|
The opening of the uterus is
called the cervix.
While the cervix is considered a portion of the uterus, it is
functionally and histologically quite different. It is composed of dense
connective tissue, with very little smooth muscle. The body of the uterus,
in contrast, is primarily smooth muscle.
The cervix is located at the top of the vagina and is
easily visualized by inserting a vaginal speculum fully into the vagina and
opening the blades. The firm, smooth, pink structure appearing at the end of
the vagina is the cervix.
The cervix is of clinical significance because of:
-
The role it plays in pregnancy, remaining tightly closed for the bulk
of gestation, then, at just the right time, thinning and opening to allow
for birth of the baby.
-
It's vulnerability to cervical dysplasia and, by extension, cancer of
the cervix, and
-
The occasional patient who experiences symptoms of cervicitis,
primarily painful intercourse and vaginal discharge.
Nabothian Cysts
Two normal anatomic variations are responsible for considerable clinical
concern among the less experienced who examine women, Nabothian cysts
and cervical ectropion.
Nabothian cysts from when the secretions from
functional glandular epithelium become trapped below the surface of the
skin. This can occur because of the normal deep infolding of the
endocervical epithelium. It also may occur when the squamous exocervical
epithelium covers over the mucous-producing endocervical epithelium (squamous
metaplasia). It is seen more commonly after childbirth and sometimes
occurs concomitantly with cervicitis.
Clinically, Nabothian cysts are seen or felt as firm nodules on the
cervix. If close to the surface, they care clearly seen as cystic. If
the diagnosis is in doubt, puncturing them will release clear, mucoid
material. It is not necessary to do this, however, as the diagnosis is
rarely in doubt.
Sometimes, particularly if large, Nabothian cysts will be seen to
have a significant blood vessel or two coursing over the surface. These
are of no concern, though if tampered with, they may bleed.
Cervical Ectropion
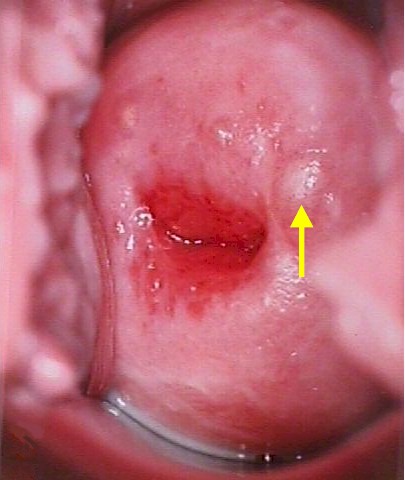
Inexperienced examiners are sometimes frightened to see a large, red,
somewhat friable lesion occupying the central portion of the cervix and
surrounding the cervix.
This is not a lesion...it is cervical
ectropion.
The red color is from the shallow, vascular, mucous-producing
endocervical epithelium which has grown out onto the face (exterior
portion) of the cervix. Over time, the ectropion may enlarge or
diminish in size, as the squamocolumnar junction changes its relative
position on the cervix. With pregnancy, the cervix tends to evert,
making the ectropion larger. In menopause, the SQJ tends to recede back
up the cervical canal, making the ectropion get progressively smaller
before disappearing completely. The fact that a cervical ectropion is
present is of no clinical concern. It needn't be treated and can safely
be ignored. If the ectropion is causing symptoms (eg., post-coital
bleeding), or in the presence of recurrent cervical infections (cervicitis),
then the ectropion can be treated by any means that safely eliminates
the most superficial layer of cells, facilitating the inward growth of
the surrounding squamous mucosa. Among these treatments are cryosurgery,
chemical cautery (AgNO3), electrocautery, thermal cautery, LEEP, and
laser ablation.
Cervicitis
Cervicitis means an infection of the cervix. This usually involves the
glandular elements (columnar epithelium) of the cervix and is usually
caused by organisms found in the vagina. Sometimes it is caused by such
sexually transmitted diseases as chlamydia or gonorrhea. Most cases of
cervicitis are unnoticed by the patient, but some notice painful
intercourse, persistent vaginal discharge, aching pelvic pain or
menstrual cramps.
The diagnosis can be confirmed by palpation of the
cervix. Normally, this doesn't hurt, but in the case of cervicitis,
compression or movement of the cervix causes some discomfort. When
clinically warranted, testing for STDs can be helpful before initiating
treatment. If found, they should be individually treated.
A simple course of oral antibiotics can be effective at resolving the
cervicitis, although if there is extensive cervical ectropion, the
cervicitis may return. For recurrent cervicitis, some form of cervical
ablation is usually needed, in addition to a short course of
antibiotics, to permanently resolve the problem.
 Cervical Cancer Cervical Cancer
Invasive cancer of the cervix is a relatively uncommon malignancy among
women, representing about 2% of all new cancers. This is in contrast to
the more common female cancers (breast 30%, lung 13%, colon 11%). It is
less common than uterine (6%). ovarian (4%), and bladder (3%) cancer.
Pap smear screening has had a dramatic impact on the incidence of
cervical cancer. Initially throught to promote early diagnosis of
cervical cancer, Pap screening has been most helpful in detecting the
pre-malignant changes that, when treated, are effective in preventing
the actual development of cervical cancer. Most cases of invasive
cervical cancer occur among women who have not been screened with Pap
smears or who have not had a Pap smear in many years.
Those at increased risk for cervical neoplasia include women with
multiple sexual partners, HPV infection (particularly the high risk HPV
types), cigarette smokers and those with impaired immune systems.
The most common symptom of cervical cancer is abnormal vaginal
bleeding, either spontaneous or provoked by intercourse or vigorous
physical activity. In advanced cases, some patient will notice back or
flank pain provoked by ureteral obstruction and hydronephrosis.
The diagnosis is usually confirmed by biopsy, but is suspected if a
friable, visible, exophytic lesion is seen on the cervix. Endophytic
lesions tend to invade deeply into the cervical stroma, creating an
enlarged, firm, barrel-shaped cervix. Initial metastases are to the
parametrial tissues and lymph nodes. Later, in addition to aggressive
local spread into the upper vagina, rectum and bladder, hematogenous
spread to the liver, lungs, and bone occurs.
Following diagnosis of cervical cancer, staging of the cancer is
performed to assist in selecting the best treatment. Stages (0-IV) are
defined by the International Federation of Gynecology and Obstetrics,
and include:
|
Stage |
Extent of Disease |
5-Year Survival Rates |
|
0 |
Carcinoma in situ, limited to
the epithelium, without invasion |
>99% |
|
I |
Cancer limited to the cervix |
70%-99% |
|
II |
Cancer extends beyond the
cervix, but not to the pelvic sidewall, and not to the lower third
of the vagina |
60% |
|
III |
Cancer extends to the pelvic
sidewalls and/or to the lower third of the vagina. |
45% |
|
IV |
Cancer extends beyond the true
pelvis, or extends into the bladder or bowel mucosa. |
18% |
In addition, there are subcategories within each stage.
Treatment can consist of surgery, radiation therapy, and sometimes
adjuvant therapy. The best option for treatment depends on the stage of
the cancer. Surgery seems to work best on Stages I and IIA (no obvious
parametrial involvement). Radiotherapy seems to work better for more
advanced stages. Complications of either approach include bladder and
bowel fistula formation, and loss of vaginal length. |

Cervix viewed through a
vaginal speculum
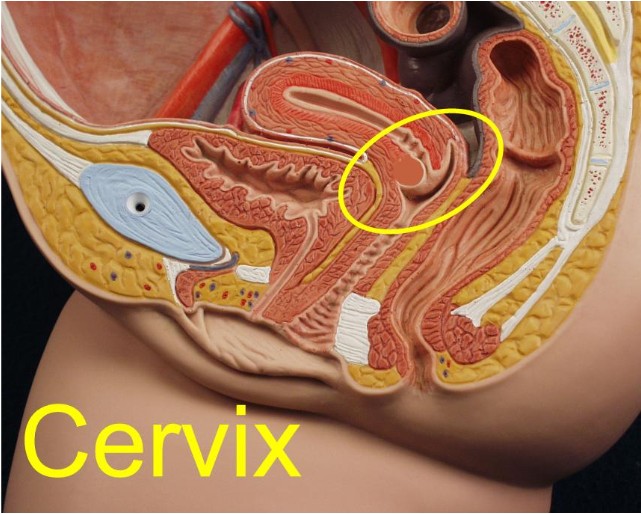
Side view of the cervix
Nabothian Cyst

Cervical Ectropion

Cervicitis
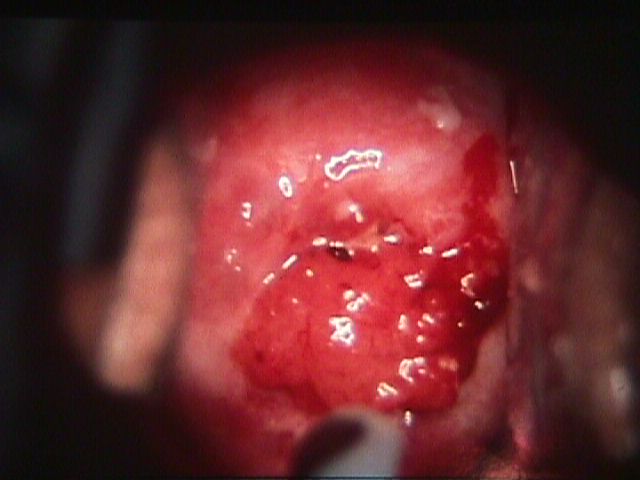
Invasive Squamous Cell Cancer |