Gynecologic Ultrasound
Scan
Technique
This scan can be done abdominally, transvaginally, or both. The abdominal scan
tends to give a larger field of view, but less detail, particularly for
structures deep in the pelvis and partially hidden by the pubic symphysis. If
scanning abdominally, a full bladder is helpful as sound transmits well through
water. In this case, the full bladder serves as an acoustic "window"
into the pelvis. The full bladder also helps raise pelvic structures up from
behind the symphysis and into view. If scanning transvaginally, a full bladder
makes the scan more difficult because it pushes the uterus, tubes and ovaries
further away from the vaginal transducer.
While performing the scan, you may use the vaginal probe as though it were
your examining fingers, putting pressure on different structures to see if they
are tender or fixed in place. Similarly, you may use your other had abdominally
to press down, bringing structures closer to the vaginal probe. This type of
dynamic ultrasound scanning may provide information you might otherwise miss.
Ultrasound Adjustments
When performing this type of scan, adjusting various settings for the equipment
can have a significant effect on improving the images and clarifying
detail.
- Increasing to higher ultrasound frequency will give better resolution, but
poorer depth of penetration. In the obese patient, depth of penetration is
very important and resolution may need to be sacrificed somewhat in order to
see all of the structures.
- Increasing the gain (amplification) will bring out more echoes on the
screen, particularly at the lower end of the image, but increasing the gain
results in more artifact. Decreasing the gain will clear up some of the
artifact (particularly in cystic masses), but with some loss of signal,
particularly deep in the tissues.
- Focal distances can be varied. Set the focus just below the deepest
structure you wish to see clearly.
- Field of view can be widened or narrowed. The narrower the field of view,
generally the better the image quality within the field.
The Normal Uterus
Start by visualizing the uterus in its long axis. You should see the
endocervical canal connecting to the endometrial stripe.
Measure the uterus in three dimensions, total length, width and depth.
Sweep through the uterus both lengthwise and transversely, evaluating
the myometrium for the presence of fibroids. Small cystic masses in the cervix
are Nabothian cysts and are of no clinical significance.
Endometrium
The endometrial lining, or "stripe," varies in thickness and texture with the
menstrual cycyle.
Uterine Abnormalities
Fibroid tumors are the most common uterine abnormality seen with ultrasound.
These round masses are seen within the myometrium or projecting out from the
myometrium.
Normal Ovaries
Normal ovaries appear lateral to the uterus and vary in their relative
position within the pelvis. In this example, the ovary lies in the classical
position just above the vessels. In other cases, the ovaries may be quite remote
from this location.
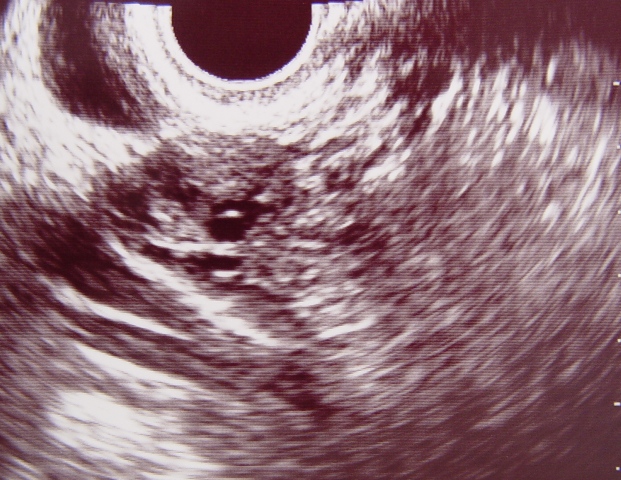
Normal Ovary |
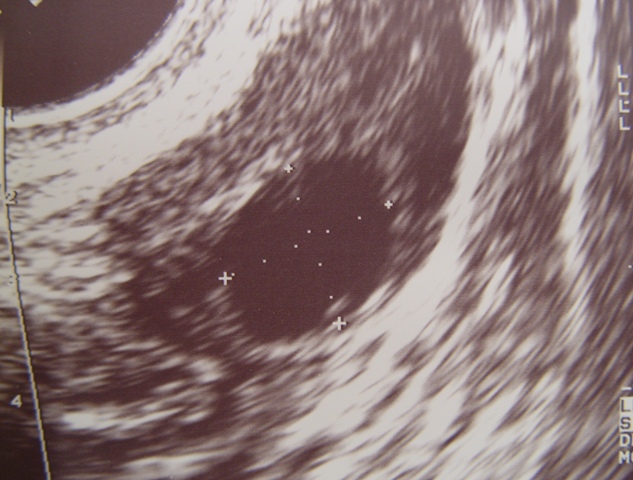
Normal Ovarian Follicle |
During childbearing years, the ovaries are usually readily identified by the
presence of small ovarian follicles. As the menstrual cycle advances, several
ovarian follicles are recruited and grow to 8-12 mm in diameter. Then, one
dominant follicle is usually selected which continues to grow at 2-4 mm/day,
until it reaches about 25 mm (22-30). It then releases the egg and partially
collapses, forming a corpus luteum.
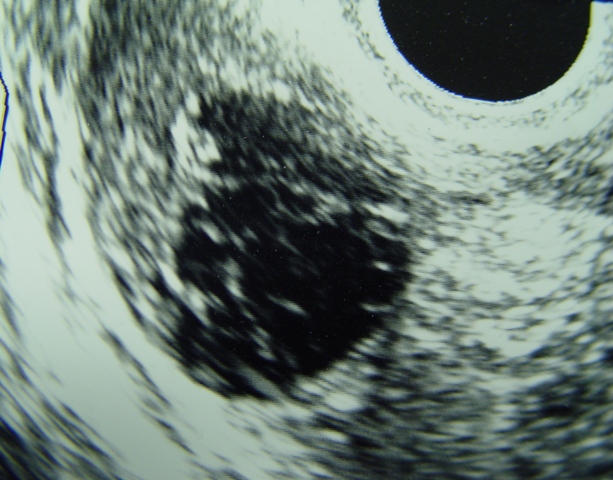
Hemorrhagic Corpus Luteum Cyst |
If there is any internal bleeding into the cyst cavity, the corpus luteum
takes on an irregular, "cob-web" appearance that promptly resolves. This is
known as a hemorrhage corpus luteum cyst and is innocent, though it has a
somewhat disturbing ultrasound appearance.
At menopause, the ovarian follicles no longer grow and the ovary may become
difficult to identify.
Similar findings can be seen among long-term oral contraceptive pill users,
although the changes are generally not as dramatic.
Ovarian Abnormalties
A large number of ovarian abnormalities can be seen, among them cysts, solid
tumors, and endometriomas.
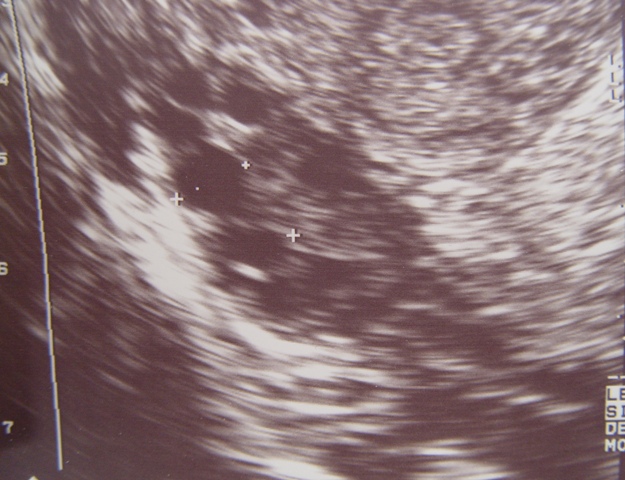
Polycystic Ovary |
|
