilatation, try measuring various objects and then use a centimeter ruler to check your estimate. Effacement refers to the thickness of the cervix, typically recorded in centimeters. If this water bottle neck were a cervix, you would say it is two centimeters thick. Station refers to the location of the leading edge of the presenting part, relative to the ischial spines. If the leading edge is even with the spines, that is called zero station. If the leading edge is one centimeter below the spines, that is plus one station. Plus two station means two centimeters below the spines and plus three station is three centimeters below the spines. Minus one station means the leading edge is one centimeter above the ischial spines. The ischial spines are usually easily palpated during pelvic examinations. Serial measurements can be tracked over time to assist in evaluating labor progress. Most labors progress normally, but some do not, and the causes of abnormal can often be determined from this graphical display. Babies are usually delivered occiput anterior facing down. Some are born occiput posterior, facing up. This fetal position does matter since it can influence both the course of labor and delivery. Begin by determining whether the presentation is cephalic or breech. The fetal skull is rounded, firm and smooth. In contrast, the fetal breech is soft, with some bony prominences. Feet have a distinctive feel, and hands may present with the head as a compound presentation. Should you encounter a prolapsed umbilical cord, with the cord coming before the fetal head, this is an obstetrical emergency. Move the patient into the knee-chest position and try to elevate the fetal head off the cord with your examining hand. Transport the patient in this position to the delivery room for immediate delivery. With fetal heads, it is easiest to first find the sagital suture. Once that is located, the anterior fontanelle is identified by four suture lines coming together. The anterior fontanelle is diamond shaped, but the forces of labor may distort that landmark. Next, identify the posterior fontanelle at the junction of three suture lines. The soft, triangular shaped depression may or may not be present because of compression of the fetal head. With breech presentations, the midline is first identified, followed by the bony prominence of the fetal sacrum. The status of the fetal membranes can be determined during an exam. Sometimes the free flow of clear or meconium stained amniotic fluid makes it obvious that the bag of waters is ruptured. In other cases, it may be prudent to perform a sterile speculum exam to obtain a specimen from the upper vagina for further testing. Vaginal secretions are normally mildly acidic. The presence of alkaline amniotic fluid will turn the nitrazine paper bright blue. Other methods include examining dried fluid for ferning. Clinical pelvimetry may be used to estimate the pelvic capacity for delivery. Digital evaluation allows the examiner to categorize the pelvis as probably adequate, borderline, or small for an average sized baby. Measure the diagonal conjugate by inserting two fingers into the vagina until they reach the sacral promontory. The distance from the sacral promontory to the exterior portion of the symphysis is the diagonal conjugate and should be greater than 11.5 cm. Feel the ischial spines for their relative prominence or flatness. Spinal prominence narrows the transverse diameter of the pelvis and can make delivery more difficult. Feel the pelvic sidewalls to determine whether they are parallel, diverging or converging. Parallel or diverging are fine, but converging is associated with outlet obstruction. Fortunately, true outlet obstruction is rare. Measure the distance between the ischial tuberosities by pressing your closed fist against the perineum. Greater than 8 centimeters is considered normal. |
||||||||
|
This information is provided by The Brookside Associates, a private organization, not affiliated with any governmental agency. The opinions presented here are those of the author and do not necessarily represent the opinions of the Brookside Associates. For educational simplicity, only one method is usually shown, but many alternative methods may give satisfactory or superior results. This information is provided solely for educational purposes. The practice of medicine and surgery is regulated by statute and restricted to licensed professionals and those in training under supervision. Performing these procedures outside of that setting is a bad idea, is not recommended, and may be illegal. The presence of any advertising on these pages does not constitute an endorsement of that product or service by the Brookside Associates. C. 2010 All Rights Reserved |
|||||||||
 This is the Archived Desktop Edition.
This is the Archived Desktop Edition.