|
Mild dysplasia means the skin cells of the cervix are reproducing slightly
more quickly than normal. The cells are slightly more plump than they should be and have
larger, darker nuclei. This is not cancer, but does have some pre-malignant potential in
some women. Other phrases that describe mild dysplasia include:
Many factors contribute the development of mild dysplasia, but infection
with HPV, (Human Papilloma Virus) is probably the most important. Immune
system impairment may also contribute.
Mild dysplasia is not a permanent feature once it
occurs. It can come and go, being present on a woman's cervix (and Pap
smear) at one time and not another. This happens because the HPV
virus that is a pre-requisite for these changes can lie dormant within
the cervical skin cells. Normally held in check by the woman's immune
system, the HPV can, at times of immune system distraction, reactivate
the cellular machinery that leads to more rapid growth.
For women
who develop a single Pap smear showing mild dysplasia, there are
basically three approaches that are commonly followed:
-
Repeat Pap in 6 months. If the dysplasia
persists or worsens, further evaluation is undertaken. If the Pap
returns to normal, the woman is followed with more frequent Pap smears.
Ultimately, the frequency of Pap smear screening returns to normal, if
there is no further evidence of dysplasia. The primary advantage of this
approach is it limits the number of women needing colposcopy.
Particularly among adolescent women, most of these Pap abnormalities
will prove to be self-limited HPV infections. Repeating the Pap allows
for many of these cervices to heal, avoiding more extensive
intervention. The
primary disadvantages of the repeat Pap approach are that the majority of these women will
ultimately need colposcopy anyway and they have been subjected to
varying degrees of anxiety over known, but unresolved health issues.
-
Immediate Colposcopy. Some physicians feel that the cervix should be evaluated with colposcopy with even a single dysplastic
Pap smear. Their reasoning is that while many of the Pap smears (about
half) revert to normal in 6 months, the abnormality will often re-appear
at a later, less convenient time. They also reason that many women will
feel anxiety over simply observing the abnormality over time and not
investigating it right away. The primary disadvantage to this approach
is that even women with falsely positive Pap smears will undergo a
moderately costly evaluation.
-
See and Treat. Rather than colposcopic
evaluation and directed biopsies, followed by some form of treatment a
few days or weeks later, some physicians prefer to evaluate the cervix
with the colposcope, then immediately perform a LEEP procedure at the
same time, for those in whom the LEEP is appropriate. Their rationale is
that the combined see-and-treat is more cost-effective, it provides an
excellent specimen, and is typically highly effective treatment. Its
primary drawbacks are: It is a relatively costly procedure, requiring
more advanced skills and equipment not always available in all GYN
offices, and is overtreatment for most of those seen. For this reason,
many gynecologists reserve the see-and-treat approach for those whose
Pap smears show more advanced lesions.
One common method of treatment of mild dysplasia is cryosurgery (freezing the part of the
cervix containing the dysplastic cells and destroying those cells). Other approaches
include vaporizing the dysplastic cells with a laser, or shaving them off with an
electrified wire (LEEP). Sometimes, with very limited areas of dysplasia,
the process of biopsy of that area removes enough tissue that the
remaining dysplasia is sloughed off in the resulting eschar.
In years past, we would often treat everyone with mild
dysplasia vigorously to try to prevent progression to cancer. We had
good results in about 90% of those treated. Unfortunately, all of the
treatment modalities had about a 10% recurrence rate, not much different
than if we had not treated them at all.
If
not treated, about 10% of women who develop mild dysplasia, will
demonstrate a slow progression to moderate, then severe dysplasia, and ultimately develop
invasive cancer of the cervix. This process generally takes about 10
years, although occasionally it can progress much more rapidly. The
remaining 90% will either remain unchanged at mild dysplasia or regress back to
normal.
Currently, we usually just observe women
with mild dysplasia with frequent Paps (every 3-6 months) over the next
year or two, to discern those who will progress (the few) from those who
remain unchanged or regress (the many). Those showing signs of
advancement are then treated. This is based on the principles that:
-
Most cases of mild dysplasia regress.
-
Those that advance will do so slowly enough that we can
detect it.
-
Treatment of dysplasia earlier gives no better results
than treatment later.
-
While the risks associated with treatment are small,
they are not negligible, so it is better to reserve treatment for those
who really need it.
There are plenty of exceptions to this general approach.
Women whose access to medical care at a later time could be limited may
benefit from more aggressive treatment. Those whose dysplasia covers an
unusually wide area or whose lesion remains relatively inaccessible may
also need to be treated.
For women who have previously been evaluated with colposcopy and found to
have dysplasia, the appearance of mild dysplasia on a subsequent Pap smear is not
particularly alarming. Whether to re-colposcope them and the timing of such a
re-evaluation must be individualized, based on the patient's history,
risk factors, the degree of abnormality in the past and intervening Pap
smear results. |

Initial normal appearance of mild dysplasia

Mild Dysplasia after application of acetic acid
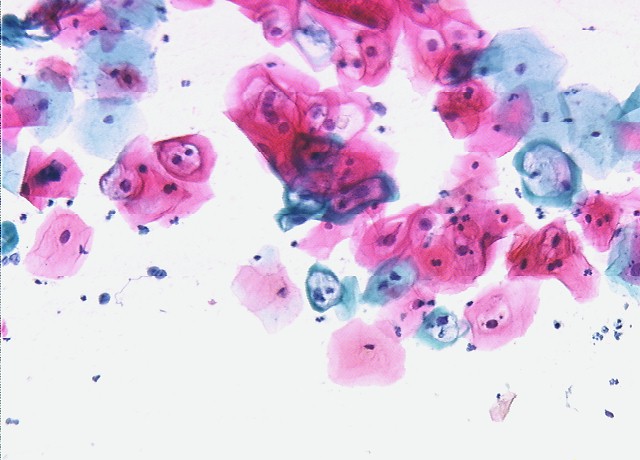
Mild Dysplasia

Cervix immediately after LEEP
|