Pelvic Examination
Evaluate the pelvis systematically.
Position the patient at the
very edge of the exam table, with her feet in stirrups, knees bent and
relaxed out to the side. If she is not down far enough, the exam will be
more difficult for you and more uncomfortable for her.
Pad the stirrups to avoid the
stirrups digging into her feet. Kitchen pot-holders work well for this,
but almost any soft material can be used.
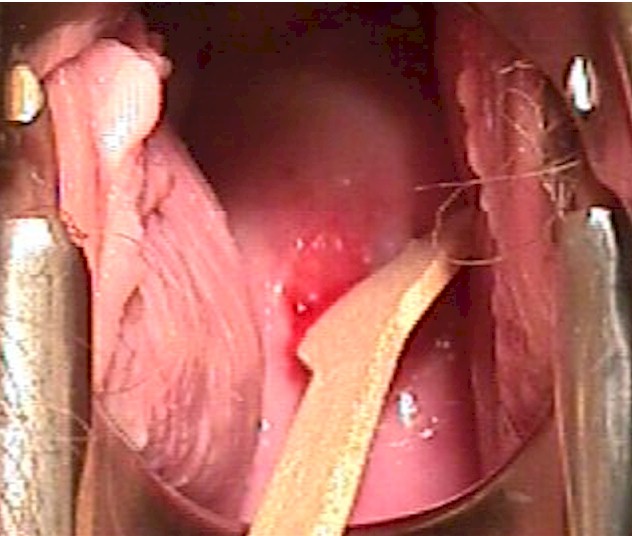
Use a bright light to visually
inspect the vulva, vagina and cervix. Most examiners find it easiest to
look just over the light to get the best view. Separate the labia with
your gloved fingers to look for any surface lesions, redness, or
swellings. Look within the pubic hair for the tiny movement of pubic
lice or nits. Look on the labia for the cauliflower-like bumps that are
known as venereal warts. Using magnification (magnifying lenses or
colposcope) is very useful when the patient has vulvar complaints and
the diagnosis is not obvious.
Look between the folds of skin
for ulcerative lesions that can indicate an active herpes infection.
Gently retract the clitoral hood back, exposing the clitoris while
looking for peri-clitoral lesions.
Look for the hymen or remnants
of the hymen and identify any redness just exterior to the hymen that
can indicate vulvar vestibulitis.
The periurethral glands
(Skene's glands) have tiny ducts that open onto the surface. Look for
them next to the urethra. While looking at the urethra, note any
discharge coming from the urethral opening that might suggest gonorrhea
or chlamydia.
Palpate the upper labia majora
for masses related to hernias extending through the Canal of Nuck.
Palpate the middle and lower portion of the labia majora for masses
suggesting a Bartholin Duct Cyst.
After warming a vaginal
speculum with warm water, separate the labia with one hand while gently
inserting the speculum with the other hand. It is frequently more
comfortable for the patient if you insert the speculum rotated about 45
degrees (so the blades are not horizontal but are oblique). Once past
the introitus, rotate the speculum back to it's normal position.
The labia, particularly the
labia minora, are very sensitive to stretching or pinching, so try not
to catch the labia minora in the speculum while inserting it.
Some gynecologists ask their
patients to "bear down" while they are inserting the speculum and feel
that this assists with insertion. Others find this instruction to be be
confusing and don't use it.
Obtain specimens for a
Pap smear and any cultures that may be indicated.
Then feel the pelvis by
application of a "bimanual exam."
For a normal examination:
-
External genitalia are of
normal appearance. There is no enlargement of the Bartholin or Skene
glands.
-
Urethra and bladder are
non-tender.
-
Vagina is clean, without
lesions or discharge
-
Cervix is smooth, without
lesions. Motion of the cervix causes no pain.
-
Uterus is normal size, shape,
and contour. It is non-tender.
-
The adnexa (tubes and
ovaries) are neither tender nor enlarged.
During the bimanual exam, you
may use one finger or two fingers inside the vagina. Two fingers allows
for deeper penetration and more control of the pelvic structures, but
one finger is more comfortable for the patient. You should individualize
your exam for the specific patient.
Turning your hand palm up,
compress the urethra against the underside of the pubic bone. Normally,
this doesn't hurt. If it causes discomfort for the patient, it is likely
that at least some degree of urethritis is present.
Then insert your fingers deeper
into the pelvis. Keeping your palm up, curl your vaginal finger(s) up,
compressing the bladder against the back of the pubic bone. Normally,
this pressure creates the sensation that the patient needs to urinate,
but is not painful. If it is painful, this is good clinical evidence of
cystitis (urinary tract infection), or (less likely) endometriosis.
In some patients, particularly
those with difficult to feel pelvic masses, a combined rectovaginal exam
is useful. Change gloves, lubricate the rectum, and then gently insert
your index finger into the vagina and your middle finger into the
rectum. The rectovaginal exam is helpful in feeling the uterosacral
ligaments, a common site of endometriosis involvement.
On completion of the rectal
exam, stool can be checked for the presence of occult blood.
If the hymen is intact, it may
still be possible to perform a comfortable and complete exam, but if the
exam is causing too much pain, stop the exam and consider these
alternatives:
-
Rectal exam with your index
finger can often provide all the information you need at that time.
-
Exam under anesthesia will
provide full access without causing pain to the patient.
-
Ultrasound scan, abdominally
and trans-perineal, can sometimes provide you with the information you
need.
|

Position the patient at the edge of the
exam table.

Inspect the vulva.

Warm and lubricate the speculum with warm
water.

Separating the labia with one hand,
insert a warmed, water-lubricated speculum with the other hand.
Obtain a Pap smear or cervical cultures,
if indicated.

Bimanual Exam
|