|
Lesson 6: Introduction to Physical Assessment
An accurate physical assessment requires an organized and systematic approach using the techniques of inspection, palpation, percussion, and auscultation. It also requires a trusting relationship and rapport between the nurse and the patient to decrease the stress the patient may have from being physically exposed and vulnerable. The patient will be much more relaxed and cooperative if you explain what will be done and the reason for doing it. While the findings of a nursing assessment do sometimes contribute to the identification of a medical diagnosis, the unique focus of a nursing assessment is on the patient's responses to actual or potential problems.
6-2. FACTS ABOUT PHYSICAL ASSESSMENT
a. Physical assessment is an organized systemic process of collecting objective data based upon a health history and head-to-toe or general systems examination. A physical assessment should be adjusted to the patient, based on his needs. It can be a complete physical assessment, an assessment of a body system, or an assessment of a body part.
b. The physical assessment is the first step in the nursing process. It provides the foundation for the nursing care plan in which your observations play an integral part in the assessment, intervention, and evaluation phases.
c. The chances of overlooking important data are greatly reduced because the physical assessment is performed in an organized, systematic manner, instead of a random manner.
6-3. PURPOSES OF A PHYSICAL ASSESSMENT
a. A comprehensive patient assessment yields both subjective and objective findings. Subjective findings are obtained from the health history and body systems review. Objective findings are collected from the physical examination.
(1) Subjective data are apparent only to the person affected and can be described or verified only by that person. Pain, itching, and worrying are examples of subjective data.
(2) Objective data are detectable by an observer or can be tested by using an accepted standard. A blood pressure reading, discoloration of the skin, and seeing the patient in the act of crying are examples of objective data.
(3) Objective data are sometimes called signs, and subjective data are sometimes called symptoms.
(4) Data means more than signs or symptoms; it also includes demographics, or patient information that is not related to a disease process.
b. The purposes for a physical assessment are:
(1) To obtain baseline physical and mental data on the patient.
(2) To supplement, confirm, or question data obtained in the nursing history.
(3) To obtain data that will help the nurse establish nursing diagnoses and plan patient care.
(4) To evaluate the appropriateness of the nursing interventions in resolving the patient's identified pathophysiology problems.
6-4. CONSIDERATIONS IN PREPARING A PATIENT FOR A PHYSICAL ASSESSMENT
a. Establish a Positive Nurse/Patient Rapport. This relationship will decrease the stress the patient may have in anticipation of what is about to be done to him.
b. Explain the Purpose for the Physical Assessment. The purpose of the nursing assessment is to gather information about the patient's health so that you can plan individualized care for that patient. All other steps in the nursing process depend on the collection of relevant, descriptive data. The data must be factual, not interpretive.
c. Obtain an Informed, Verbal Consent for the Assessment. The chief source of data is usually the patient unless the patient is too ill, too young, or too confused to communicate clearly. Patients often appreciate detailed concern for their problems and may even enjoy the attention they receive.
d. Ensure Confidentiality of All Data. If possible, choose a private place where others cannot overhear or see the patient. Explain what information is needed and how it will be used. It is also important to convey where the data will be recorded and who will see it. In some situations, you should explain to the patient his rights to privileged communication with health care providers.
e. Provide Privacy From Unnecessary Exposure. Assure as much privacy as possible by using drapes appropriately and closing doors.
f. Communicate Special Instructions to the Patient. As you proceed with the examination, inform the patient of what you intend to do and how he can help, especially when you anticipate possible embarrassment or discomfort.
6-5. BASIC TECHNIQUES USED IN PERFORMING A PHYSICAL ASSESSMENT
a. Inspection. Visual examination of a person is called inspection. This is done in an orderly manner, focusing on one area of the body at a time.
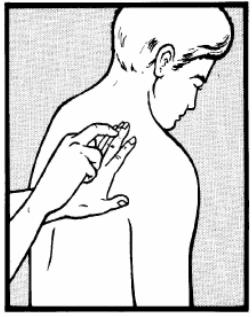
b. Palpation. Examination by touch is called palpation (figure 6-1). The nurses feels for texture, size, consistency, and location of body parts.
c. Auscultation. Examination by listening for sounds produced within the body is called auscultation. The sounds most frequently listened for are those of the abdominal and thoracic viscera and the movement of blood in the cardiovascular system. Direct auscultation, using the ear only, is seldom done. Indirect auscultation is generally carried out with a stethoscope.
d. Percussion. Examination of the body by tapping it with the fingers is called percussion (figure 6-2). Percussion is a special assessment skill that the practical nurse is not required to perform. This technique is usually performed by a registered nurse (RN) or a physician.
6-6. AREAS OF GENERAL APPEARANCE AND BEHAVIORAL ASSESSMENT
a. Demographic Data. You begin the assessment by collecting personal information, which includes name, age, sex, marital status, race, and religion. This identifies the patient and provides important demographic data.
b. Body Build. Observe the patient's general appearance and health state in relation to his age and lifestyle. Determine the patient's height, weight, and vital signs at this time.
c. Posture and Gait. Observe whether the patient is erect or slouched, steady or unsteady. Posture can indicate mood. For example, a slumped position may reflect depression; too rigid and upright a position may indicate anxiety.
d. Hygiene and Grooming. Look for cleanliness of nails, hair, skin, and overall appearance. Usually, you can assess these gradually while observing other parts of the body for data. Observe the skin for color, texture, temperature, and lesions. Lesions warrant particular attention during assessment. Some primary skin lesions are:
(1) Nodule--a solid mass extending into the dermis.
(2) Tumor--a solid mass larger than a nodule.
(3) Cyst--an encapsulated fluid-filled mass in the dermis or subcutaneous layer.
(4) Wheal--a relatively reddened, flat, localized collection of fluid. An example is hives.
(5) Vesicle--circumscribed elevation containing serous fluid or blood. An example is chickenpox.
(6) Bulla-- large fluid-filled vesicle. An example is a second-degree burn.
(7) Pustule--a vesicle or bulla filled with pus. An example is acne. e. Dress. Observe the patient's clothing in relation to age, climate, socioeconomic status, and culture. Notice whether the clothing is clean, properly buttoned, or zipped. The patient's dress may reflect the cold intolerance of hypothyroidism. Slippers or untied shoelaces suggest edema.
f. Body and Breath Odors. Malodorous body or breath may indicate pulmonary infections, uremia, or liver failure. A breath odor of acetone may be due to diabetes. Although odors give important clues, avoid the common mistake of assuming that alcohol on a patient's breath explains neurologic or mental status findings. Alcoholic breath does not necessarily mean alcoholism.
g. Attitude. The patient's attitude is reflected in his appearance, speech, and behavior. The patient may be aloof and unwilling to participate in the interview. He may verbalize anger or fear. Some patients have a "take care of me" attitude and expect nurses and other health care personnel to magically know everything about them. Such findings should be noted as part of your general impression.
h. Affect/Mood. Affect is the emotional state as it appears to others. Mood is the emotional state as described by the patient. Observe the patient's facial expression. No part of the body is as expressive as the face. Feelings of joy, sadness, fear, surprise, anger, and disgust are conveyed by facial expression. Facial expressions generally are not consciously controlled.
i. Speech. Assess the patient's speech for loudness, clarity, pace, and coherence. Observe the patient for poor articulation of words and language difficulty. Patients who are not fluent in English or have limited education are sometimes mistakenly labeled as "indifferent" or "noncommunicative."